CHAPTER 43 Brain Abscess
Brain abscess is defined as a focal intracranial infection that is initiated as an area of cerebritis and evolves into a collection of pus surrounded by a vascularized capsule.1 Given their location, the approach to brain abscesses often presents diagnostic and therapeutic challenges. The following sections review the epidemiology, pathogenesis, etiology, and diagnostic and management approach for this devastating infection.
Epidemiology
Incidence and Risk Factors
Before the advent of infection with human immunodeficiency virus (HIV), brain abscess was not common, with an incidence of 0.3 to 1.3 cases per 100,000 persons per year in the United States.2 This translates to approximately 1500 to 2500 cases per year in the United States, with a higher incidence in developing countries.3 There is a male preponderance of 2 : 1 to 3 : 1, and the median age at infection is between 30 and 40 years.2,4 Differences in age are based on the primary site of infection—when the abscess is from an otitic focus, patients are generally younger than 20 years or older than 40 years, and when secondary to a focus in the paranasal sinuses, most patients are between 30 and 40 years of age. About 25% of brain abscess cases occur in children, mostly secondary to an otitic focus or in those with congenital heart disease; in one review from the University of Virginia Children’s Hospital from 2000 to 2007, an average of only 1.5 children per year were admitted to the inpatient pediatric service with a primary diagnosis of brain abscess.5 Brain abscess may occur after cranial operations. It was reported in only 0.2% of 1587 operations in one study6 and in 10 of 16,540 cranial surgeries performed by 25 neurosurgeons in another review7; although rare, a small percentage of patients will require a repeat operation to treat the infection. In more recent series, brain abscess is more commonly reported in patients who are immunocompromised,2,3 including those infected with HIV, receiving chemotherapy for cancer, receiving immunosuppressive therapy after organ transplantation, or after prolonged use of corticosteroids.
Pathogenesis
Organisms can reach the central nervous system (CNS) by spread from a contiguous source of infection (25% to 50% of cases), hematogenous dissemination (20% to 35% of cases), or trauma1–5,8–16; brain abscess is cryptogenic in about 10% to 35% of patients.2,17 Sources from a contiguous focus of infection include infections in the middle ear, mastoid cells, or paranasal sinuses. Brain abscess that results from otitis media usually localizes to the temporal lobe or cerebellum; in one review, 54% were in the temporal lobe, 44% in the cerebellum, and 2% in both locations.18 Recent series, however, have demonstrated that cases of brain abscess secondary to otitis media have been decreasing, although intracranial complications may be increased in patients in whom appropriate treatment of otitis media is neglected. In patients with brain abscess secondary to paranasal sinusitis, the frontal lobe is the predominant site. When the abscess is a complication of sphenoid sinusitis, the temporal lobe or sella turcica is usually involved. Dental infections, particularly of the molar teeth, can lead to brain abscess, often in the frontal lobe, but temporal lobe extension has been reported.19,20
Hematogenous dissemination to the brain generally leads to multiple, multiloculated abscesses, which are associated with higher mortality than abscesses that result from contiguous foci of infection.2–4 The most common sources in adults are chronic pyogenic lung diseases (especially lung abscess), bronchiectasis, empyema, and cystic fibrosis. Other distant sources of infection include wound and skin infections, osteomyelitis, pelvic infections, and intra-abdominal infections; they can also occur after esophageal dilation or sclerosing therapy for esophageal varices.21–23 Cyanotic congenital heart disease (especially in patients with tetralogy of Fallot and transposition of the great vessels) is another predisposing factor that accounts for 5% to 15% of brain abscess cases. Even higher percentages are reported in pediatric series,24,25 although advances in cardiovascular surgery have led to a decrease in patients with cyanotic congenital heart disease as a predisposing factor.3 Brain abscess occurs in less than 5% of patients with infective endocarditis despite the presence of continuous bacteremia.26–28 There is also a significant likelihood of brain abscess in patients with hereditary hemorrhagic telangiectasia, which is almost always observed in those with coexisting pulmonary arteriovenous malformations, perhaps by allowing septic emboli to cross the pulmonary circulation without capillary filtration29–32; the risk ranges from 5% to 9% and is 1000 times greater than in the general population.
Trauma can lead to brain abscess formation as a result of an open cranial fracture with dural breach or foreign body injury or as a sequela of neurosurgery.33 The incidence of traumatic brain abscess in the civilian population ranges from 2.5% to 10.9%, and reports have included brain abscess secondary to compound depressed skull fractures, dog bites, rooster pecking, tongue piercing, and injuries from lawn darts and pencil tips.34–36 Nosocomial brain abscess has been seen after halo pin insertion,37 after electrode insertion to localize seizure foci,38 and in malignant glioma patients treated by placement of Gliadel wafers in the tumor bed to release carmustine.39 In military populations, the incidence of brain abscess after head trauma ranges from 3% to 17%, and they usually occur secondary to retained bone fragments or contamination of initially uninfected missile sites with bacteria from skin, clothes, or the environment.40 However, the importance of retained bone fragments in the pathogenesis of infection has been questioned. In a study from Croatia of 160 war missile penetrating craniocerebral injuries in which 21 skull base injuries were treated surgically,41 only the accessible retained bone or metallic fragments were removed; the retained foreign bodies did not seem to increase the infection rate except in patients who suffered an in-driven cluster of bone fragments or leakage of cerebrospinal fluid. These findings were confirmed in another retrospective study from Croatia in which 88 patients with brain missile wounds had only accessible bone or metallic fragments removed during intracranial débridement42; there were 9 cases of brain abscess and the presence of retained fragments was not responsible for an increased rate of infection. Similar results were found in another study of 43 patients who survived low-velocity missile injuries to the brain during military conflicts and had retained fragments; suppurative sequelae were seen in 6 patients and only 2 progressed to brain abscess.43
Etiology
Numerous infectious agents have been reported to cause brain abscess. The probable infecting pathogen depends on the pathogenesis of the infection (see earlier) and the presence of various predisposing conditions (Table 43-1). This chapter focuses on important bacterial and fungal causes of brain abscess. Protozoal and helminthic causes (e.g., Trypanosoma cruzi, Taenia solium, Entamoeba histolytica, Schistosoma spp., Microsporidia spp., and Paragonimus spp.) are discussed in other chapters of this book. The most important protozoal cause of brain infection is Toxoplasma gondii, which is seen primarily in patients infected with HIV; this organism and the approach to CNS mass lesions in patients infected with HIV are also discussed in other chapters of this book.
TABLE 43-1 Predisposing Conditions and Probable Etiologic Agents in Brain Abscess
| PREDISPOSING CONDITION | POSSIBLE MICROBIAL CAUSES |
|---|---|
| Otitis media or mastoiditis | Streptococci (aerobic or anaerobic), Bacteroides spp., Prevotella spp., Enterobacteriaceae |
| Sinusitis (frontoethmoidal or sphenoidal) | Streptococci, Bacteroides spp., Enterobacteriaceae, Haemophilus spp., Staphylococcus aureus |
| Dental infection | Mixed Fusobacterium, Prevotella, Actinomyces, and Bacteroides spp.; streptococci |
| Penetrating trauma or secondary to neurosurgical procedure | Staphylococcus aureus, Enterobacteriaceae, Clostridium spp. |
| Lung abscess, empyema, or bronchiectasis | Fusobacterium, Actinomyces, Bacteroides, and Prevotella spp.; streptococci; Nocardia spp. |
| Bacterial endocarditis | Staphylococcus aureus, streptococci |
| Congenital heart disease | Streptococci, Haemophilus spp. |
| Immunocompromised state | |
| Neutropenia | Aerobic gram-negative bacilli, Aspergillus spp., Mucorales, Candida spp., Scedosporium spp. |
| Transplantation | Enterobacteriaceae, Listeria monocytogenes, Nocardia spp., Aspergillus spp., Candida spp., Mucorales, Scedosporium spp., Toxoplasma gondii |
| HIV infection | Listeria monocytogenes, Nocardia spp., Mycobacterium spp., Cryptococcus neoformans, Toxoplasma gondii |
Bacteria
