Cervical Spinal Infections
Choll W. Kim
Bradford L. Currier
John G. Heller
Frank J. Eismont
Advances in infectious disease management, radiologic imaging, and surgery during recent decades have dramatically improved the prognosis of patients suffering from spinal infections. Before antibiotics were available, the mortality rate of patients with neurologic compromise secondary to tuberculous spondylitis was nearly 60% (1). Today, fewer than 5% of patients similarly affected die of the disease (2,3). Despite this encouraging statistic, spinal infections may still lead to devastating consequences. Infections do not involve the cervical region as frequently as they involve the thoracic or lumbar spine. However, cervical infections have the highest rate of neurologic compromise and the greatest potential for causing disability. Prompt evaluation and treatment are essential when a cervical spine infection is suspected.
EVALUATION OF THE PATIENT WITH A CERVICAL SPINE INFECTION
CLINICAL PRESENTATION
The clinical presentation of a patient with a spinal infection depends on the cause of infection, the pathogenic features of the organism, and the anatomic compartment of the spine that is affected. Neck pain remains the most common symptom of spinal infection. In vertebral diskitis-osteomyelitis, neck pain is present in more than 90% of patients (4). The pain frequently radiates to the trapezius region and the shoulder. Fraser et al. (5) suggested that a patient with a subdural abscess presents similarly to one with an epidural abscess, except often there is no spinal percussion tenderness. Only one-third of patients with subdural abscesses complained of spinal tenderness (6). However, not all patients with an epidural abscess have spinal tenderness, making that feature unreliable for distinguishing the two disorders (7,8). Unilateral neck pain with radiculopathy may represent an infection of the cervical facet. Although rare, they are often found together with an epidural abscess (9). In contrast to infections in other areas of the body where fever is a common initial sign, patients with spinal infections are often afebrile. Only about 50% of patients with acute osteomyelitis have a fever (10).
Torticollis also may be present (11,12). In underdeveloped countries with a high incidence of tuberculous infections, one study reported that torticollis was present in 45% of patients with subaxial involvement (13) and five of six patients with atlantoaxial disease (14). Nuchal rigidity may occur in patients with an epidural abscess, meningitis, and/or intramedullary spinal cord abscess (15). Torticollis may also be caused by Grisel’s syndrome. Grisel’s syndrome results from a wide variety of inflammatory conditions including upper respiratory tract infection, sinusitis, tonsillitis, otitis media, parotiditis, mastoiditis, acute rheumatic fever, and others (16, 17, 18, 19, 20, 21, 22 and 23). If atlantoaxial rotatory deformity has occurred, the patient’s head is rotated away from the ventrally displaced C1-C2 joint and tilted toward the involved side (24). The patient may be able to increase the deformity actively but cannot overcome the torticollis beyond the neutral position. Attempts to correct the deformity are painful (16,25, 26, 27 and 28). The sternocleidomastoid muscle on the side opposite the tilt may be in spasm as if attempting to correct the deformity (26,27,29). On palpation, the C2 spinous process may be prominent and deviated to the side to which the chin is pointed, secondary to the lateral tilt of the head (25,26,30) or from counterrotation of C2 in an attempt to realign the head (20,31). This phenomenon is known as Sudeck’s sign (25,32), although it was described in 1907 by Corner (25), who also pointed out that the prominence of the C2 spinous process is due to flexion and forward displacement of the head. Neurologic complications are fortunately uncommon (16, 17 and 18,20,23,33, 34 and 35).
Atypical symptoms, such as headache, chest pain, dysphasia, meningeal irritation, or respiratory problems, occur in about 15% of cases (10,36,37). Rarely, patients present with signs of septicemia (38). In patients with chronic disease, signs and symptoms such as fever, axial pain, and spine tenderness may be lacking (8,15,39, 40, 41 and 42).
The rate of neurologic deficits is higher in the setting of cervical spine lesions than in other regions of the spine. Weakness and paralysis may not develop for many months, or they may occur suddenly and unpredictably in a matter of hours (40,43). Neurologic deficits occur in about 17% of all patients with vertebral osteomyelitis (10). However, Stone et al. (44) found that more than half of their cases of cervical osteomyelitis included neurologic
deficits while 82% of the patients in the series by Eismont et al. (45) were paralyzed. Initial presentation of neurologic deficit is more common in patients with an intramedullary spinal cord abscess. In patients with intramedullary spinal cord infections, 88.9% will present with weakness and 47.7% with sensory loss, but only 25.6% will present with fever, according to one series (46). Predisposing factors for paralysis include diabetes mellitus, rheumatoid arthritis, increased age, systemic steroid therapy, and a more cephalad level of infection (10,45,47).
deficits while 82% of the patients in the series by Eismont et al. (45) were paralyzed. Initial presentation of neurologic deficit is more common in patients with an intramedullary spinal cord abscess. In patients with intramedullary spinal cord infections, 88.9% will present with weakness and 47.7% with sensory loss, but only 25.6% will present with fever, according to one series (46). Predisposing factors for paralysis include diabetes mellitus, rheumatoid arthritis, increased age, systemic steroid therapy, and a more cephalad level of infection (10,45,47).
The nonspecific nature of neck pain as the presenting symptom, together with a paucity of fever and neurologic compromise as presenting signs, often leads to a delay in diagnosis. A literature review in 1979 showed that 50% of patients had symptoms for more than 3 months and only 20% were diagnosed within 3 weeks (10). Infants and intravenous drug abusers generally have a more acute presentation than other subgroups of patients (10,48, 49 and 50). Patients with epidural abscesses are initially misdiagnosed in about 50% of cases (43). For postoperative wound infections, the only symptoms may be fever and progressive neck pain out of proportion to the expected postoperative course. The wound may appear completely benign (51).
DIAGNOSTIC EVALUATION
The differential diagnosis of disk-space infection and vertebral osteomyelitis includes granulomatous infections, metastatic carcinoma, multiple myeloma, degenerative disease, trauma, fractures associated with osteoporosis, destructive spondyloarthropathy of hemodialysis (pseudospondylodiskitis), and Scheuermann’s disease (10,52, 53, 54 and 55). The diagnosis begins with a high index of suspicion. Thereafter, the most informative study remains magnetic resonance imaging (MRI) (40,56, 57, 58 and 59). It is noninvasive, safe, and ideal for visualizing the degree of cord compression and extent of the abscess.
Magnetic Resonance Imaging
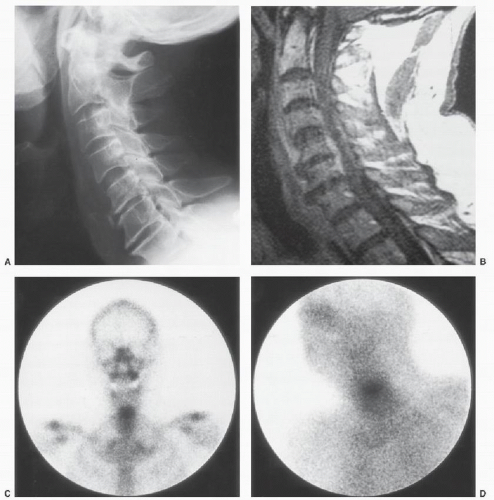
Use of MRI allows early diagnosis of infection and recognition of abscess formation without the risk of intrathecal injection that is present with computed tomography (CT) myelography (Fig. 58.1 and 58.1) (60,61). This study provides much more anatomic information than radionuclide studies, and results become positive at about the same time as a gallium scan (62). MRI has been shown to have 96% sensitivity, 93% specificity, and 94% accuracy in detecting vertebral osteomyelitis (62). Areas of infection appear as high signal intensity on T2-weighted images. On T1-weighted sequences, the signal intensity in the peridiskal area is decreased and the junction between the disk and the vertebral body is indistinct. On T2-weighted sequences, the signal intensity is higher than normal in the disk. Gadolinium, a paramagnetic contrast material, causes enhancement of the disk space and allows better delineation of epidural abscesses (63). The enhanced images allow localization of optimal sites for percutaneous biopsy and may distinguish active infections from those responding to treatment (63). In almost all cases, MRI allows distinction of tumor from infection. Tumors rarely involve the disk spaces and do not have the typical T1- and T2-weighted changes described for infection. Contiguous vertebral involvement is seen more frequently in infections than in tumors. Fat planes are often obscured diffusely as a result of edema in the setting of infection, whereas they are often intact or only focally altered by spinal tumors (64). The differential diagnosis of an epidural abscess also includes acute transverse myelitis (65). The findings of adjacent osteomyelitis suggest an epidural abscess, and multilevel or multiply loculated collections favor a diagnosis of subdural abscess (6). Imaging studies are generally not helpful in the diagnosis of postsurgical wound infections, and treatment should not be delayed while waiting for these studies to be performed.
Follow-up studies on treated infections may show a decrease in abscess size, but enhancement may persist in the disk or epidural space despite clinical improvement (66). This persistent enhancement may represent chronic granulation tissue or scar formation. Over time, the T1-weighted sequences revert from a hypointense signal in the vertebral body to a hyperintense fat signal, and the hyperintense signal on the T2-weighted sequence gradually diminishes. In the healed stage, the disk space is narrowed or obliterated and spontaneous fusion is common (67,68).
False-negative results may occur with nonenhanced MRI, especially with extensive abscesses that do not have discrete cephalad and caudad borders (40). MRI may also be falsely negative in patients with concomitant meningitis because the signal changes in the abscess may be similar to those in the infected cerebrospinal fluid (CSF) (61). Recently, a case of gouty tophus of the cervical spine was shown to mimic infection and thus should be considered in the differential diagnosis (69).
Other Imaging Modalities
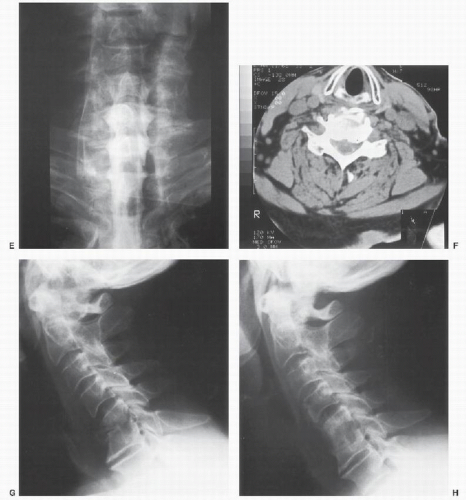
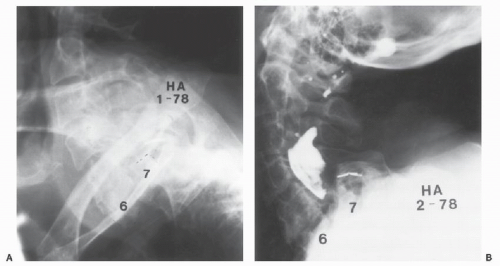
Plain radiographic findings are characteristic but are not evident until 2 to 4 weeks after the onset of the disease (70, 71, 72, 73 and 74). The earliest sign of infection is narrowing of the disk space and abnormal prevertebral soft tissue contours. Paraspinal soft tissue swelling is found in a third of patients with pyogenic infections compared with twothirds of the patients infected with tuberculosis (75). Destructive changes in the end plates and the ventral aspect of the vertebral body are present after 3 to 6 weeks (Fig. 58.1). The late changes seen on plain radiographs include reactive bone formation, fracture, collapse, kyphosis, and enlarging abscesses (10). The process may extend to adjacent levels; 79% of cases involve at least two vertebrae (71). The overall accuracy of plain radiographs is 74% (62).
Radionuclide studies allow detection of spinal infections earlier than plain films (62,76, 77 and 78). These studies provide a survey of the entire body and may detect multiple sites of infection, which occur in 4% of cases (62). Gallium scans show evidence of infection earlier in the course of the disease than technetium scans (76,79). Gallium scans are more useful for following the response to treatment because they become normal during resolution of the
infection; technetium scans remain positive for many months after the disease has resolved (80). A gallium scan may be slightly more sensitive than a technetium scan and has a slightly higher specificity than technetium scans alone (85% vs. 78%) (62,76,81). Single photon emission computed tomography (SPECT) is more sensitive and has better contrast resolution than planar scintigraphy; it also allows three-dimensional localization (82). Feiglan et al. (83) found the sensitivity of planar technetium scintigraphy to be 74% and gallium planar scintigraphy 69%, compared with 92% for SPECT scans. Indium scans are not particularly helpful in the evaluation of spinal infections because of low sensitivity. The specificity is 100%, but the sensitivity is only 17% and the accuracy 31% (84).
infection; technetium scans remain positive for many months after the disease has resolved (80). A gallium scan may be slightly more sensitive than a technetium scan and has a slightly higher specificity than technetium scans alone (85% vs. 78%) (62,76,81). Single photon emission computed tomography (SPECT) is more sensitive and has better contrast resolution than planar scintigraphy; it also allows three-dimensional localization (82). Feiglan et al. (83) found the sensitivity of planar technetium scintigraphy to be 74% and gallium planar scintigraphy 69%, compared with 92% for SPECT scans. Indium scans are not particularly helpful in the evaluation of spinal infections because of low sensitivity. The specificity is 100%, but the sensitivity is only 17% and the accuracy 31% (84).
CT imaging may be helpful in distinguishing infection from malignancy and in demonstrating the extent of bony destruction and the formation of soft tissue abscesses (85, 86 and 87). The soft tissue mass, frequently seen in the prevertebral area in infections, usually surrounds the spine ventrally, in contrast to neoplasms, which are more likely to have a partial paravertebral soft tissue mass or no extension beyond the vertebrae. Neoplasms are more likely to involve the dorsal elements than infections and may be osteoblastic compared with the osteolytic appearance of spinal infections (87).
When MRI is contraindicated, such as in patients with cardiac pacemakers, postmyelography CT should be considered in patients with neurologic signs or symptoms (Fig. 58.1F). Plain CT has a high false-negative rate, and in one study, it was diagnostic in only four of nine cases. Contrast-enhanced CT has been advocated by authors (88). Unfortunately, it may miss the area of interest unless a myelogram is performed in conjunction with the study. If pus is encountered during needle insertion, a specimen should be taken for culture, but the thecal sac should not be entered. A second puncture for myelography should be performed at a different level. CSF should be sampled at the time of myelography for cell count, glucose and protein measurement, and culture. Fraser et al. (5) noted that there is no major anatomic barrier in the subdural space; therefore, an abscess in this location could extend more easily than an epidural abscess. They believed that the myelographic finding of multiple defects favors a diagnosis of a subdural abscess over an epidural abscess (5,6,89,90). In contrast, the radiographic finding of osteomyelitis in association with a myelographic block favors a diagnosis of an epidural abscess because an infection in the subdural space is unlikely in association with vertebral osteomyelitis.
Laboratory Evaluation
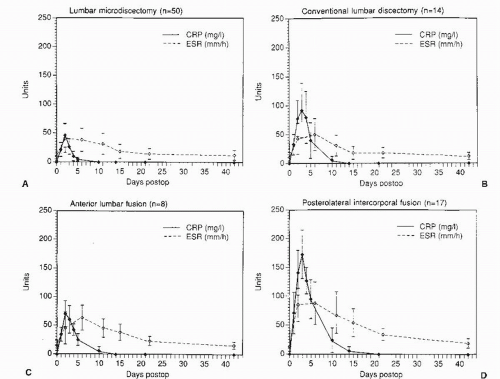
It is common to obtain laboratory studies concomitantly with advanced imaging evaluation. While most studies are nonspecific, certain laboratory tests aid not only in the diagnosis but also in monitoring the response to treatment. The white blood cell count is increased in only 42% of cases overall and is usually normal in patients with chronic infections (10,70). The erythrocyte sedimentation rate (ESR) is increased in more than 90% of patients (10). An increased ESR is not specific for infection, but it is a good screening test and is also useful for following the response to treatment (10,53,77,91,92). The C-reactive protein (CRP) value is a more sensitive method of evaluating a systemic inflammatory response. It has advantages over ESR in the evaluation and follow-up of patients with vertebral osteomyelitis since it increases more rapidly and has a much shorter half-life (31). CRP was discovered in 1930 by Tillett and Francis in their studies of pneumonia. This acute-phase protein is a 187 amino peptide that is able to precipitate the C-fraction polysaccharide from Strep-tococcus pneumonia (93). With the onset of an infection, or other inflammatory process, the CRP level increases within 4 to 6 hours, doubling every 8 hours, and peaking at about 36 to 50 hours (93). The half-life of CRP is 24 to 48 hours. The degree of increase can be up to 10,000-fold higher than normal, while ESR increases only 10- to 100-fold (94). The ESR begins to increase only several days after onset of infection and peaks at 7 to 8 days (93).
Blood cultures are positive in 24% of patients with pyogenic spinal infections (10). In patients with epidural abscesses, blood cultures are positive in 60% of cases, and cultures of spinal fluid yield the organism in approximately 11% of cases (8,41). Patients with chronic disease often appear to have fewer toxic responses, and the white blood cell count is normal (15).
The ESR and CRP values are normally increased in the early postoperative period after uncomplicated procedures (Fig. 58.2) (95). In lumbar procedures, the CRP level peaks after 2 to 3 days and typically returns to normal 5 to 14 days after operation. The ESR peaks 5 days after operation and declines slowly and irregularly. Similar data for cervical spine procedures are not available. An ESR or CRP level that is higher than expected or rising after 3 to 5 days, respectively, is suggestive of infection. The white blood cell count is generally unremarkable (51).
Whenever a myelogram is performed, spinal fluid should be obtained for analysis. In most parameningeal processes, there is an increased protein level, a moderate pleocytosis, and a low to normal glucose level (5,6). Bacteria may be present in the CSF in 7% to 13% of cases in which the epidural abscess is complicated by meningitis or, more rarely, a subdural abscess (15,42,43,96).
Microbiology Evaluation
Despite the accuracy of MRI, an absolute diagnosis must be based on bacteriologic or histologic examination of the pathologic tissue (97, 98 and 99). The only circumstances in which the diagnosis may be made without a tissue biopsy include pediatric diskitis (rare in the cervical spine) and when a patient with signs and symptoms of spinal infection has a positive blood culture.
Needle biopsies can be performed safely throughout all regions of the spine (100,101). A definite diagnosis is possible with a percutaneous needle biopsy in 68% to 86% of cases (10,70,100,102, 103 and 104). A false-negative result of a needle biopsy often occurs in patients being treated with antibiotics at the time of the biopsy. Open biopsies have lower false-negative rates because the surgeon is able to select grossly abnormal tissue and to provide the pathologist with a larger tissue sample (10). In the cervical spine, open biopsy is often performed as part of the definitive surgical procedure.
It is not necessary to obtain specimens for cultures of a draining postoperative wound before taking the patient to the operating room if antibiotics can be withheld until after the operation. Exploration and debridement of the wound should be performed urgently, and tissue samples for cultures can be obtained at operation. If the wound appears benign but a deep infection is suspected, the wound can be aspirated to obtain a specimen for Gram stain and culture. After surgical preparation of the wound, a spinal needle can be advanced down to bone and the wound can be aspirated. If the tap is
dry, a new needle can be inserted in another quadrant of the wound and the procedure repeated until fluid is obtained for analysis. If all four quadrants of the wound produce dry aspirates, the examination is considered to have a negative result. The sensitivity and specificity of percutaneous aspirations of the cervical spine are not known. If signs of superficial infection are present, the deep aspiration is not performed until the superficial space is clean because the needle may contaminate the deep space.
dry, a new needle can be inserted in another quadrant of the wound and the procedure repeated until fluid is obtained for analysis. If all four quadrants of the wound produce dry aspirates, the examination is considered to have a negative result. The sensitivity and specificity of percutaneous aspirations of the cervical spine are not known. If signs of superficial infection are present, the deep aspiration is not performed until the superficial space is clean because the needle may contaminate the deep space.
During evaluation of a patient with a suspected cervical spinal infection, the spine must be protected and the patient’s neurologic status must be examined frequently. Infections in the cervical spine are more likely to lead to instability and neurologic compromise than involvement of the thoracolumbar region. A significant or progressive neurologic deficit is a surgical and medical emergency. If the spine is unstable, MRI-compatible Gardener-Wells tongs and cervical traction should be applied, and an MRI or CT should be obtained urgently. Definitive treatment is based on the severity of the disease, the anatomic location, and characteristics of the offending organism. The characteristics of various types of infections along with their recommended treatment strategies are described below.
PYOGENIC INFECTIONS
IATROGENIC WOUND AND DISK-SPACE INFECTIONS
Epidemiology and Etiology
The risk factors for a postoperative spinal infection include increased patient age, steroid therapy, malnutrition, cigarette smoking, poorly controlled diabetes mellitus, immunosuppression, rheumatoid arthritis, and preoperative hospitalization (59,105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115 and 116). Cruse and Foord (111) found that the infection rate doubles for each additional week that patients are hospitalized before operation. Measures that help decrease infection intraoperatively include double gloving, limiting traffic in the operating room (106), careful soft tissue handling, and periodic release of selfretaining retractors to allow reperfusion of muscle (117).
The prevalence of infection varies with the approach and the magnitude of the procedure. Compared to infection rates in the lumbar spine, cervical spine procedures tend to have less risk of postoperative infection. Espersen et al. (118) reported that infections developed in 1.8% of 1,106 patients treated with the Cloward technique by various graft types. A superficial infection occurred in 1% of cases, a deep infection in 0.27%, and a donor-site infection in 0.5%. The infection rate following anterior cervical diskectomy and instrumented fusion with a plate is also very low (119, 120 and 121). Tippits and Apfelbaum (121) found only one infection in 220 cases of ventral cervical plate fixation. The one infected case was managed with antibiotic therapy, and the hardware was retained.
Cervical spine infection due to esophageal or pharyngeal injury is a rare but dreaded complication of ventral cervical surgery. While the risk of esophageal or pharyngeal injury is exceedingly rare, ranging from 0.02% to 1.49%, its mortality may be as high as 20% (122,123). In a study of 44 patients presenting to a spinal cord injury center with esophageal perforations, 34 were related to the operations performed for cervical fractures, of which 28 patients had plate and screw fixation (122). The most frequently occurring clinical symptoms were neck and throat pain, odynophagia, dysphagia, hoarseness, and aspiration. The most common clinical findings were an elevated temperature, localized induration and neck tenderness, crepitus or subcutaneous air in the neck and ventral chest wall, an unexplained tachycardia, and blood in the nasogastric tube. Nearly all patients (42/44) underwent surgical repair of the esophageal injury and required an extended hospital stay (253 days). The perforation may occur during exposure of the spine (124), from the sharp edge of a bone graft (125), or from erosion of the wall of the esophagus from ventral hardware (126,127). Several case reports show that esophageal perforation can occur years after operation (126, 127, 128, 129, 130 and 131).
The infection rate after a dorsal cervical fusion ranges from 0% to 18% (112,114, 115 and 116,132, 133 and 134). With contemporary techniques using lateral mass screw-rod systems, the infection rate is about 5% (135, 136, 137 and 138). Patients with rheumatoid arthritis have high infection rates ranging from 5% to 18% (112, 113, 114, 115 and 116). Patients with Down’s syndrome also have a higher rate of infection (139). Revision surgery was associated with a high infection rate as well (140). In a randomized controlled trial of ventral versus dorsal surgery to treat unilateral facet fractures, Kwon et al. (141) showed that postoperative wound infection was higher for dorsal surgery.
Fusion to the occiput does not appear to increase the infection rate. McAfee et al. (142) described 37 patients who had an occipitocervical fusion without instrumentation. The infections only involved the donor site in two patients and halo pin sites in two. Instrumentation used to augment an occipitocervical fusion did not increase the risk of infection (143,144). Itoh et al. (145) reported one infection in 17 cases (6%) of occipitocervical fusion with Luque segmental instrumentation, but all the patients in that series had rheumatoid arthritis.
Transoral procedures once were associated with a high infection rate (146). Later series proved that infection rates were low when the oral approach was used for decompression only and antibiotics were given prophylactically (147, 148 and 149). Hadley et al. (148) reported only one infection in 53 transoral decompressions. Bone grafting through the transoral approach may increase the infection rate and has caused at least one fatality (148). Several successful case series have been reported (148,150), but McAfee et al. (142) prefer the ventral retropharyngeal approach. They had no infections in 15 cases of fusions performed through the retropharyngeal approach. The prevalence of infection after an extrapharyngeal approach to the subaxial cervical spine ranges between 0% and 2% (119, 120 and 121,142,151,152).
The use of minimally invasive techniques will likely decrease the infection rate even further. In a large series of patients, Fessler and coworkers studied 1,338 minimally invasive spinal procedures (153). The infection rate for simple decompression was 0.10%, for minimally invasive fusion was 0.74%, and the overall infection rate for the entire group was 0.22%. Of the 161 cervical spine decompression cases, there were no infections. Similarly, percutaneous procedures such as epidural steroid injections and diskograms are associated with a low risk of infection. Grubb and Kelly (154) showed that only 3 of 807 (0.37%) cervical injections led to an infection, while Zeidman et al. (155) in a large series of 4,400 diagnostic cervical injections reported that only eight patients became infected (0.18%).
Management
The principles of treatment of postoperative wound infections include (a) thorough irrigation and debridement, (b) appropriate antibiotic therapy, (c) proper nutrition and medical management, and (d) appropriate wound care. The management of postoperative diskitis is the same as the treatment for hematogenous disk-space infection and is discussed in a later section.
Treatment of a wound infection must be expeditious. The patient should be taken to surgery without undue delay, and the wound should be opened and explored. If the infection is superficial, the deep fascia can be left intact. Samples of the subcutaneous tissues should be cultured, and the tissues should be copiously irrigated and debrided. The fascia is then inspected for any signs of communication between the layers. If the fascia is intact and the patient does not have signs of septicemia, the subfascial plane can be aspirated and left undisturbed if the tap is negative (51). However, most surgeons believe it is necessary to open and debride the wound (one layer at a time) down to the bone in nearly all cases (156). All devitalized tissue should be removed from the wound. Bone graft that becomes loosened by irrigation or grossly infected should be removed as well. It is not necessary or desirable to remove all of the bone graft that is needed to achieve a solid fusion, although some cases may require replacement of bone graft from other sources (51,157, 158 and 159). If hardware is present, it should be left in place unless it has failed (51,110,157, 158, 159 and 160). Multiple debridements may be required to control the infection.
The technique and timing of wound closure are based on the nature of the infection, the appearance of the wound, the clinical response, and host risk factors. The options include (a) wound closure over drains in each layer, (b) open packing with delayed closure, and (c) open
packing with healing by secondary intention. The use of vacuum-assisted wound closure systems is popular in large, chronic wounds. Its application in difficult dorsal lumbar wound infections has been relatively safe and effective (161).
packing with healing by secondary intention. The use of vacuum-assisted wound closure systems is popular in large, chronic wounds. Its application in difficult dorsal lumbar wound infections has been relatively safe and effective (161).
Prognosis
The prognosis of a patient treated for postoperative infection is based on the nature of the infection, the health of the host, and the adequacy of treatment. Information on cervical infections is limited, and guidelines must be extrapolated from the literature on thoracolumbar infections. Massie et al. (156) described 22 patients with postoperative spinal infections. Five cases required reoperation and 10 cases were allowed to heal by secondary intention, but all wounds eventually healed. There were no cases of chronic drainage, osteomyelitis, or death. Stambough and Beringer (107) described 11 patients with deep infections, four with superficial infections, and four with iliac crest donor-site infections. The hardware was removed in 3 of the 11 patients with deep infections but retained in all other cases. Seventeen of eighteen patients achieved a solid fusion, and all but one infection eventually resolved.
HEMATOGENOUS VERTEBRAL OSTEOMYELITIS AND DISK-SPACE INFECTION
Epidemiology and Etiology
Hematogenous vertebral osteomyelitis may be caused by any condition that results in bacteremia. Infections of the urinary tract, soft tissues, or respiratory tract, as well as intravenous drug abuse, are all common causes (50). The cervical spine is involved in about 6% of cases of vertebral osteomyelitis (10,71). The incidence of cervical infection is higher in patients who are elderly or immunocompromised (37,53). Patients who are diabetic or human immunodeficiency virus (HIV) serology positive are particularly susceptible to the development of vertebral osteomyelitis (37,50). Similarly, intravenous drug users are at higher risk of diskitis-osteomyelitis (4,50,162).
Microbiology
Staphylococcus aureus remains the most common pathogen, accounting for 50% of all spinal infections (10). The most common gram-negative pathogens are Pseudomonas, Escherichia coli, and Proteus species, which are common causes of urinary tract infections (70,91,163,164). Pseudomonas aeruginosa is frequently identified as the organism responsible for vertebral osteomyelitis in IV drug abusers (50,165,166). Anaerobic infections are uncommon and generally are associated with open fractures, human bites, foreign bodies, or diabetes (10,167). Salmonella osteomyelitis is rarely encountered and has a tendency to infect sites of preexisting disease (74,168).
Pathogenesis
Disk-space infection and vertebral osteomyelitis once were thought to be distinct clinical entities. Because the clinical manifestations and treatment of septic diskitis and vertebral osteomyelitis are similar, it is best to consider them as related conditions in a spectrum of disease (169,170). The pathogenesis of neurocompromise associated with vertebral osteomyelitis may be related to direct compression by bone or disk, from spinal instability and deformity, or by epidural pus and granulation tissue. The neural tissue may also sustain ischemic damage from septic thrombosis or be impaired by inflammatory infiltration of the dura (10,77,98).
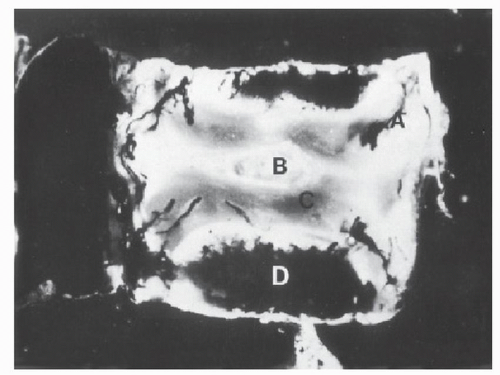
The nucleus pulposus receives nutrients from diffusion across the end plates and from the blood vessels in the annulus fibrosis (171,172). In the developing spine, the end plate has an orderly arrangement of cartilage canals that contain vascular organs resembling glomeruli (Fig. 58.3) (8,84). After birth, the cartilage end plates become progressively thinner, and by adulthood, most of the vessels of the cartilage canals are obliterated (133,173,174). In children, microorganisms have nearly direct access to the nucleus pulposus through the cartilage canals, allowing infection to begin spontaneously in the disk and then spread to adjacent bone. Pediatric diskitis is relatively common in the lumbar spine but rare in the cervical spine. In adults, hematogenous infection begins in the metaphysis and spreads across the disk by lysosomal destruction of the nucleus pulposus or through the annular vessels. Wiley and Trueta (175,176) demonstrated that bacteria could gain access to the metaphyseal region of adjacent vertebrae through these arteries and cause infection.
Evaluation and Treatment
The evaluation of a patient with diskitis-osteomyelitis is discussed in the previous section. Once a diagnosis
is established, the goals of treatment are to prevent or reverse neurologic deficits, to relieve pain, to establish spinal alignment and stability, to eradicate the infection, and to prevent relapses. Antibiotic therapy and surgery play a major role in the treatment of spinal infections, but attention to good general medical care is still a vital part of the treatment. Associated conditions that compromise wound healing or immune response should be managed aggressively. Proper nutrition and the reversal of metabolic deficits and hypoxia are essential. Diabetes and other systemic illnesses, including coexistent infections, should be brought under control (45).
is established, the goals of treatment are to prevent or reverse neurologic deficits, to relieve pain, to establish spinal alignment and stability, to eradicate the infection, and to prevent relapses. Antibiotic therapy and surgery play a major role in the treatment of spinal infections, but attention to good general medical care is still a vital part of the treatment. Associated conditions that compromise wound healing or immune response should be managed aggressively. Proper nutrition and the reversal of metabolic deficits and hypoxia are essential. Diabetes and other systemic illnesses, including coexistent infections, should be brought under control (45).
When possible, the choice of antibiotic agent should be determined by the culture and sensitivity test results so that the most specific and least toxic agent can be used. Antibiotic treatment should be withheld until an organism is identified by a biopsy in case a second biopsy is required. Patients who have systemic toxicity or neurologic deficit, however, should be treated with maximal doses of broadspectrum antibiotics as soon as the biopsy has been completed. Antibiotics should be administered parenterally for 6 weeks. Parenteral therapy for less than 4 weeks results in a higher rate of failure (10,45,71,91).
Inflammatory markers, such as CPR and ESR, are useful to assess the therapeutic response. The ESR can be expected to decrease to half to two-thirds of pretreatment levels by the completion of successful treatment (10,53,77,91,177). However, the ESR remains elevated for over 3 weeks postinfection (178). The CRP, in contrast, decreases more rapidly and often returns to normal levels in 10 days.
Surgical treatment is indicated in the following circumstances: (a) to obtain a bacteriologic diagnosis, (b) to drain a clinically significant abscess (spiking fevers and septic course), (c) to treat cases refractory to nonoperative treatment (persistently increased ESR/CRP or persistent pain), (d) to decompress neural elements in the presence of a neurologic deficit, and/or (e) to correct spinal deformity and/or instability (45,71,179,180). The timing of operation must be individualized. A progressive neurologic deficit or a clinically significant abscess is a surgical emergency, but most spinal infections can be managed in a less urgent time frame. In nearly all cases, the spine should be approached ventrally to provide direct access to the infected tissues and to allow adequate debridement. In cases of epidural extension, the posterior longitudinal ligament should be excised to ensure that the neural elements are decompressed and the infected tissue is removed. Infections in the cervical spine may lead to extensive bone destruction extending laterally to the foramen transversarium, placing the vertebral artery at risk during debridement (181). The risk can be higher if the vertebral artery is tortuous, which has been shown in cadaver studies to occur in 2.7% of cases (182). Ventral exposure allows stabilization of the spine by bone grafting, which promotes rapid healing without collapse and facilitates rehabilitation (45,183, 184, 185 and 186). Laminectomy is contraindicated in most
cases because it may lead to neurologic deterioration and increased instability (Fig. 58.4 and 58.4) (45,187,188).
cases because it may lead to neurologic deterioration and increased instability (Fig. 58.4 and 58.4) (45,187,188).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree