3 Cervical Spine
I. Key Points
– The subaxial cervical spine includes C3 to C7.
– The cervical spine normally demonstrates a lordotic curvature.
– Posterior instrumentation often uses lateral mass screws because the pedicles are narrower than in the thoracic and lumbar spine, increasing the risk of neurovascular injury.
– The size and volume of lateral masses decrease from the upper to lower subaxial cervical spine.
II. Bony Anatomy
– Radiographic landmarks1: C3 is at the hyoid, C4 is at the thyroid cartilage, and C6 is at the cricoid cartilage.
– Palpable landmark: the anterior tubercle of the C6 transverse process (Chassaignac tubercle) is palpable.
– The width of vertebral body is usually 17 to 20 mm.
– In the coronal plane, uncovertebral joints are noted at the anterolateral aspect of the vertebral body (Fig. 3.1).
– The spinal canal is triangular and has a greater lateral than anteroposterior (AP) dimension.
– The AP diameter of the spinal canal decreases caudally2: 17 mm at C3, 15 mm at C7.
– Lateral masses of the subaxial spine are composed of the superior and inferior articulating processes (the facet).
– A lateral mass begins lateral to where the lamina and pedicle meet.
– C7 is a transitional vertebra: the lateral mass is thinner and the pedicle is wider than in C3 to C6.
– The normal lordotic curvature of the cervical spine is 16 to 25 degrees.3
– Cervical disc herniation occurs most frequently at C5/6 and C6/7.
– Biomechanical studies show maximal flexion-extension at C4/5 and C5/6 and maximal lateral bending at C2/3, C3/4, and C4/5.
– The least mobile segment is C7/T1.
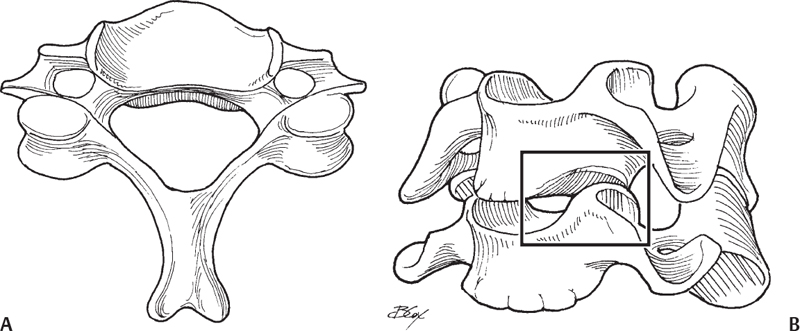
Fig. 3.1 Cervical vertebrae superior (A) and oblique (B) views.
III. Neural Anatomy
– C3 to C7 nerve roots exit above their corresponding level (e.g., C7 exits above the C7 pedicle).
– The C8 nerve root exits above the T1 pedicle.
– The cervical spinal cord enlarges caudally and reaches a maximal cross-sectional area at C6.
– Nerve roots enter the intervertebral foramina laterally, occupy approximately one-third of the foramina, and are covered by epidural fat and venous plexus above.
– Nerve roots exit the spine at a point that is anterolateral to the superior joint facet.
– The cervical plexus is formed by the anterior rami of C1 to C4.
– The brachial plexus is formed by the anterior rami of C5 to T1.
– The cervical plexus gives rise to (1) the ansa cervicalis (supplies a branch to the hypoglossal nerve and innervates the strap muscles, except for the thyrohyoid), (2) phrenic nerve (C3 to C5, but mainly C4), and (3) cutaneous nerves of the posterior head and neck.
IV. Vascular Anatomy
– Vertebral arteries usually originate from the subclavian artery and ascend between the anterior scalene and longus colli muscles.4
– Vertebral arteries enter the spine at the transverse foramen of C6 (occasionally at C7).
– Vertebral artery segments: V1 (pre-foraminal), origin to transverse foramen entrance; V2 (foraminal), C6 to C2; V3, C2 to dura; V4, intradural segment to basilar artery.
– The transverse foramen is lateral to the vertebral body and anterior to the nerve root groove.
– At C3 to C5, the lateral-most aspect of the transverse foramen is often anteromedial to the midpoint of the lateral mass.
– At C6-C7, a portion of the transverse foramen is often anterior to the midpoint of the lateral mass.
– Blood supply to spinal cord includes the anterior spinal artery, the two posterior spinal arteries, and the segmental medullary arteries.
– The anterior spinal artery originates from the vertebral arteries.
– The posterior spinal arteries originate from either vertebral arteries or the posterior inferior cerebellar arteries (PICA).
– Venous drainage of the spinal cord: three anterior and three posterior longitudinally running veins.
– Spinal cord is surrounded by an anterior and a posterior venous plexus.
– The anterior venous plexus is most pronounced medial to the pedicles.
V. Ligamentous and Muscular Anatomy
– The anterior longitudinal ligament covers anterior vertebral bodies and limits extension.
– The posterior longitudinal ligament covers posterior vertebral bodies and limits flexion.
– The interspinous and supraspinous ligaments run between adjacent spinous processes and form the ligamentum nuchae.
– The ligamentum nuchae makes up the midline avascular plane.
– The carotid triangle of the neck is an important surgical landmark for anterior approaches, formed laterally by sternocleidomastoid, superiorly by dorsal portion of the digastric, and anteriorly by omohyoid.
– The carotid triangle contains the carotid sheath (common carotid, internal jugular, and vagus nerve).
– Longus colli muscles lie anterolateral to vertebral bodies and are elevated during anterior spinal procedures (Fig. 3.2).
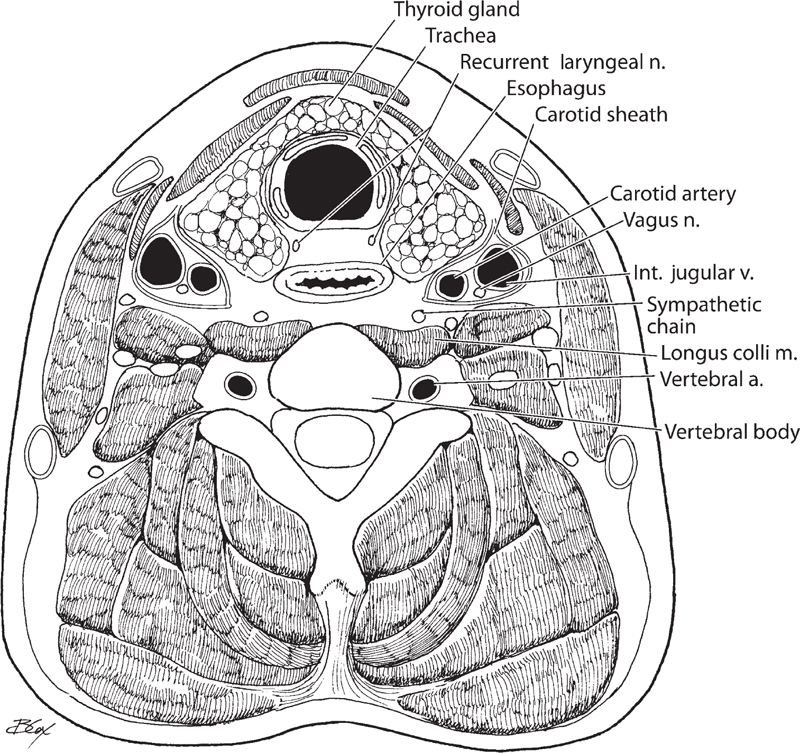
Fig. 3.2 Cross-section of the neck and spine at the C5 level.
VI. Surgical Pearls
– Uncovertebral joints provide several surgical landmarks: they define the lateral borders for corpectomy or discectomy, and they define the midline for cervical plate placement.
– The Magerl technique for lateral mass screw placement is used to avoid injuring the vertebral artery or nerve root. The drill is placed 1 mm medial to the midpoint of the lateral mass and is angled 25 degrees laterally and 30 degrees superiorly.
– During anterior procedures, instruments are most safely inserted into the lateral aspect of the canal.
– During posterior cervical procedures, the patient can be placed in a slight reverse Trendelenberg position to reduce venous engorgement.
– C7 is a transitional-level vertebra. For a posterior fusion involving C7, some surgeons advocate extending the fusion to T1 to reduce adjacent-level disease.
Common Clinical Questions
1. Where does cervical disc herniation most often occur?
2. What is the normal curvature of the cervical spine?
3. Which arteries provide the majority of blood circulation to the spinal cord?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