The most common bacterial causes of brain abscess are streptococci (aerobic, anaerobic, and microaerophilic), which are isolated in up to 70% of cases.2,10,44 They include organisms in the Streptococcus anginosus (milleri) group, which normally reside in the oral cavity, appendix, and female genital tract. Staphylococcus aureus is isolated in 10% to 20% of cases, most commonly after cranial trauma or infective endocarditis.2 Enteric gram-negative bacilli (e.g., Proteus spp., Escherichia coli, Klebsiella spp., Pseudomonas aeruginosa, and Enterobacter spp.) are isolated in 23% to 33% of patients; predisposing factors include otitis media, bacteremia, neurosurgical procedures, and the immunocompromised state.2,45,46 Anaerobes (especially Bacteroides and Prevotella spp.) have more often been isolated after proper culture techniques and are found in 20% to 40% of patients, frequently in mixed culture.2,47,48 Multiple organisms are cultured in 14% to 28% of those with positive culture results.2,9–12 The incidence of negative cultures has ranged from 0% to 43%2,3,9–13,15,18,47,49; previous use of antimicrobial therapy may account for these negative culture results.
Other species are less commonly isolated in patients with bacterial brain abscess but should be considered in those with certain underlying conditions. For example, brain abscess caused by Listeria monocytogenes is uncommon (<1% of cases) but accounts for about 10% of cases of CNS listeriosis50,51; Listeria should be considered in patients who are immunocompromised (e.g., leukemia, lymphoma, HIV infection, and conditions requiring corticosteroids or other agents that cause immunosuppression). Salmonella species may cause brain abscess in patients who are bacteremic or in the presence of some compromise of the reticuloendothelial system.52 Brain abscess caused by Nocardia species may occur as part of a disseminated infection in patients with cutaneous or pulmonary disease; most have defects in cell-mediated immunity such as corticosteroid therapy, organ transplantation, HIV infection, or neoplasia.53,54 Rare cases of Nocardia brain abscess have also been seen in pregnant women. Other bacteria that cause brain abscess include Streptococcus pneumoniae, Haemophilus influenzae, Burkholderia pseudomallei, and Actinomyces species.2,16,55,56 When meningitis is caused by certain facultative gram-negative organisms (e.g., Citrobacter diversus), concomitant brain abscess is observed in more than 75% of cases.1,57,58 Mycobacterium tuberculosis and nontuberculous mycobacteria have increasingly been observed to cause brain abscess,1,2,59 with most cases reported in patients with HIV infection60,61; when the caseous core of a CNS tuberculoma liquefies, a tubercular abscess will result.62
Fungi
In recent years, the incidence of fungal brain abscess has been rising as a result of the increased use of corticosteroid therapy, broad-spectrum antimicrobial therapy, and immunosuppressive agents.63–66 Candida species have been the most prevalent fungi but are often not discovered until autopsy; these fungi cause microabscesses, macroabscesses, noncaseating granulomas, and diffuse glial nodules. Risk factors for candidal brain abscess include the use of broad-spectrum antimicrobial agents, corticosteroids, and hyperalimentation; premature birth; malignancy; neutropenia; chronic granulomatous disease; diabetes mellitus; thermal injury; and the presence of a central venous catheter.
CNS aspergillosis is reported in 10% to 20% of patients with invasive disease.63,65,67,68 The lungs are the usual primary site of infection, with dissemination to the CNS occurring by direct extension from an area that is anatomically adjacent to the brain. The most important underlying immune defect in patients with invasive aspergillosis is neutropenia (i.e., in those who have an underlying malignancy), but it may also be seen in patients with hepatic disease, diabetes mellitus, chronic granulomatous disease, Cushing’s syndrome, HIV infection, injection drug use, organ transplantation, and bone marrow transplantation, as well as after craniotomy and in patients receiving chronic corticosteroid therapy.
CNS infections caused by the Mucorales group are among the most fulminant infections known. Diabetes mellitus, usually associated with acidosis, is the most common predisposing condition (≈70% of cases), but disease may also be seen in patients with acidemia from profound systemic illness (e.g., sepsis, severe dehydration, severe diarrhea, chronic kidney disease), hematologic neoplasms, renal transplantation, injection drug use, and use of deferoxamine.65,69 CNS disease results from direct extension from the rhinocerebral form, after open head trauma, or after hematogenous dissemination. Bilateral involvement of the basal ganglia has been reported in injection drug users. Rhizopus arrhizus is the most common isolate.70
Scedosporium species may cause CNS disease in immunocompetent and immunocompromised hosts.65,71–75 These organisms may enter the CNS by direct trauma, hematogenous dissemination, or direct extension from infected sinuses. An association between near-drowning and subsequent CNS infection has been reported because these organisms are present in contaminated water and manure.
Many other fungal species have been reported to cause brain abscess, including Cryptococcus neoformans, the endemic mycoses (Coccidioides spp., Histoplasma spp., and Blastomyces dermatitidis), and many of the dematiaceous fungi. It is beyond the scope of this chapter to review all fungal causes of brain abscess, and more detail can be found from other sources.65
Experimental Models of Infection
Numerous animal models have been developed to study the pathogenesis and pathophysiology of brain abscess.76 Some large-animal models were created by direct implantation of bacteria into the brain; however, these models were limited by lack of reproducibility, they required multiple steps and an agar vehicle to initiate infection, and they were quite expensive. Another method used embolization of contaminated pliable cylinders implanted into the carotid artery but required concomitant cerebral injury for abscess formation, and the accompanying brain infarction caused a high mortality rate even in uninfected control animals.
A better animal model involved the use of mice or rats and consisted of a simple, one-step, easily reproducible procedure for consistent production of brain abscess. Infection was produced by the injection of 1 µL of saline containing a fixed inoculum of bacteria through a bur hole and into the frontal lobe of the brain.77,78 With this model, brain abscess was achieved in a one-step process at a specific site with the injection of bacteria alone, the inoculum could be regulated in terms of both volume and number of organisms, the number of injected bacteria and the number of bacteria that remain viable in the tissue could be quantified at a later time, and there was precise control of the injection site, thereby reducing tissue trauma with minimal (or no) infection in the subarachnoid space. This model also simulated human infection in that the abscess was produced in the white matter at the white and gray matter junction and migrated toward the ventricle, a shift in intracranial contents occurred, and there was minimal histologic evidence of meningitis; the abscess capsule was asymmetric by being more complete on the cortical than on the ventricular side, perhaps because the increased vascularity of normal cortical gray matter allowed greater fibroblast proliferation and collagen helix formation. In addition, development of the abscess paralleled clinical disease with the initial development of cerebritis and massive white matter edema followed by encapsulation.
In another animal model, brain abscess was produced in a rat by direct intracerebral injection of agarose beads laden with S. aureus.79 This method was also easy, reproducible, effective, and associated with a low mortality rate, and the histologic features of these experimental abscesses were similar to those observed in other animal models and in humans. These models have been useful in delineating the early events in brain abscess formation with respect to bacterial virulence factors and the host defense mechanisms involved in brain abscess formation; these concepts are reviewed in greater detail subsequently.
Initiation of Infection
The brain appears to be significantly more sensitive to infection than many other tissues. In a rat model of experimental brain abscess, injection of 104 colony-forming units (CFUs) of S. aureus or 106 CFUs of E. coli failed to cause infection in the skin, but abscess formation in brain tissue was induced by a level as low as 102 CFUs of either organism.80 The brain may also be more susceptible to infection by different organisms; in the experimental rat model, strains of E. coli were more virulent (i.e., led to abscess formation at lower inocula) than P. aeruginosa, S. aureus, or Streptococcus pyogenes.81 In addition, E. coli strains possessing the K1 antigen were more infective than strains without this antigen, thus indicating that certain encapsulated strains may be more virulent in brain abscess formation. Furthermore, inoculation of Bacteroides fragilis or streptococci such as S. intermedius failed to lead to abscess formation in rats even though these organisms account for a high percentage of isolates from brain abscesses in humans; this may be explained by the fact that brain abscess is often the result of a contiguous focus of infection and the synergistic infectivity of mixed populations of anaerobes plus a facultative organism may be necessary to establish infection.82,83 In an experimental dog model of brain abscess formation, inoculation of B. fragilis with Staphylococcus epidermidis in mixed culture caused a virulent reaction,84 although each organism was not tested separately. The role of other bacterial virulence factors in the pathogenesis of brain abscess formation has not been elucidated. However, the role of virulence factor production in the development of brain abscess was demonstrated by the inability of heat-inactivated S. aureus to induce proinflammatory cytokine or chemokine expression in an experimental mouse model; alpha toxin was identified as a key virulence factor for survival of S. aureus in the brain and subsequent development of brain abscess.85
Brain abscess may also develop in patients with bacterial meningitis, a rare complication except in human neonates with meningitis caused by C. diversus.45,46 Pathologically, there is cerebral necrosis and liquefaction, along with vasculitis of small vessels and hemorrhagic necrosis of adjacent tissue with a propensity for contiguous inflammation in the cerebral white matter, which may reflect the effects of endotoxin in the small penetrating vessels in this area; the typical abscess with capsule formation was not present. The pathogenesis was investigated in an infant rat model in which infection was initiated with the production of a high-grade bacteremia, infiltration of the leptomeninges, and subsequent development of ventriculitis.86 Brain abscesses were found exclusively in the periventricular white matter, apparently from disruption of the ventricular ependymal lining with direct extension of the infection into the parenchyma. The virulence factors responsible for the propensity of this organism to cause brain abscess are undefined, although a minor 32-kD outer membrane determinant may be a marker for strains that are more likely to produce ventriculitis and brain abscess87; strains that lacked the 32-kD outer membrane protein caused more bacteremia, meningitis, and death.
Stages of Infection
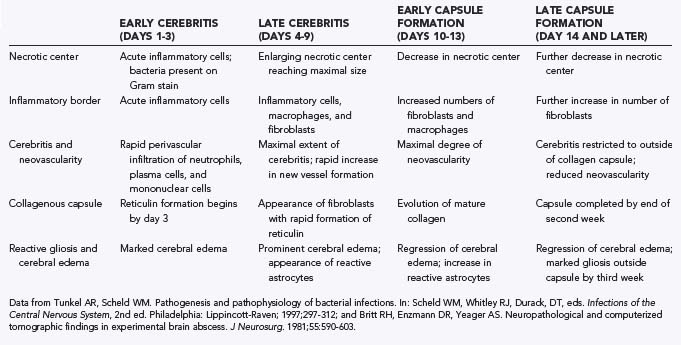
The temporal course and pathologic consequences of brain abscess were examined in a canine model of infection after inoculation of α-hemolytic streptococci. Four stages of infection were identified (Table 43-2): early cerebritis, late cerebritis, early capsule formation, and late capsule formation.88 These stages are somewhat arbitrary but are useful in the classification and comparison of virulence between different organisms in the production of brain abscess. Similar neuropathologic findings were described in an experimental model of anaerobic brain abscess,84 but capsule formation could not be divided into early and late stages because of delayed encapsulation. S. aureus was found to be more virulent than α-hemolytic streptococci, with a greater amount of necrosis and total area of involvement and a longer course of progression to resolution, time to reach a stable size, and time to contain the necrotic region within a collagenous capsule.89 Inflammation with histologic evidence of extension of inflammation, necrosis, and edema beyond the capsule was also observed, similar to findings after inoculation with B. fragilis. In all these studies, capsule formation was less prominent on the ventricular than on the cortical surface,84,88,89 perhaps because differences in vascularity between the cortical gray and white matter allow greater fibroblast proliferation, which probably explains the tendency for brain abscesses to rupture into the ventricular system rather than into the subarachnoid space. In contrast, the histopathologic sequence of brain abscess formation was examined in an experimental rat model after inoculation of E. coli90; the histopathologic findings supported an alternative hypothesis that brain abscesses tend to rupture intraventricularly because the infectious process is directed along the major white matter tracts (areas of lower tissue resistance) rather than as a result of asymmetric collagen deposition. However, the question of rupture of brain abscess requires further study.
Host Defense Mechanisms
In the experimental models just described, bacteria were inoculated directly into the brain, thus bypassing the brain’s normal host defense mechanisms. Although the brain is generally protected from infection by an intact blood-brain barrier, once infection is established, immune defenses are usually inadequate to control the infection. Local opsonization in the brain is deficient, which allows encapsulated bacteria such as B. fragilis and E. coli to escape efficient phagocytosis; phagocytosis of Bacteroides species also requires heat-labile serum factors such as complement and lysozyme, and these factors are probably absent in the CNS.91,92 The outer membrane components of Bacteroides species may also be important in the inhibition of neutrophil chemotaxis, thereby reducing the host response to brain abscess caused by this organism.93
As shown in Table 43-2, the border around the initial area of inoculation is composed of acute inflammatory cells during the early cerebritis stage, accompanied by the rapid development of a perivascular infiltrate consisting of neutrophils, plasma cells, and mononuclear cells.84,88,89 In an experimental rat model of brain abscess formation, production of the proinflammatory cytokines interleukin-1α (IL-1α), IL-1β, IL-6, and tumor necrosis factor-α (TNF-α) occurred as early as 1 to 6 hours after exposure to S. aureus.94 This was followed by enhanced concentration of the CXC chemokine KC, which correlates with the appearance of neutrophils in the abscess. The importance of neutrophils in the initial containment of S. aureus in the brain was established by the fact that mice transiently depleted of neutrophils, before the implantation of bacteria-laden beads, had higher CNS bacterial burdens than did control animals.95 Both macrophage inflammatory protein-2 (MIP-2) and KC/CXCL1, two neutrophil-attracting CXC chemokines, were significantly elevated in the brain after S. aureus exposure, thus indicating the importance of the CXCR2 ligands MIP-2 and KC, as well as neutrophils, in the acute host response. The continued release of proinflammatory mediators by activated glia and infiltrating peripheral immune cells may potentiate the subsequent recruitment and retention of newly recruited inflammatory cells and glia,96 thereby perpetuating the antibacterial inflammatory response. Recent studies support this persistent immune activation associated with experimental brain abscess in which increased concentrations of IL-1α, TNF-α, and MIP-2 were detected between 14 and 21 days after S. aureus exposure,97 thus suggesting that intervention with anti-inflammatory compounds, subsequent to bacterial neutralization, might minimize damage to the surrounding brain parenchyma. Although Toll-like receptor 2 (TLR2) has an important role in mediating S. aureus–induced activation, additional receptors are also involved in glial responses to S. aureus. With progression to the late cerebritis stage, the acute inflammatory cells become mixed with macrophages and fibroblasts, and reticulin formation surrounds the necrotic center. As the capsule begins to form, increased numbers of fibroblasts and macrophages infiltrate the periphery, and mature collagen is deposited to form a capsule. The necrotic center then continues to decrease in size while marked gliosis develops outside the capsule.
Despite the presence of virulence factors of the organism that resist host defense mechanisms, the host inflammatory response is important in containment of the abscess, as has been examined with the use of immunosuppressed animals. Initial studies in a dog model of experimental brain abscess with S. aureus or Proteus mirabilis demonstrated that the administration of dexamethasone slowed, but did not fully impair, capsule formation.98 In contrast, there was no evidence of capsule formation when dexamethasone was given at the same time as inoculation of either S. pyogenes or S. aureus in another study.99 In an experimental rat model of E. coli brain abscess,90 dexamethasone administration led to a reduction in macrophage and glial responses, collagen deposition, and host survival, with demonstration of an increased number of viable bacteria in the brain abscess. Coadministration of dexamethasone also impaired the lymphocytic and fibroblastic response in a rat model of experimental S. aureus brain abscess,100 although it did not entirely halt the encapsulation or reduce the associated cerebral edema.
Another study in dogs, who were immunosuppressed with azathioprine and prednisone 7 days before the intracerebral inoculation of α-hemolytic streptococci, demonstrated that the immunosuppressed animals manifested a decreased inflammatory response that was characterized by a reduction in neutrophils and macrophages in the lesion, a decrease and delay in collagen deposition, and persistence of viable organisms into the late capsule stage.101 Reduction of neutrophils, plasma cells, lymphocytes, and macrophages in the areas surrounding the necrotic center of the abscess was observed, and cerebritis was also decreased outside the developing capsule. However, gliosis was markedly increased in the area surrounding the collagenous capsule in these immunosuppressed dogs. Although the decreased inflammatory response and edema initially resulted in less mass effect, the eventual size and area of the abscess may have become larger as a result of the diminished host response.
Clinical Findings
The clinical manifestations of brain abscess may run the gamut from indolent to fulminant; most are related to the size and location of the space-occupying lesion within the brain and the virulence of the infecting organism.1–3,8–17 Common symptoms and signs are presented in Table 43-3. Headache is generally observed in 70% to 75% of patients; sudden worsening of the headache, accompanied by new onset of meningismus, may signify rupture of the abscess into the ventricular space.102,103 In one study of 33 consecutive patients with intraventricular rupture of brain abscess, severe headaches and signs of meningeal irritation were prominent findings before rupture, followed by rapid clinical deterioration within 10 days.104 Intraventricular rupture appears to be more likely if the abscess is deep-seated, multiloculated, and in close proximity to the ventricular wall102; a 1-mm reduction of the distance between the ventricle and the abscess increased the rupture rate by 10%. The classic triad of fever, headache, and focal neurological deficits is seen in less than 50% of patients with brain abscess. The specific neurological findings of brain abscess are also defined by location within the CNS (Table 43-4).1–3,9–16,105,106 In immunocompromised patients, the clinical findings may be masked by the diminished inflammatory response.
TABLE 43-3 Initial Symptoms and Signs in Patients with Brain Abscess
| SYMPTOM OR SIGN | FREQUENCY RANGE (%) |
|---|---|
| Headache | 49-97 |
| Fever | 32-79 |
| Focal neurological deficits* | 23-66 |
| Altered mental status | 28-91 |
| Seizures | 13-35 |
| Nausea and vomiting | 27-85 |
| Nuchal rigidity | 5-41 |
| Papilledema | 9-51 |
* The specific deficit depends on the central nervous system location of the abscess (see Table 43-4).
Data from references 1, 2, 8, 9–17, 102.
TABLE 43-4 Possible Initial Findings in Patients with Brain Abscess Based on Intracranial Location
| INTRACRANIAL LOCATION | FINDING |
|---|---|
| Parietal lobe | |
| Frontal lobe | |
| Temporal lobe | |
| Cerebellum | |
| Brainstem |
The clinical manifestations of brain abscess may also be defined by the infecting pathogen. For example, patients with nocardial brain abscess may have concomitant pulmonary, skin, or muscle lesions53,54,107; however, the CNS findings are more often nonspecific and associated with fever, headache, and focal neurological deficits defined by location. Patients with Aspergillus brain abscess commonly manifest signs of a stroke syndrome as a result of ischemia or intracerebral hemorrhage, or both, that is referable to the involved areas of the brain.65,67,68 Patients who are severely immunocompromised usually have nonspecific findings shortly before death, whereas those who are less immunocompromised are more likely to have headache and focal neurological deficits, but evidence of aspergillosis in other organ systems is usually apparent.
Patients with rhinocerebral mucormycosis initially have symptoms referable to the eyes or sinuses and complaints of headache, facial pain, diplopia, lacrimation, and nasal stuffiness or epistaxis.65,69 With continued infection and spread to contiguous structures, necrotic lesions appear in the turbinates, nose, paranasal skin, or hard palate; chemosis, proptosis, and external ophthalmoplegia may also occur. Cranial nerve involvement is common, and blindness may occur as a result of invasion of the cavernous sinus, ophthalmic artery, and orbit. Because the organism has a proclivity for blood vessel invasion, thrombosis is a striking feature of the disease. Far advanced disease is suggested by focal deficits such as hemiparesis, seizures, or monocular blindness. In patients with the nonrhinocerebal form, fever, headache, and focal neurological deficits are present in more than half the patients. In one review of 22 cases, half the patients were injection drug users and the basal ganglia was the most commonly involved site.70
Scedosporium apiospermum brain abscess tends to occur in immunocompromised patients or in individuals 15 to 30 days after an episode of near-drowning.72,73 The location tends to be in the cerebrum, cerebellum, or brainstem. Clinical findings include seizures, altered consciousness, headache, meningeal irritation, focal neurological deficits, abnormal behavior, and aphasia.
Diagnosis
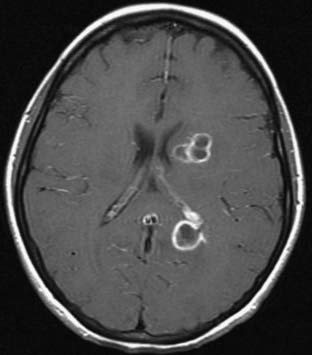
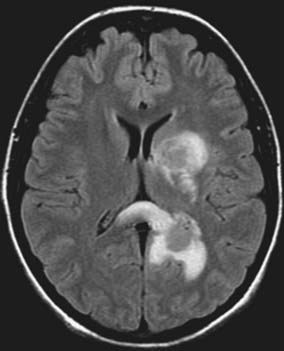
Magnetic resonance imaging (MRI) is the diagnostic neuroimaging procedure of choice in patients with brain abscess; it is more sensitive than computed tomography (CT) and offers significant advantages in the early detection of cerebritis, more conspicuous spread of inflammation into the ventricles and subarachnoid space, and earlier detection of satellite lesions (Figs. 43-1 and 43-2).17,108 On T1-weighted images, the abscess capsule often appears as a discrete rim that is isointense to mildly hyperintense; administration of gadolinium-diethylenetriaminepentaacetic acid helps clearly differentiate the central abscess, surrounding enhancing rim, and cerebral edema. On T2-weighted images, the zone of edema that surrounds the abscess demonstrates marked high signal intensity in which the capsule now appears as an ill-defined hypointense rim at the margin of the abscess. On diffusion-weighted images, restricted diffusion (bright signal) may be seen and may distinguish abscesses from necrotic neoplasms.3 Proton MR spectroscopy is another diagnostic modality that may assist in differentiating between malignant tumors and cerebral abscesses; when combined with diffusion-weighted imaging, MR spectroscopy can significantly increase the diagnostic accuracy of conventional MRI.109 In patients who cannot undergo MRI, CT with and without intravenous contrast enhancement is recommended; there is characteristically a hypodense center with peripheral uniform ring enhancement after the intravenous injection of contrast material.110–112 Other findings include nodular areas and regions of low attenuation without enhancement, the latter finding seen in the early cerebritis stage before abscess formation. In later stages, contrast material no longer differentiates the lucent center, and the CT appearance is similar to that of the early cerebritis stage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree