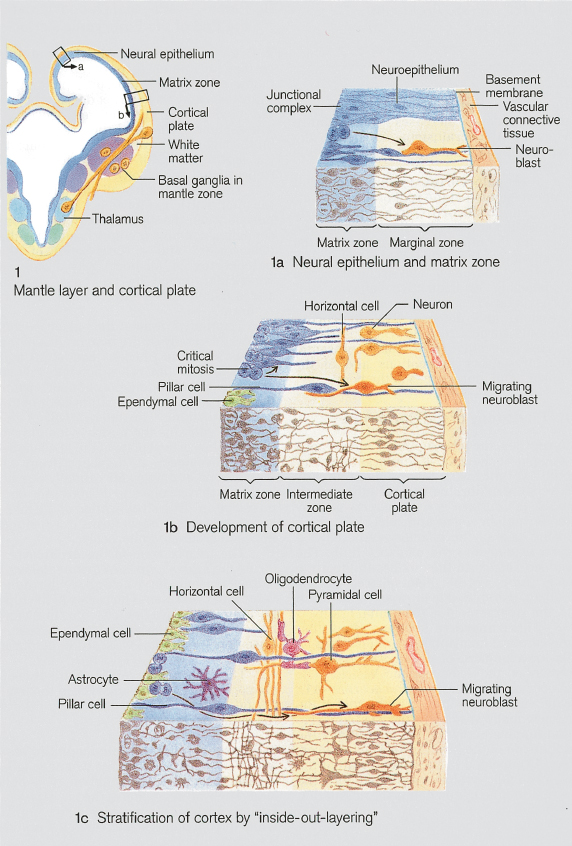
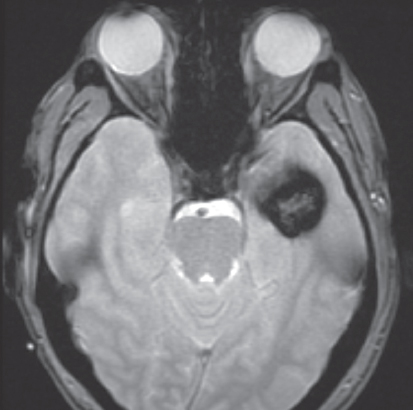
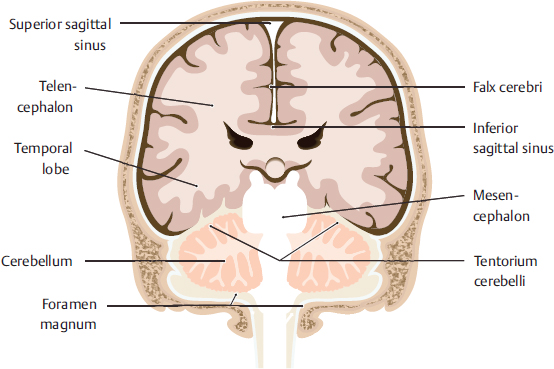
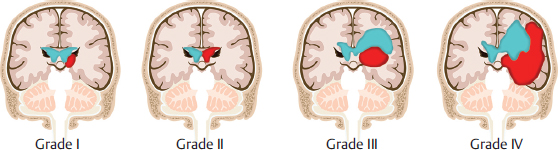
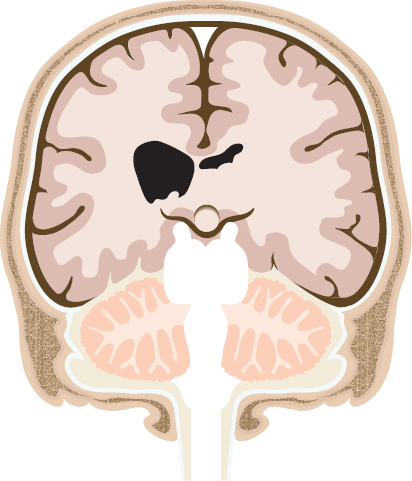
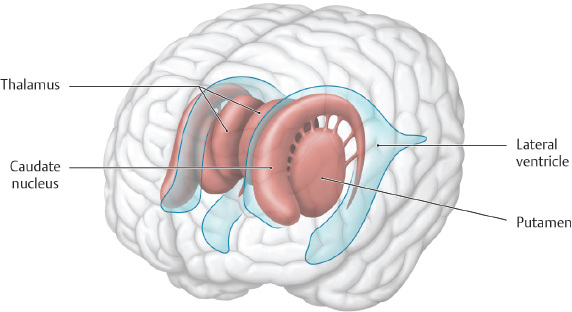
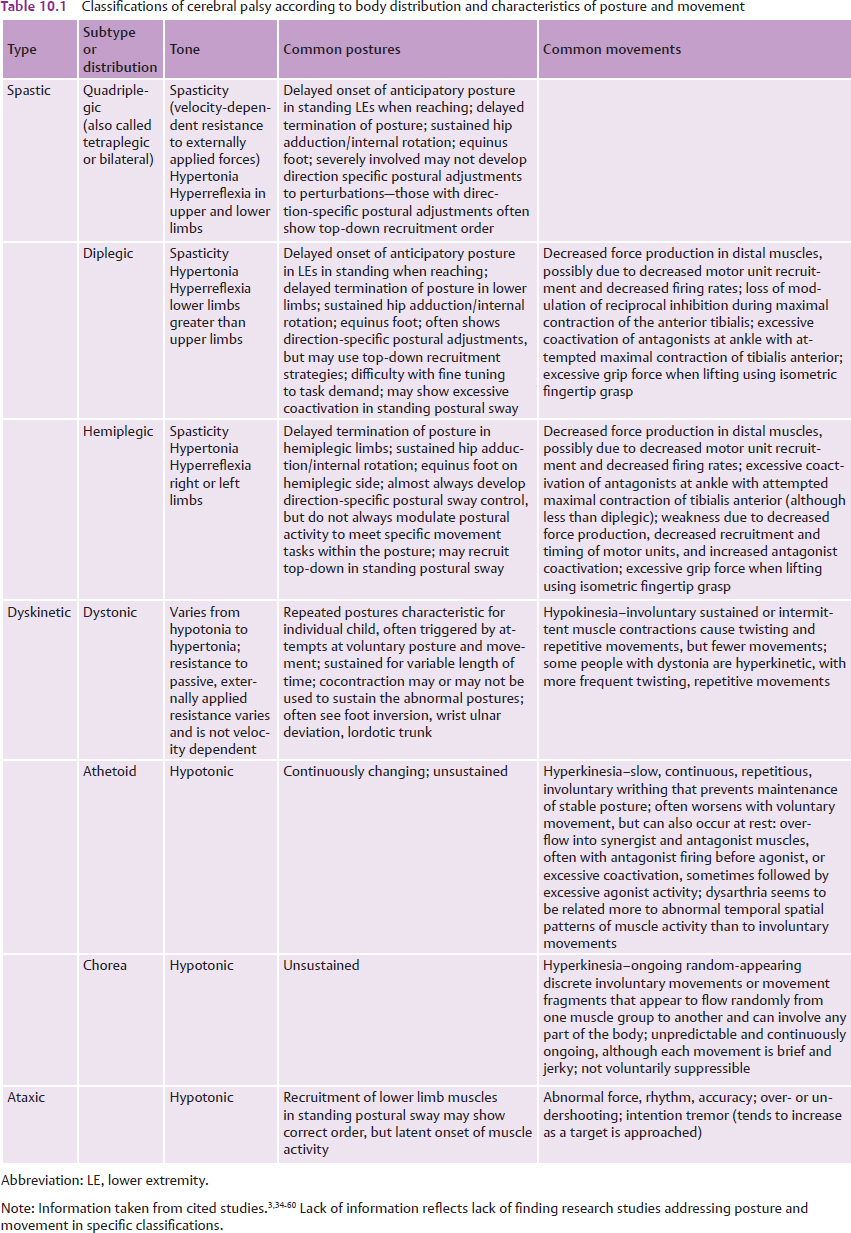
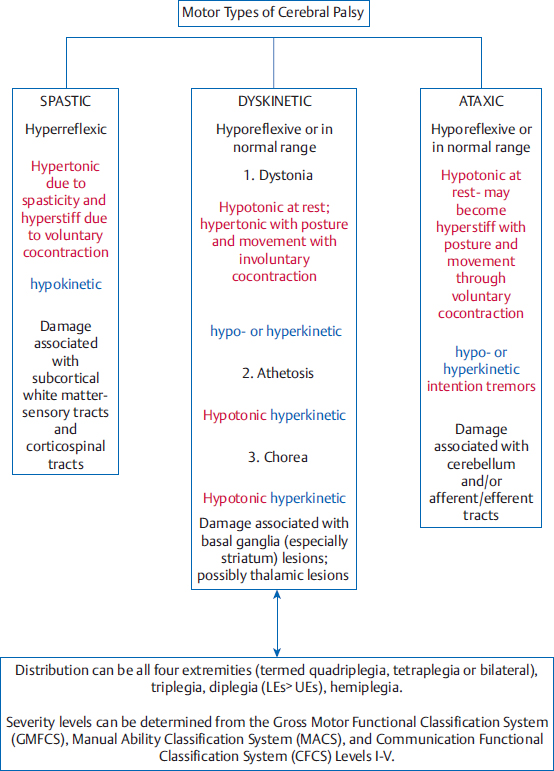
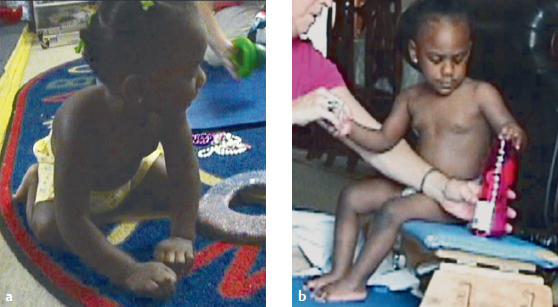
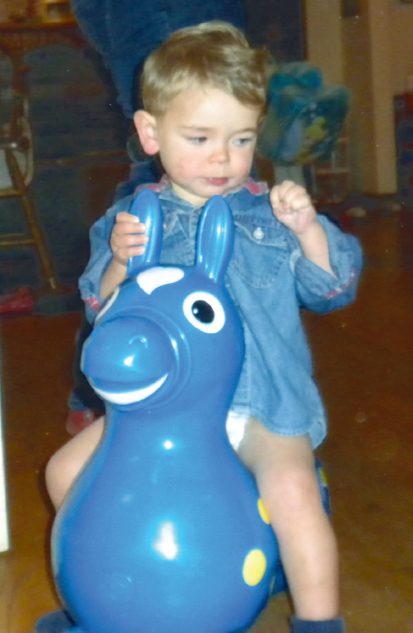
10 Cerebral Palsy This chapter provides essential information about postures and movements expressed in people with cerebral palsy (CP). Neuro-Developmental Treatment (NDT) recognizes that each person participates and chooses activities because of complex and interacting factors and that each person will have a unique combination of abilities and disabilities as well as effective and ineffective postures and movements. This chapter describes common postures and movements observed in many people with CP and provides core knowledge needed for examining and evaluating their effects on activity and participation. Learning Objectives Upon completing this chapter the reader will be able to do the following: • Define CP according to the consensus definition from the international definition of 2004. • State the three primary classifications of CP, describing their identifying positive and negative impairments. • Identify the typical sites of lesions for the three primary classifications of CP. • Describe posture and movement impairments that are typically seen in children with the following: • Describe at least three unique impairments that an adult with CP is likely to contend with, relating these impairments to the need for advocacy for lifetime episodes of care. Cerebral palsy (CP) has been recognized as a central nervous system (CNS) pathology since at least the 19th century.1,2 Cerebral refers to the brain and palsy to a general paralysis. These terms can be misleading because palsy in cerebral palsy refers to impaired voluntary posture and movement control rather than complete loss of muscle activity. Authors describing CP have considered revising the name of this disability to reflect a more accurate description3,4 but state that the term is well established in the literature and culture and so recommend that the term not be changed. In the 20th century, two definitions of CP dominated the literature. The first was Bax’s definition: “a disorder of movement and posture due to a defect or lesion of the immature brain”5 (italics added). A second, oft-quoted definition by Mutch et al6 defined CP as “an umbrella term covering a group of non-progressive, but often changing, motor impairment syndromes secondary to lesions or anomalies of the brain arising in the early stages of development.” Recently, researchers felt a need to update the definition in light of the complexity and breadth of the disorders grouped as CP. An executive committee meeting for the definition of CP3 in an international workshop held in Bethesda, Maryland, in 2004, wrote and revised this definition: Cerebral palsy (CP) describes a group of permanent disorders of the development of movement and posture, causing activity limitation, that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The motor disorders of cerebral palsy are often accompanied by disturbances of sensation, perception, cognition, communication, and behavior; by epilepsy, and by secondary musculoskeletal problems.3 This definition emphasizes many important points about CP. First, CP is a heterogeneous group of disorders. Blair and Watson7 emphasize that CP is a description, not a diagnosis, whereas Shevell et al8 describe CP as a “symptom complex” to denote the wide range of presentations, etiologies, impairments, and functional implications possible. Palisano et al9 created the Gross Motor Function Classification System (GMFCS), Eliasson et al10 created the Manual Ability Classification System (MACS), and Hidecker et al11 created the Communication Function Classification System (CFCS) to classify CP according to the range of functional abilities and limitations, which emphasizes their wide variation. Classifying people with CP according to activity rather than type of tone and its limb distribution may be a more valid and reliable method of classifying for research and epidemiological consistency.8 This newer definition continues to emphasize the central characteristic common to all children and adults with CP—that it is a group of disorders of posture and movement. This is particularly relevant to clinicians who practice using Neuro-Developmental Treatment (NDT) because the NDT Practice Model emphasizes knowledge and careful analysis and treatment of posture and movement. The definition of CP also emphasizes that, although the anomalies and lesions that cause CP are nonprogressive, the effects on a young and developing brain cause an ever-changing posture and movement disorder.8,12 These effects persist throughout the life span, which approaches a typical length in those who are not severely involved.13,14,15,16,17,18,19 Researchers are interested in linking pathology of brain anomalies and lesions and the timing of them to particular types of CP, if possible. Researchers state that the causal links from pathology to type of CP are currently weak, although magnetic resonance imaging (MRI) shows lesions and anomalies in over three-fourths of people with CP,2,20,21,22 and estimating the timing of lesions is becoming more exact. The following information is tentative and will likely change as studies with more powerful diagnostics become available. However, we should begin to study this information and follow its evolution closely. Advances in neuroradiology have made defining and differentiating pathologies that can cause CP more possible. In the CNS, the many developing structures and pathways are more vulnerable to injury at different stages of development. Identifying when an insult occurs or a structure malforms is of great importance.20 The effects of the insult or anomaly will also be shaped by its severity and duration (e.g., asphyxia will have a more profound effect than transient hypoxia). Some researchers question the usefulness of the current classifications of CP by distribution and posture/movement because the timing and type of insults that cause CP result in differing clinical presentations. Rosenbloom23 notes that there are huge differences among children classified as quadriplegic due to differing pathologies (e.g., extensive white matter damage vs. ischemic infarction vs. extensive neuronal migration abnormalities). He calls for better clinical descriptions of the classification of CP to develop appropriate services and prognoses. Congenital malformations usually indicate injury to CNS development during the first half of pregnancy.20 Malformations are usually the result of interruptions of migrating neurons during the developmental process of forming layers of the cortex and synaptic connections (Fig. 10.1). If malformations result in the posture and movement disorders defined as CP, they are included with this diagnostic category (as opposed to malformations such as neural tube defects that may cause disorders such as spina bifida and anencephaly).2 Kułak et al25 noted congenital brain anomalies as a frequent cause of spastic quadriplegia (other causes in their study were white matter damage and cerebral atrophy), whereas Feys et al26 found malformations as one cause of hemiplegic CP (Fig. 10.2). Focal malformations in the supra- and infratentorial regions (Fig. 10.3) and extensive cerebellar malformations have been implicated in ataxic CP.27 Minor structural anomalies in the mouth, hands, feet, and trunk of some children with ataxia suggest that these congenital malformations occur in the early prenatal period.28 Primary white matter damage is often seen in children with spastic forms of CP.2 Malformations of the corpus callosum are one type of white matter damage; myelin abnormalities are another. White matter damage of immaturity results from insults between 24 and 34 weeks’ gestation and often results in preterm birth.20,29,30 Bax et al31 state that 71% of children with spastic diplegia show evidence of white matter damage of immaturity, including periventricular leukomalacia (PVL) and periventricular hemorrhage (Fig. 10.4). PVL is likely to be caused by both vascular and metabolic lesions.25 Some children with spastic quadriplegia also show white matter damage (to a greater extent than those with diplegia). Focal lesions close to term are often in the territory of the middle cerebral artery, often resulting in hemiplegia.20 Bax et al report that 27% of children with hemiplegia in their studies had strokes. Some children with hemiplegia show asymmetrical PVL31 (Fig. 10.5). Feys et al26 state that many children in their study of hemiplegic CP had a combination of white matter damage and basal ganglia/thalamic involvement. Reduced thalamic volume was seen in preterm children with moderate to severe white matter damage in a study by Lin et al.32 When the infant’s brain is close to gestational maturity, the gray matter is more sensitive to injury than the white matter,20 and damage is often associated with various levels of hypoxia and anoxia. Gray matter is present in the cerebral cortex and the subcortical nuclei, including the basal ganglia and thalamus. Koman et al30 note that the basal ganglia have unique metabolic needs at 38 to 40 weeks’ gestation, creating selective vulnerability that may result in dystonic movement disorders with insults at this time (Fig. 10.6). Bax et al31 state that many children with dystonic or athetoid CP have basal ganglia lesions, and Towsley et al33 found lesions in this subcortical gray matter are often associated with severe CP. Fig. 10.1 Neuronal migration begins in the fifth week of gestation and continues until at least the fifth month of gestation.24 This drawing shows examples of neural migration in the central nervous system. Errors of neuronal migration include lissencephaly, heterotopia, polymicrogyria, and schizencephaly.24 Reproduced from Drews, Color Atlas of Embryology, 4th edition© 1995. Thieme Publishers, Stuttgart. The purpose of classifying CP into distinct posture and movement disorders resulting from early brain lesions and anomalies is to encourage a more standardized terminology for diagnostics, research, and epidemiology studies. Rosenbaum et al,3 Cans et al,34 the Surveillance of Cerebral Palsy in Europe,35 and Sanger et al36,37 have all worked to classify CP in terms of muscle tone and posture and movement characteristics. Researchers such as Nashner et al,38 Rose and McGill,39 van der Heide et al,40 van der Heide and Hadders-Algra,41 Brogren et al,42 van Roon et al,43 Woollacott and Shumway-Cook,44 Hadders-Algra et al,45 and de Graaf-Peters et al46 have focused their studies on postural control of people with and without CP. All state that research about the specifics of postural control variations among the classifications of people with CP is only beginning, and many more studies need to be done to corroborate or challenge their findings. Researchers such as Eliasson et al,47,48,49 Yokochi et al,50 Hadders-Algra et al,51 Hallett and Alvarez,52 O’Dwyer and Neilson,53 Fowler et al,54,55 Fowler and Goldberg,56 Stackhouse et al,57 Tedroff et al,58 Leonard et al,59 and Hirschfeld60 focused their studies on movement disorders in children with CP. Again, these studies are pioneering insights into the particular movement disorders that accompany various classifications of CP. Fig. 10.2 This image depicts a cavernous malformation, a vascular malformation that can cause focal neurological impairments and seizure activity. Reproduced from Tsiouas et al, Case-Based Brain Imaging, 2nd edition© 2013. Thieme Publishers, New York. Fig. 10.3 Malformations in the area of the tentorium, the dural covering of the cerebellum, may cause ataxic cerebral palsy. Modified from Schuenke, Schulte, Schumacher, Head, Neck, and Neuroanatomy, 2nd edition© 2016. Thieme Publishers, New York. Table 10.1summarizes posture and movement characteristics of people with CP. Fig. 10.7 diagrams the motor types of CP with characteristics of pathophysiology, muscle tone, and movement. While research contributes more and more information about the impairments observed and measured in the defined classifications of CP, it does not describe posture and movement in detail. Recall in Chapter 3 about NDT and the International Classification of Functioning, Disability and Health (ICF) model that the foundation of problem solving in NDT is generating hypotheses about the relationships of pathology to impairments, impairments to posture and movement, and all of these domains of functioning to contextual activities and participation. Hypothesis generation is difficult, especially if the clinician does not have a detailed understanding of the common postures and movements that people with CP use and why they are there. Describing and defining postures and movements in detail are also necessary for interpreting effectiveness of interventions aimed at improving activity and participation outcomes. Because CP is a heterogeneous group of posture and movement disorders, intervention strategies that are effective for one person with CP may be inappropriate for another person with very different impairments, activities, participation, and the context in which all of these interact. The clinician uses research to guide and inform decision making, not as a recipe for intervention for individuals. Fig. 10.4 Periventricular hemorrhages of grades III and IV with resultant ventricular enlargement are a frequent finding in children with spastic quadriplegia.25 The clinician using NDT must always remember that any description of CP is a description of commonly observed and measured phenomena. The following information will be useful only insofar as it allows clinicians to improve observation skills and deepen their understanding of posture and movement. The most important skill a clinician using NDT can develop is the ability to observe and measure each individual’s functioning and then create hypotheses about possible causes and relationships of findings. Children with spastic forms of CP make up ~ 80 to 86% of people who have CP where CP registers are kept.35,61,62 Lesions that cause spastic CP are located in the cerebral cortex and the subcortical white matter. These lesions may be the results of errors of neuronal migration, hypoxic/anoxic events, bleeding of the cerebral blood vessels into the brain and ventricles, cerebral atrophy, and other structural malformations. The resultant damage may be focal or diffuse, causing a person to develop quadriplegia (total body involvement), diplegia (lower body more involved than upper body), or hemiplegia (one side of the body involved). Clinically, this clear-cut division of distribution is rarely seen. Many children present asymmetrically in addition to the described distribution or have three limbs involved with one limb relatively spared (often an upper extremity). In addition, the extent of the damage will initially determine the severity of the posture and movement disorder. For example, a person could have quadriplegic distribution and attain motor goals, such as walking, speech, and many independent activities of daily living, whereas others may not be able to achieve these skills at all, even with excellent intervention and care. The lesions that result in spasticity damage the corticospinal tracts and other descending tracts that transmit direct posture and movement commands, which carry motor commands from the cerebral cortex through the subcortical internal capsule, crossing at the medulla to travel down the spinal cord. The corticospinal tracts carry information for motor commands and are the largest motor tracts that descend through the spinal cord and synapse with spinal afferents and efferents. The tracts synapse with α motor neurons at all spinal levels to give commands to muscles. Positive primary impairments that result from damage to these upper motor neurons result in abnormal responses to velocity-dependent stretch, which defines spasticity. Fig. 10.6 Damage to the basal ganglia in babies at term birth is thought to occur primarily in the putamen and caudate nucleus. Damage to the thalamus may also result in dystonic cerebral palsy. Reproduced from Schuenke, Schulte, Schumacher, Head, Neck, and Neuroanatomy, 2nd edition© 2016. Thieme Publishers, New York. Spasticity is often not immediately apparent in the infant. The typical presentation of an infant who will later express spasticity and other primary impairments is that of generalized hypotonia.63 This hypotonia could be a systemic response to trauma or an expression of the immaturity of the motor system. Spasticity is examined by responses to externally imposed passive joint ranging at increasing speeds.36 Increasing speed causes increased resistance to joint mobility through excessive muscle activity, and often, a spastic catch abruptly halts movement that may indicate the threshold of the stretch reflex. Deep tendon reflexes are hyperreflexive. Spasticity continues to be a poorly understood mechanism; however, lack of cortical inhibition and hypersensitivity to stretch originating in the muscles themselves are often implicated as possible causes of the abnormal velocity-dependent responses. Supraspinal lesions may disrupt presynaptic inhibition, reciprocal inhibition, and recurrent inhibition.64 These lesions may disrupt the balance of excitatory and inhibitory pathways. Spasticity, therefore, may not be only one phenomenon since there may be more than one source as its cause. Research is needed to explain if and how spasticity disrupts voluntary movement. Negative primary impairments that result from upper motor neuron lesions include the loss of selective motor control. This loss is expressed as errors in timing and ordering of muscle contraction, errors in the ability to select some motor units while others remain inactive, errors in the ability to recruit sufficient motor units for the task,39 and errors in the ability to terminate a muscle contraction (errors in the ability to inhibit motor units once activated). The result is often overrecruitment of muscles (usually superficial, two-joint muscles), overrecruitment of muscles not needed for efficient movement (mirroring and overflow are terms often used to describe this error), and underrecruitment of muscle activity responsible for joint stability and postural control. When the lateral corticospinal tract is involved, loss of fractionated movement in the distal upper extremity results. Other negative primary impairments that are often seen in children with spasticity are visual processing impairments due to lesions affecting the optic tracts as they travel from the optic chiasm to the occipital cortex, somatosensory impairments due to damage of the primary sensory strip and association areas in the parietal lobe, central vestibular impairments, and impairments of conscious proprioception processing. The parietal lobes of the cerebrum receive, process, and route somatosensory information. Babies who develop spastic CP may or may not be born prematurely, depending on the timing of the lesion and its cause, as well as the health of the mother and external environmental conditions. Many children with spastic diplegia and subcortical white matter damage are born prematurely; others are born at term. Initially, caregivers and professionals frequently note generalized hypotonia, or occasionally hypertonia, with poverty of movement in infants who will later be diagnosed with CP.63 Detailed examination may show abnormal general movements over time predictive of CP and lack of development of fidgety general movements typically seen from ~ 6 weeks postterm to 4 months post-term.65,66 Spontaneous movements of preterm and term babies can be assessed using the General Movements Assessment (GMsA), which measures qualitative movements over time.67 Other tests quantify and qualify posture and movement performance. One test, the Test of Infant Motor Performance (TIMP),68 specifically identifies postures and movements in infants. Research using the TIMP has shown that infants later diagnosed with CP showed delayed postural control as early as 7 days of age on items related to head control, antigravity arm movements, and facilitated rolling.69 In addition, several TIMP items are particularly effective in documenting early regression of postural control. In a group of 10 infants later diagnosed with CP, TIMP scores on antigravity items, such as bilateral hip and knee flexion, reciprocal kicking, and selective control of ankle movements, regressed when tested longitudinally at neonatal intensive care unit discharge and 4 months post–conceptual age. Assessments of infants serve different purposes. Whereas the GMsA is used to help identify infants who are at high risk for the development of CP, other assessments, such as the TIMP and the Alberta Infant Motor Scales (AIMS), assess posture and selective movement.67 The TIMP can be used to assess progress with intervention as well. NDT-educated clinicians select different tests and assessments to identify, predict, and measure functional skills in people with CP throughout their life span, ensuring the measure selected is validated to test the desired clinical outcome. Test results can then be accurately interpreted within the confines of the outcomes the test is able to assess. Care is taken not to interpret the meaning of test outcomes in ways they are not intended; for example, the Bayley Scales of Infant Development are designed as normative scales of development that can be used to determine eligibility for programs for children with disabilities.70 The Bayley Scales are not designed to measure the effectiveness of treatment and are therefore not valid for measuring outcomes of intervention. In NDT, we hypothesize that the primary positive and negative impairments immediately affect posture and movement, as well as influence each other as the baby attempts to move against gravity and interact with caregivers and the environment. Damage to the sensory systems, depending on which ones are damaged and how severely, can affect the baby’s awareness of body position (proprioception), stability and movement of the head (vision, vestibular, and proprioception), and perception of environment (vision, hearing, tactile, vibration). Spasticity, although tested passively, causes excessive resistance to actively generated movements, restricting range of joint mobility and length of muscle. Spasticity may also contribute to abnormal sensory feedback about internal and external events relative to the body. Muscles responsible for antigravity postures and joint stability may be difficult to contract with sufficient force or force that can be sustained long enough to control body position. The baby is often restricted to muscle contractions in the sagittal plane and may rely on flexion or extension of many joints of the body at the same time to produce movement (lack of selective control). The following initial postures and movements are typical of babies and young children with spastic CP due to the interaction of impairments: • A compromised ability to initiate and sustain antigravity postures. Recall that, in CP, muscles responsible for posture and stability are difficult to contract. This initially affects head and trunk postures against gravity in those who have total body involvement or moderate to severe diplegia. Babies and young children developing with hemiplegia will most likely develop asymmetrical postures due to asymmetrical muscle activity. Sensory losses and/or abnormal sensory processing usually add to the degree of postural inefficiency. • Babies and children will attempt to interact with caregivers and the environment despite poor abilities to control antigravity postures. This interaction means that the baby and child must use compensations for the ineffective antigravity postures. These compensations are variable and dependent on the context of the family environment and family dynamics, as well as the extent, number, and severity of posture and movement impairments present in the baby and young child. Children with spasticity can frequently increase joint stiffness through co-contraction or by sustaining one or more superficial muscles in contraction (active stiffness). Often, many muscles are recruited. Abnormal muscle activity is imposed on poor alignment of body segments because the muscles are used in the shortened positions often retained from infancy. Joint and bone structure, different in infants than in older children, and normally molded by normal muscle pull, normal muscle tension, and active and passive joint stability, not only retains infant structure, but deforms in response to abnormal and prolonged muscle activity. Secondary impairments in the musculoskeletal system can appear even in young children as a result, and the person with spastic CP is vulnerable to these impairments over the life span. One difficulty this stiffness presents for the clinician is that the resistance when the child is held, carried, dressed, fed, and assisted to move is often attributed to spasticity only, when it may, in reality, be due to both spasticity and compensatory voluntary contraction of muscles designed for movements. Superficial, two-joint muscles are designed for large-range movements rather than the way children with spastic CP must use them in attempts to initiate and sustain antigravity postures. The child learns that this contraction must be sustained to prevent falling and to attempt any control of posture and movement at all. For example, as described in the case report about Makayla in Unit V (B4) (Fig. 10.8a, b), she moves across the floor on all fours with her hands fisted. Her stiff movements on all fours with fisted hands may be incorrectly evaluated as spasticity only. Most likely, however, a more complex interaction of spasticity, voluntary cocontraction and excessively sustained muscle contractions in select muscles, and insufficient muscle length or joint mobility in some body segments results in the posture and movement she uses. The clinician using NDT carefully examines and evaluates the person with spastic CP, asking the caregivers how the child initiates postures and movements, responds to postures and movements imposed on him or her, and performs activities. The clinician begins to formulate hypotheses to explain the child’s particular posture and movement repertoire. Through observation, handling for examination, and assisting postures and alignment to see how the child responds, the clinician hypothesizes about the interaction of impairments and the compensations developed to allow function, predicting how these may affect future postures and movements. For example, Makayla uses upper extremity and chin support at times when she is standing at furniture to widen her base of support (Fig. 10.9). Her physical therapist generates the following hypotheses as to why Makayla must use this posture: Fig. 10.8 (a) Makayla moves around the floor with fisted hands. (b) When Makayla feels safe in her position against gravity and the demands on her postural control include the muscles that provide stability to the spine, rib cage, and pelvis, she is able to easily open her hands to play with toys, indicating that the fisting of her hands on all fours is not the result of spasticity only, and in fact, may not be due to spasticity at all. Fig. 10.9 When Makayla stands supported, she is unable to extend her trunk, hips, and knees. With her flexed posture and center of mass shifted anteriorly, she rises onto her toes. In infants born full term without neurological insults, the rib cage sits in the upper third of the length of the trunk and the thoracic and lumbar spine is in flexion. The shoulder complex is elevated with the scapulae elevated and abducted. The hips are flexed, abducted, and externally rotated, although the femur itself has internal torsion along its long axis. The acetabulum is shallow. The infant’s elbows and knees do not fully extend due to soft tissue limitations of the two joint flexors, and the hands are loosely fisted. The fingers and toes extend and abduct briefly with general body movements (Fig. 10.10). Refer to Chapter 14 on motor development for a more detailed description. Makayla may retain some of these morphological characteristics seen in infants if she does not use antigravity postures and movements that would change structure in the manner that typically developing children change their structure. Her structure could also change in atypical ways based on the common postures and movements she uses (Fig. 10.11). The constraints imposed on people with spastic quadriplegia due to their impairments include the following: • Muscles used for postural control and joint stability against gravity are difficult to recruit throughout the body (this difficulty varies with the severity of CP). • When muscles are recruited, superficial, two-joint muscles are likely to be recruited first (and sometimes exclusively) and/or without the stabilizing effect of postural muscles that work in synergy with two-joint muscles in people without neurodisability. Recruitment is ungraded, often with overflow into unnecessary and often antagonistic muscles. As a result, inefficient cocontraction and/or overflow results and persists, increasing active joint stiffness. Another result is that the two-joint muscles work in small ranges only, sustaining activity longer than functional demands require, and eventually shortening. • Over the life span, muscles that are recruited and sustained in short ranges tend to alter the proportion of fiber types, alter in extracellular structure, and may be infiltrated by collagen.39,71,72 Therefore, muscle tissue and surrounding soft tissues shorten and change in structure and function. Altered muscle activity alters the pull on bones, as do lack of weight bearing and movement. All result in a process of secondary impairments of increasing bone and joint deformities. Fig. 10.10 This infant, who is 10 days old and full-term, demonstrates the physical proportions and positions described in the text. Her morphological characteristics limit movements, such as cervical extension with capital flexion; full thoracic, lumbar, and hip extension; costovertebral mobility with respirations; and hand movements toward midline. Fig. 10.11 Makayla’s shoulder complex is almost always in a position of elevation, similar to the position seen in young infants. Active muscle contractions of the thoracic and lumbar superficial and deep extensors, abdominals, and scapular stabilizers change the shoulder complex position in children developing without neuromuscular impairments. Makayla has not been able to establish this neuromuscular control yet, and may be actively using shoulder complex elevation to assist with her antigravity postures and movements. She is not able to free her arms for play in supported standing, however, using this strategy. • Perception of the self and the environment is altered due to altered body segment alignment, limited successful antigravity postures, and poverty of movement, as well as due to any primary sensory system impairments that alter the development of perception. Infants and young children with spastic quadriplegia are usually capable of generating simple synergies of flexion or extension in the axial muscles.45 Muscle contractions are often initiated from the infant position of head asymmetry with an immobile and elevated rib cage. Because postural activity does not develop well to stabilize joints and body segments against gravity, the child uses what she or he has: the ability to sustain contractions in two-joint muscles to assume and sustain antigravity postures. This strategy is often partially successful, allowing some function. The child is stiff, moving in small ranges. Stiffness increases with effort and is often interpreted incorrectly as increased spasticity (Fig. 10.12). Muscles of the trunk that work hard to attempt antigravity postures and movements include the pectorals, latissimus dorsi, scapular elevators, and erector spinae (most effective in the cervical and lumbar spine; they are often overstretched and ineffective in the kyphotic and rigid thoracic spine). The person with spastic quadriplegia often uses breath holding to increase trunk stability at the price of developing controlled exhalation for vocalizing and voicing. Breathing is shallow otherwise, as the thoracic spine remains in flexion and the rib cage remains in its infantile elevated position, limiting lung expansion. The rib cage becomes increasingly rigid as the child matures, and bone replaces the cartilage present in infant rib cages. Often, the rib cage becomes barrel shaped because the child must work hard with the superficial muscles to attempt active stability and sustain respirations (Fig. 10.13). Because the child’s trunk is limited by structure and function as described, the child often attempts to use the limbs to substitute for trunk control. The upper extremities are constrained by pectoral and latissimus action as they insert on the humerus and are used as a part of antigravity control. The price paid is lack of most functions for which the human arm was designed: body weight support, reach, grasp, manipulation, and nonverbal communication. The upper extremities tend to increase their original infantile position of shoulder complex elevation and shoulder extension, becoming ever more internally rotated with the constant activity of the pectorals and latissimus. Because the upper extremities are being used to attempt and augment trunk stability, any attempts to move the child’s arms away from the trunk result in attempts by the child to resist. The child’s resistance is for a good reason—the person attempting to move the arms away from the trunk is taking away the child’s system of antigravity control. The child’s resistance is again misinterpreted as increased spasticity, when, in reality, it is increased voluntary contraction, primarily with two-joint muscles, resulting in increased stiffness or hyperstiffness (Fig. 10.14). Likewise, the hips attempt to substitute for lack of postural control in the trunk. The hips of children with spastic quadriplegia are biased toward flexion, adduction, and internal rotation using the medial hamstrings (long, large muscles). When the child attempts functional activities that require postural control of the trunk and hips, she or he is often unable to generate sufficient activity in the trunk extensors (including the deeper extensors that lie close to the facet joints), the pectorals as horizontal adductors, the intercostals and oblique abdominals, and the gluteal muscles. So the child uses muscles that are easiest to recruit: hip flexors, adductors, and medial hamstrings. The gastrocnemius, a large two-joint muscle, is also recruited and sustained in a shortened range (Fig. 10.15). Fig. 10.12 This young child with congenital left hemiplegia shows stiffness in his left upper extremity. Is this stiffness entirely attributable to spasticity? Or are additional neural and nonneural impairments in the neuromuscular system contributing to his stiffness? Is his upper extremity postured this way to assist trunk extension? Or is his posture protective of his arm because his sensory reception or processing of sensation is different between left and right arms? There may be other explanations for his left upper extremity posture too.
 Spastic quadriplegia.
Spastic quadriplegia.
 Spastic diplegia.
Spastic diplegia.
 Spastic hemiplegia.
Spastic hemiplegia.
 Dyskinetic dystonia.
Dyskinetic dystonia.
 Dyskinetic athetosis.
Dyskinetic athetosis.
 Dyskinetic chorea.
Dyskinetic chorea.
 Ataxia.
Ataxia.
 Mixed spastic dystonia.
Mixed spastic dystonia.
 Mixed ataxia diplegia.
Mixed ataxia diplegia.
10.1 What Is Cerebral Palsy?
10.1.1 Types and Timing of Pathologies That Can Cause Cerebral Palsy
10.1.2 Classification of Cerebral Palsy by Body Distribution and Characteristics of Posture and Movement
10.1.3 Classification of Cerebral Palsy for the Clinician
10.1.4 A General Description of Children with Spastic Cerebral Palsy
Primary Pathology
Early Development in Children with Spastic Cerebral Palsy
 She has not developed control of her trunk in extension.
She has not developed control of her trunk in extension.
 She has not developed control of hip and knee extension with a plantigrade foot in standing.
She has not developed control of hip and knee extension with a plantigrade foot in standing.
 She cannot effectively initiate and terminate any lower extremity (LE) muscle groups to adjust hip, knee, and ankle joint position in supported standing.
She cannot effectively initiate and terminate any lower extremity (LE) muscle groups to adjust hip, knee, and ankle joint position in supported standing.
 She is not able to use or has not developed the ability to use the anterior trunk and hip, knee, and ankle muscles to recover balance if her center of mass is displaced toward the back of her base of support when sitting or standing with support.
She is not able to use or has not developed the ability to use the anterior trunk and hip, knee, and ankle muscles to recover balance if her center of mass is displaced toward the back of her base of support when sitting or standing with support.
Typical Postures and Movements in Children with Spastic Quadriplegia
< div class='tao-gold-member'>
Cerebral Palsy
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree