Cervical Laminoforaminotomy
Sadashiv Karanth
Ronald I. Apfelbaum
Daniel R. Fassett
Cervical radiculopathy occurs most commonly as a result of compression upon the preganglionic nerve root due to cervical spondylosis with uncovertebral osteophyte hypertrophy encroaching upon the neural foramina. Soft disk herniations, including extruded fragments of nucleus pulposus behind the posterior longitudinal ligament and disk bulges contained by the posterior longitudinal ligament, are also potential causes for cervical radiculopathy.
The majority of patients with cervical radiculopathy will respond to conservative treatments without the need for surgical intervention. Surgery, typically involving decompression of the nerve root, may be considered in patients with symptoms refractory to conservative treatment or in patients with significant or progressing neurologic deficit without prior conservative treatment. Of the surgical options for nerve root decompression, posterior cervical laminoforaminotomy, as was originally described by Scoville et al. (1) in 1951, is a good surgical option for the treatment of cervical radiculopathy. Description of the technical aspects of this procedure, along with its advantages and disadvantages, and comparison to other options for cervical nerve root decompression are discussed in this chapter.
INDICATIONS/CONTRAINDICATIONS
Radiculopathy most commonly presents with pain or paresthesias in a dermatomal or myotomal distribution of the irritated nerve root. Weakness can also occur within the nerve root distribution. Radiculopathy is commonly single level, but there is potential for multilevel nerve root irritation in some patients. Coexistent myelopathy is not uncommon in association with radiculopathy, and symptoms of myelopathy can often be underappreciated by the patient.
Physical examination of the patient with suspected radiculopathy includes a range of motion of the neck and neurologic assessment. Patients with cervical radiculopathy will often guard against neck extension and lateral bending to the side of the radiculopathy as these maneuvers reduce foraminal size and further compress an already irritated nerve root. Spurling’s maneuver, with head extension and lateral bending ipsilateral to the radicular symptoms and simultaneous axial compression upon the head by the examining physician, will often reproduce pain in a radicular distribution.
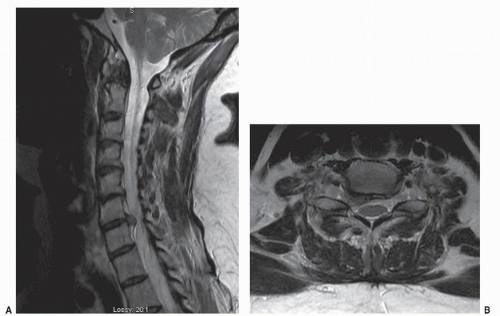
Conservative treatment should be considered prior to evaluation with imaging studies for patients with radicular pain without significant neurologic deficit. Nonsteroidal anti-inflammatory drug (NSAID) medications, analgesics, oral steroids, physical therapy, and cervical traction are all treatment options. A significant number of patients will have resolution of their symptoms with these treatments and therefore do not need a costly imaging study performed. In patients with symptoms refractory to conservative treatment, or those with significant motor weakness, further evaluation with imaging studies is indicated. Magnetic resonance imaging (MRI), or computed tomographic myelography in patients that cannot have MRI imaging, is done to evaluate the location, degree, and cause of neural compression (Fig. 75.1). Plain imaging of the cervical spine including dynamic flexion/extension images are often also useful and should be considered in the patient’s evaluation. Patients with concordance between symptoms, physical examination, and imaging findings do not need further studies. Nerve conduction studies and electromyography may be considered in patients with nonconcordant findings to better differentiate the source of their symptoms. Further conservative treatment options may include epidural or periradicular steroid injections, chiropractic treatment, and acupuncture.
In patients in whom radicular pain or weakness persists or progresses despite conservative treatment, surgical decompression of the nerve root may be considered. Posterior cervical laminoforaminotomy is an option to treat many of these patients with refractory root compromise due to both “hard disks” (osteophytes) and “soft disks” (herniations of the nucleus pulposus) as long as the compression is located laterally in the spinal canal or in the neural foramen. Some case series have suggested that hard disks do not have a favorable outcome with laminoforaminotomy (2). Other surgical options may include anterior approaches with or without fusion and more extensive posterior decompressions with or without fusion. Cervical total disk arthroplasty has also become an option for treatment of cervical radiculopathy (3).
Relative contraindications for posterior laminoforaminotomy include the presence of myelopathy, cervical kyphosis, and a significant component of neck pain. Spinal cord compression occurring with myelopathy is typically better addressed by a full canal decompression either posteriorly with complete bilateral laminectomy or an anterior approach involving discectomy or corpectomy with full resection of the marginal osteophytes to decompress the spinal cord and the nerve roots via an anterior foraminotomy. In the presence of cervical kyphosis, cervical laminoforaminotomy is not favored due to potential for aggravation of the kyphosis with disruption of posterior supporting structures with this procedure. Patients with a significant component of neck pain and advanced spondylosis should be counseled that neck pain may increase after this procedure, and alternatives involving arthrodesis or arthroplasty may be favored.
PROCEDURE
POSITIONING
Sitting and prone are the two most common positions used for posterior cervical laminoforaminotomy, but other positions like the lateral decubitus have been described. In the prone position (Fig. 75.2), the patient is carefully placed prone typically upon gel rolls with the head in three-pin fixation within a Mayfield head holder. A slight bend in the bed with the knees flexed can promote venous return in the distal lower extremities. The head is positioned in a flexed posture to widen the intralaminar space to facilitate decompression between the lamina. Neck flexion is limited, due
to potential for endotracheal tube kinking, to a position that allows two fingerbreadths between the chin and the chest. Some reverse Trendelenburg adjustment to the bed bringing the operative site above the level of the heart can improve venous return and reduce bleeding. However, the surgeon and anesthesiologist must consider the possibly of air embolism as the surgical site is raised above the heart.
to potential for endotracheal tube kinking, to a position that allows two fingerbreadths between the chin and the chest. Some reverse Trendelenburg adjustment to the bed bringing the operative site above the level of the heart can improve venous return and reduce bleeding. However, the surgeon and anesthesiologist must consider the possibly of air embolism as the surgical site is raised above the heart.
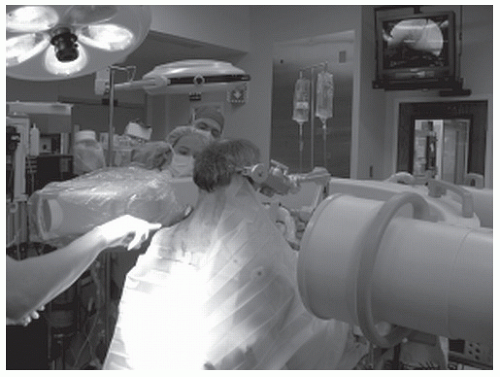
To prepare for the sitting position, the patient is initially placed in the supine position upon the operating table and the Mayfield head holder is affixed to the patients head, but not attached to the bed frame. The operating table is gradually adjusted to the sitting position with the back at approximately 90 degrees in relation to the floor. The attachment frame for the Mayfield is placed over the patients’ waist, and the Mayfield is secured to the frame with the patients’ head in a flexed posture. The C-arm is arced in front of the patient for a lateral image (Fig. 75.3). During the procedure, the surgeon is typically seated behind the patient using an operating chair. A narrow table (we use an instrument stand that has been modified so that the top is a 3 by 18 inch plate that is padded and draped) can be positioned within the sterile field in front of the operating chair to allow the surgeon to rest his or her arms to reduce fatigue.
Advantages of the sitting position, in comparison to the prone position, include improved fluoroscopic imaging as the patients’ shoulders tend to fall with gravity facilitating better radiographic visualization of the lower cervical spine, improved venous return that reduces venous bleeding during surgery, improved access to the patient by the anesthesiologist, and improved patient ventilation since they are not lying on their chest. Disadvantages of the sitting position include increased risk for air embolism, issues with surgeon arm fatigue, and the need to change the usual setup of the operating microscope to effectively utilize it in a horizontal position parallel with the floor. When using the sitting position, the anesthesiologist should place a precordial Doppler detector, and end-tidal carbon dioxide should also be monitored for early detection of air embolism. These modalities are very sensitive in detecting even minute amounts of entrained intravascular air. Air embolization is a very rare occurrence, but if it is detected, the anesthesiologist should notify the surgeon and elevate the venous pressure by increasing positive end-expiratory pressure or jugular vein compression. This will reveal the source of the entrainment and allow the surgeon to eliminate it, typically with bipolar cautery or bone wax. Intracardiac catheters, previously recommended prior to such sensitive detection devices, to allow aspiration of the air are no longer used as the air initially detected does not remain in the heart, and the above maneuvers will stop further entrainment of air before it becomes hemodynamically significant.
APPROACH
Intraoperative confirmation of the level is performed with either fluoroscopy or lateral x-ray. Fluoroscopy is beneficial in guiding the opening to avoid unneeded soft tissue injury of a more extensive exposure. The use of a K-wire to mark the level is discouraged as it may inadvertently enter the spinal canal between the lamina and injure the spinal cord. Midline exposure of the spinous process, lamina, and facets can be utilized, or a lateral muscle-splitting technique may be used. It is important to note that the cervical spinous process projects caudally, and the corresponding facet joint is at least a centimeter rostral to the tip of the spinous process. Hence, midline incision should be made a level above the corresponding spinous process to expose the desired foramen. A perfect midline incision through the avascular midline plane can limit blood loss in midline exposures. When the spinous process is identified, subperiosteal dissection is carried laterally to the medial aspect of the facets. For a single-level foraminotomy, a longitudinal incision of about 4 cm in length in the midline is often needed to facilitate the amount of lateral retraction to expose the medial facet. It is important to preserve the supraspinous as well as the interspinous ligaments to maintain stability of the posterior tension band. The dorsal musculature is retracted laterally and can be held in position by a number of commercially available retractors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree