38 Cervical Open Reduction Techniques: Anterior and Posterior Approaches
I. Key Points
– Cervical facet dislocations result from high-energy traumatic forces transmitted through flexion/distraction vectors.
• A flexion, rotational, and lateral force can result in a unilateral jumped facet.
• If the mechanism of injury involves flexion/compression forces (e.g., diving headfirst into a shallow pool), then facet and vertebral body fractures may be encountered in the form of jumped and/or perched facets.
• A severe flexion/distraction injury with a compression component is also called a teardrop fracture.
– Rule of thumb: A unilateral jumped facet results in 25% displacement (anterolisthesis) of one vertebral body on another (as seen on lateral plain radiographs or computed tomography [CT] scan of the cervical spine); bilateral jumped facets are associated with a 50% anterolisthesis.
– Acute management usually consists of reduction of the dislocated joints and the realignment of fractured cervical segments, through either open surgical intervention or axial cervical traction.
– Re-creating the force vectors of the mechanism of injury can facilitate reduction of the facets or deformity and realign the spine. For example, the cervical spine is flexed and distracted to realign the facets if the mechanism of injury was flexion/distraction.
– The open anterior approach provides for the removal of extruded disc prior to reduction of a dislocated facet. This approach may also be effective for reducing fractures and dislocations.
– Posterior instrumentation reestablishes the posterior tension band and provides the optimal environment for fusion.
II. Indications
Cervical open reduction can restore spinal alignment, decompress the neural elements, and establish rigid internal fixation.
– Cervical open reduction is indicated when:
• Decompression of neural elements is required
• Closed reduction fails
• Contraindications for closed reduction
 Patient with altered mental status
Patient with altered mental status
 Skull fracture precluding tong placement
Skull fracture precluding tong placement
 A relative contraindication is a rigid spine such as in ankylosing spondylitis.
A relative contraindication is a rigid spine such as in ankylosing spondylitis.
III. Technique
Anterior Approach
– Neuromonitoring (somatosensory evoked potentials [SSEPs], motor evoked potentials [MEPs]) allows monitoring of spinal cord function during spinal manipulation.
– Localization of the cervical level is possible using fluoroscopy or plain radiographs.
• Anatomic localizing
 C5-C6 disc space: level of the cricoid cartilage
C5-C6 disc space: level of the cricoid cartilage
 C3-C4 disc space: 1 cm above level of cricoid cartilage
C3-C4 disc space: 1 cm above level of cricoid cartilage
– If a herniated disc is compressing the neural elements, a complete discectomy is performed prior to anterior reduction.
• Blunt dissection: Retract carotid sheath laterally and trachea/ esophagus medially with retractors to expose anterior spinal column. The anterior longitudinal ligament (ALL) is typically disrupted as a result of trauma.
• Dissect longus colli laterally with monopolar cautery to expose the cervical vertebrae.
• In unilateral dislocations, the superior vertebral body will be rotated away from the side of dislocation.
• The annulus is incised with a scalpel as far laterally as possible to the uncovertebral joints.
• The disc and posterior longitudinal ligament (PLL) are removed with curettes and with Kerrison and pituitary rongeurs until the dura is visualized. The PLL may be ruptured, particularly with bilateral dislocation.
– Caspar retractors are placed, with pins one level above and below the subluxed and dislocated segments.
• Angulate pins convergently to place the spine in kyphotic (flexed) posture for distraction.
• Distract Caspar pins; the superior body will rotate back and become flush with the inferior body (Fig. 38.1).
– Once the desired spinal alignment is achieved, a tricortical bone graft harvested from anterior superior iliac crest or allograft is used for arthrodesis.
– Anterior plate placement: screws anchoring the plate should be in the middle third of the vertebral body to avoid violation of end plates.
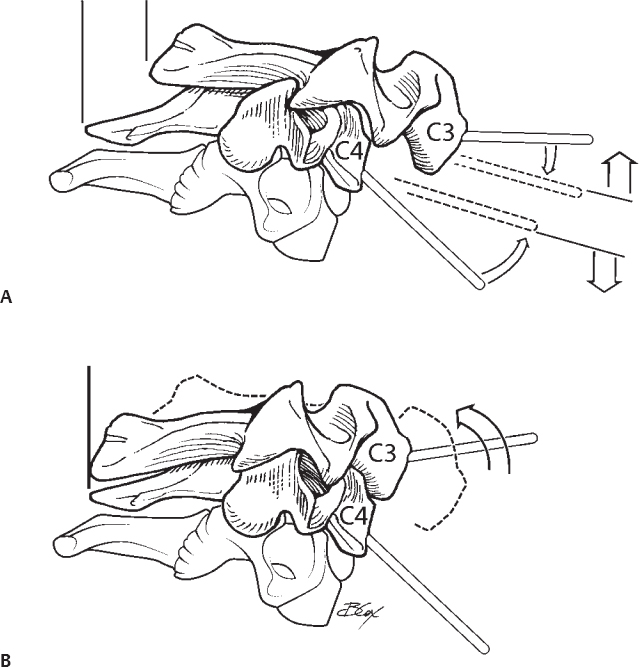
Fig. 38.1 (A,B) Anterior spinal reduction using convergently placed Caspar pins. Distracting the Caspar pins flexes and distracts the spine, unlocking the facets and reducing the spine.
Posterior Approach
– More commonly used when there is disruption of the posterior ligamentous complex and associated facet fractures preventing closed reduction
– Prone position in Mayfield head holder (Schaerer Mayfield, Randolph, MA) or Gardner-Wells tongs, and make a midline incision
– Perform subperiosteal dissection during exposure of laminae and lateral masses.
– Reduction can be performed with direct distraction using two towel clips in opposite directions on the spinous processes using a leveraging mechanism (Fig. 38.2).
– Alternatively, the superior articulating process of the inferior facet can be drilled away to facilitate reduction.
– Once decompression and reduction are achieved, the spine is locked into place using either lateral mass screws and rods or posterior wiring techniques.
– Decortication of the facets and supplemental bone graft placement in the lateral gutters help with arthrodesis.
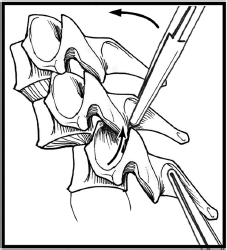
Fig. 38.2 Posterior spinal reduction using two towel clips. The inferior articulating facet of the superior vertebral body is lifted above and over the superior articulating facet of the inferior vertebral body, reducing the spine.
IV. Complications
– Wound infection (increased likelihood in trauma population)
– Graft donor site pain from autograft. Allograft bone is an alternative but may have a lower fusion rate.
– Anterior exposure may result in injury to the recurrent laryngeal nerve.
– Esophageal perforation
– Carotid artery and vagal nerve injury due to violation of the carotid sheath
– Horner syndrome: the sympathetic chain lies adjacent and anterior to the longus colli muscles.
– Damage to vertebral artery during posterior fixation
– CSF leak (which may be present from original trauma)
– Delayed fusion increases likelihood of screw loosening, plate migration, graft migration, and ultimately construct breakage.
V. Postoperative Care
– Immobilization for 6 weeks
– Serial radiographic examination: AP, lateral, swimmer’s views
– Flexion-extension views for assessment of stability
VI. Outcomes
– Kwon et al did a prospective randomized controlled trial comparing anterior and posterior fixation for unilateral cervical facet injuries and reported equal efficacy between the two techniques.1
– Johnson et al reported a 13% incidence of loss of postoperative radiographic alignment during follow-up of cervical facet fracture-dislocations treated with only anterior decompression and fusion.2
– Reindl et al reported on 41 consecutive patients with unstable dislocations/subluxations, of whom 8 required anterior reduction after failure of Gardner-Wells traction; in addition, 2 of those 8 failed, requiring posterior surgery as well.3
– Fehlings et al reported on 44 consecutive patients treated with posterior cervical fusion for traumatic instability. Long-term follow-up revealed that the cervical spine was successfully stabilized in 93% of cases.4
VII. Surgical Pearls
– Best treated anteriorly: large disc herniation with cord compression such that spinal cord can be decompressed prior to distraction
– Best treated posteriorly: hyperflexion injury, including PLL injury, unilateral and bilateral facet dislocation without anterior cervical disc herniation
– Anteriorly, avoid overdistraction of the cervical spine during placement of the interbody graft. Due to the ligamentous laxity prevalent in spinal injury, it is easy to overdistract.
– Posteriorly, be mindful of laminar fractures during exposure. Heat from a Bovie cautery can damage the spinal cord or cause CSF leaks when transmitted through fractured laminae.
Common Clinical Questions
1. When should anterior reduction be utilized when closed reduction is not possible?
2. When should open reduction be performed?
3. Postoperatively after anterior cervical discectomy with fusion, the patient has a hoarse voice and difficulty swallowing. What should the clinician be concerned about?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







