CHAPTER 357 Cerebral Venous and Sinus Thrombosis
History and Clinical Significance
Cerebral venous thrombosis (CVT) is a pathologic condition encompassing thrombosis of the cortical and deep cerebral veins and the dural sinuses. It was first described by Ribes in the early 19th century in a 45-year-old man harboring a systemic malignancy who had thrombosis of the superior sagittal sinus demonstrated at autopsy.1 CVT is thought to be a rare clinical problem, but the exact incidence is unknown. Because of the rarity of the disease and its nonspecific clinical findings, the diagnosis of CVT is difficult to make and frequently delayed.
Pathogenesis
When thrombosis occurs in the cerebral veins and dural sinuses, the resulting venous hypertension causes hypoxia of the brain with subsequent neuronal ischemia, similar to the symptomatology of dural arteriovenous fistulas.2 The spectrum ranges from varying degrees of cerebral edema to massive hemorrhage and often bilateral cerebral infarcts. The potential causes of and risk factors associated with CVT are numerous. The underlying mechanisms are related to alterations in the physical properties of the dural sinuses and veins, the chemical properties of blood, or the hemodynamic properties of blood flow.
Vascular injury from trauma causes local endothelial damage and altered hemodynamics. Trauma, neoplasms, and other mass lesions can cause vascular compression and altered hemodynamics as well. The association between dural arteriovenous fistulas and CVT has been recognized3 and is thought to be related to the aberrant rheology induced by the fistulous connection.
Protein C is a vitamin K–dependent, thrombin-activating regulatory protein. Activated protein C has been reported to have potent anticoagulation properties.4 Acquired protein C resistance can also cause a hypercoagulable state,5 and it has been reported as a cause of CVT.6–8 Furthermore, factor V gene mutation (factor V Leiden)7,9 and prothrombin (factor II) gene mutation10 have been determined to be risk factors for CVT. A hypercoagulable state may be present in patients with lupus anticoagulants,11 or circulating autoantibodies directed primarily against phospholipids, and in patients with anticardiolipin antibodies,12 both of which may represent contributing factors in the pathogenesis of CVT.
A number of coagulation system abnormalities that are rarely associated with CVT have been reported in various conditions, including Behçet’s disease,13–15 inflammatory bowel diseases (e.g., ulcerative colitis),16–18 Wegener’s granulomatosis,19 and Cogan’s syndrome,20 among others.
Infection is thought to cause CVT by altering the coagulation cascade and inducing a hypercoagulable state in patients with active infection. Infection used to be a major cause of CVT but, with the advent of modern antibiotic therapy, has become less common. Ameri and Bousser reported that 8.2% of CVT cases are due to infection.21 Cavernous and transverse sinus thrombosis is most frequently associated with infections such as sinusitis, otitis, and mastoiditis. Staphylococcus aureus is the most frequently reported pathogen. In chronic forms, gram-negative rods and fungi such as Aspergillus species are most commonly isolated.22,23
CVT is more common in young women than in other groups,13,22,24–27 and CVT developing during the puerperium is still common in developing countries.13,28 Oral contraceptives may also play a role in the pathogenesis of CVT in young women.7,13,28 Ameri and Bousser reported that 8% of their cases of CVT were thought to be caused by the use of oral contraceptives.21 Martinelli and colleagues reported an association between oral contraceptive use and the development of CVT.7 The risk is much higher in women using oral contraceptives who also have the prothrombin gene mutation. CVT was reported to develop in a postmenopausal woman taking estrogen-progesterone therapy.29
Despite a long list of possible causes of CVT, the inciting factors remain undetermined in some cases. Some investigators estimate that as many as 40% of cases are idiopathic.30,31
Incidence
Although the exact incidence of CVT is unknown, it is agreed that it is a rare disease.21 Most of the estimates are derived from autopsy studies, but autopsy cases may introduce bias because the most severe cases with the worst outcome are overrepresented. Ehler and Courville found 16 cases of superior sagittal sinus thrombosis in a series of 12,500 autopsies.32 Over a 20-year period, Barnett and Hyland found only 39 cases of noninfective CVT that were proved by autopsy.33 Later autopsy studies have reported the incidence to be as low as 0.03%34 and as high as 9% in 182 adult cases.35 Scotti and coworkers observed CVT in approximately 4% of cerebral angiograms performed in 240 children.36 In our experience, clinically significant CVT occurs in patients 2 to 51 years of age.
CVT affects all age groups and both sexes, but with a strong preponderance in women between 20 and 40 years of age.37 This may reflect the fact that women in that age group are more likely to use oral contraceptives38 and undergo changes associated with the puerperium.
Clinical Findings
The clinical manifestations of CVT are highly variable.21,26,27,39–41 Headache is the most common and often the earliest symptom21 and is seen in nearly 80% of patients.13 Nausea, vomiting, and visual changes are other symptoms experienced by patients. Increased intracranial pressure is thought to be the underlying cause of these symptoms. Papilledema is seen in about half of those afflicted, and confusion, agitation, and other changes in mental status occur in about 25% of patients.21 As the disease progresses, focal neurological deficits are present in 50% to 75%, often caused by venous hypertension and cerebral infarction or hemorrhage.13 Aphasia, hemianopia, or hemisensory deficits may also occur. Seizure is another common symptom, with simple or generalized seizures complicating nearly 33% of cases.42
The clinical features also vary according to the site and extent of thrombosis. When thrombosis is limited to the superior sagittal sinus or transverse sinus, the most frequent pattern of findings is isolated intracranial hypertension. If the thrombosis extends to the cortical veins, focal deficits and seizures may occur. Bilateral deficits are typical as late signs of superior sagittal sinus thrombosis. Transverse sinus CVT may be associated with otalgia, otorrhea, cervical tenderness, and lymphadenopathy from an underlying infection such as mastoiditis or otitis media. In cavernous sinus CVT, symptoms often include eyelid edema, chemosis, retro-orbital pain, and exophthalmos. Paralysis of cranial nerves III, IV, V1, V2, and VI may occur because of their anatomic location within the cavernous sinus. When the thrombosis involves the deep venous system, the patient can have akinetic mutism, coma, or decerebration. Mild cases causing memory disturbances or minor confusion may occur. Cortical vein thrombosis without sinus involvement can be manifested as stroke syndromes.43 Cerebellar vein thrombosis is extremely rare and often lethal.24
Diagnostic Evaluation
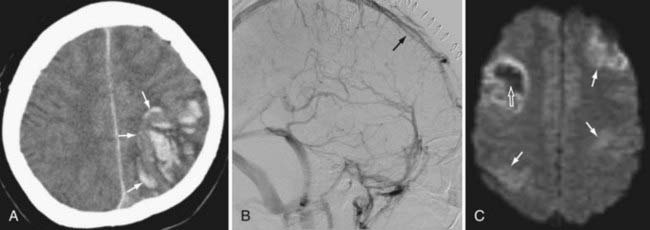
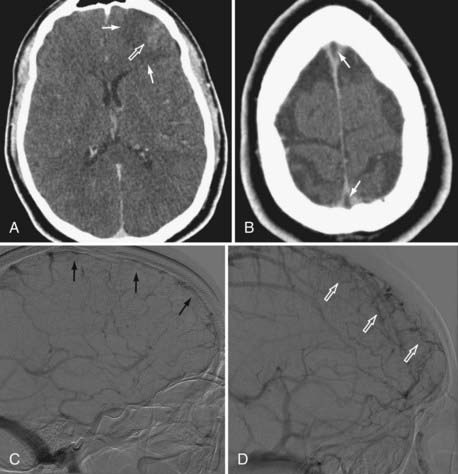
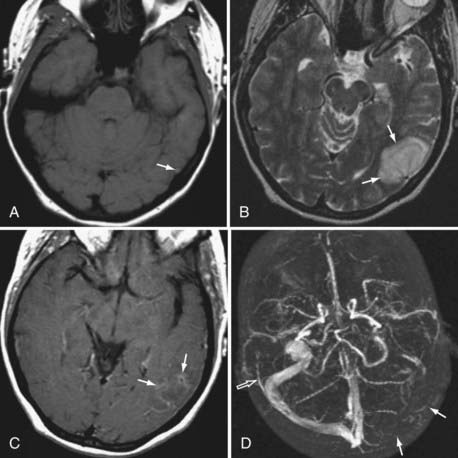
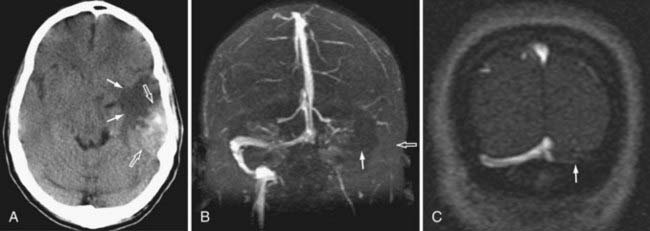
Because the clinical features are highly variable and the symptoms are usually nonspecific, the key to making the diagnosis of CVT is to have a high level of suspicion. Historically, CVT was first documented radiographically after direct injection of the superior sagittal sinus.21,24 Diagnostic modalities currently used for the confirmation of CVT include computed tomography (CT), magnetic resonance imaging (MRI), and cerebral angiography (Figs. 357-1 to 357-4).
CT is usually the initial diagnostic test performed on patients suspected of having CVT or those exhibiting acute deterioration in mental status.21,24 The dense vein and cord sign may be seen in approximately 20% of patients on standard non–contrast-enhanced head CT.30,44,45 The cord sign and the dense triangle sign correspond to spontaneously hyperdense cortical veins or sinuses, respectively. They can be seen during the first 1 to 2 weeks after thrombosis and may be falsely positive in neonates, dehydrated individuals, and those with elevated hemoglobin. Sometimes a dense triangle, also known as the delta sign, may be seen as the thrombus occupies the superior sagittal sinus. On contrast-enhanced CT, the empty delta sign consists of peripheral dural leaf enhancement along with a central nonopacified thrombus; it occurs in 10% to 30% of patients with superior sagittal sinus thrombosis.46–49 Unfortunately, the false-negative rate for the CT diagnosis of CVT is high, estimated at between 4% and 25%. CT can also show hemorrhagic infarctions as a result of poor drainage secondary to CVT. Such infarctions are usually bilateral (see Figs. 357-1 to 357-4).
MRI has recently become the modality of choice for detecting CVT.41,50–54 With magnetic resonance angiography (MRA) and magnetic resonance venography (MRV), the arterial and venous phases can be examined concomitantly or separately. MRA/MRV is now the best method for detecting CVT. MRI offers certain advantages: the thrombus can be directly visualized, and cortical lesions such as edema and hemorrhagic infarction can be detected. These MRI changes are best seen with thrombosis of the superior sagittal sinus, transverse sinus, straight sinus, and vein of Galen; they are far less obvious with thrombosis of the cavernous sinus and cortical vein, which sometimes remain difficult to diagnose. Although MRA/MRV is the most sensitive modality for detecting CVT, it may give inaccurate results in some circumstances. False-positive identification may occur when the sinuses are congenitally absent or hypoplastic. False-negative identification may occur when the signal of methemoglobin mimics that of flowing blood, when loss of signal occurs secondary to magnetic susceptibility artifact, or when the patient cannot cooperate and the study is technically poor (see Figs. 357-1 to 357-4).
Although traditionally considered to be the standard in diagnosing CVT,55 cerebral angiography is now indicated only in cases in which the MRI diagnosis is uncertain or when intervention is desired. The typical finding is nonvisualization of all or part of a sinus during the venous phase of an angiogram. In cortical vein thrombosis, there is a sudden nonvisualization of the occluded vein, which may be surrounded by dilated collateral “corkscrew vessels.“21
The value of conventional transcranial Doppler ultrasonography was examined by Canhao and colleagues.56 It was suggested that using transcranial ultrasound to detect the increase in velocity in the deep middle cerebral vein and basal vein of Rosenthal aided the diagnosis of superior sagittal sinus thrombosis. Others have stated that ultrasonography is of little benefit.57 Given the prevalence and ease of MRI in this era, ultrasonography is of limited value.
Treatment
Therapy for patients with CVT should be directed at treating the underlying causative process, symptoms secondary to elevated intracranial pressure, and seizures or focal deficits caused by cerebral edema and infarction. If an underlying cause is found, it should be treated. If an infectious process is identified, broad-spectrum antibiotics or drainage of purulent collections should be part of the treatment.21,24 Patients with CVT should initially be stabilized with appropriate airway and circulatory management. Subsequent supportive measures should be instituted. Increased intracranial pressure can be treated with osmotic agents (mannitol, hypertonic saline), temporary short-term hyperventilation, drainage of cerebrospinal fluid by ventriculostomy or lumbar puncture, barbiturate coma, or surgical craniectomy.21,24,58 Cerebral perfusion pressure should be kept at an adequate level to prevent secondary ischemic insults. Seizure is a frequent symptom and should be treated with anticonvulsants.
Antithrombotics
The natural course of CVT is variable, and the guidelines directing treatment are controversial. The use of heparin for the treatment of CVT was initially reported by Stansfield in 1942.59 Since then, several other authors have reported beneficial effects of heparin in patients with CVT,13,14,60 but there has been only one prospective, randomized, controlled study using heparin. Einhaupl and colleagues published the results of their series of 20 patients in 1991.61 The efficacy of systemic heparin was compared with that of placebo in a double-blinded, randomized study. The group of patients receiving heparin had a better outcome at 3 days, 8 days, and 3 months. Although the power of this study was reduced because the investigators did not meet all the criteria for a double-blinded, randomized study, the advantage of heparin in treating CVT was strongly suggested.
Another randomized, placebo-controlled trial looking at systemic anticoagulation was performed by de Bruijn and Stam.62 Sixty patients were randomized to receive either subcutaneous heparin or placebo for 3 weeks, followed by 3 months of oral anticoagulation. No patients were lost to follow-up. Although their study failed to show statistical significance, there was again a trend toward better clinical outcome in patients treated early with systemic anticoagulation.
Despite the risk for intracerebral hemorrhage, the benefit of using systemic heparin was examined in a large retrospective study by Ameri and Bousser.21 Their 82 patients were treated with heparin for CVT, and no mortality or worsening of clinical status was found. This has also been corroborated by other studies.62
Levine and associates found that patients treated with anticoagulation and antibiotics for cavernous sinus thrombosis in the early stage (<7 days after initial onset) had significantly less morbidity than did patients treated with antibiotics alone.63 However, if anticoagulant treatment began at a later stage of the disease, no beneficial effect was found.
The current trend is to use heparin.21,27,64 The goal of heparin anticoagulation is to maintain the activated partial thromboplastin time at 2 to 2.5 times normal. Once the patient’s condition has stabilized, warfarin therapy is initiated. There are few scientific data or guidelines on the dosage and duration of heparin and warfarin therapy in the literature on CVT. If no underlying cause of the CVT is found, the therapeutic international normalized ratio is kept between 2 and 3 for 6 months; lifelong therapy is warranted in patients with hypercoagulable disease states.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree