43 Transpedicular Approach
I. Key Points
– Alternative posterior approach for anterior decompression avoids the morbidity associated with anterior (i.e., transthoracic, thoracoabdominal) approaches for neural decompression.
– Less extensive dissection required compared with other anterior approaches
– Particularly effective technique for soft thoracic disc herniations or intrapedicular lesions
– Not ideal for large calcified central thoracic disc herniations
II. Indications
– Soft central or lateral thoracic disc herniations, anterolateral calcified thoracic disc hernations
– Reduction of retropulsed fragment(s) in vertebral burst fracture
– Resection and/or biopsy of intravertebral/intrapedicular lesions
– Decompression of anterolateral spinal canal in the setting of tumor
III. Technique
– Patient is in prone position on Jackson table with gel rolls or frame.
– Neurophysiologic monitoring (transcranial motor evoked potentials and somatosensory evoked potentials should be considered)
– Fluoroscopy: Obtain multiple views for correct localization. Either count from the sacrum or obtain anteroposterior (AP) views counting ribs, having confirmed 12 rib-bearing segments preoperatively. For extremely obese patients, a marker can be placed preoperatively by interventional radiology with subsequent imaging to confirm marker as a viable reference point.
– Midline incision: ipsilateral erector spinae muscles dissected to expose lamina, facet complex, transverse process
– If instrumentation is required, exposure is increased to encompass the targeted segments.
– In the thoracic spine, the medial portion of the transverse process overlies the pedicle.
– If necessary, AP fluoroscopy can be used to localize the pedicle margins.
– The pedicle inferior to the targeted disc space is targeted (i.e., the T8 pedicle for a T7-T8 disc herniation).1,2
– At a minimum, a laminotomy is created adjacent to the targeted pedicle.
– The posterior cortex of the pedicle is opened with a high-speed drill. Sequential passage of curettes and/or high-speed drill is used to create a channel through the cancellous pedicle. The walls of the pedicle can be thinned to an “eggshell” thickness with the drill. Once the vertebral body is reached, a down-going curette can be used to safely fracture the medial wall of the pedicle laterally, exposing the lateral margins of the dura. The medial portion of the adjacent facet is resected and the superior wall of the pedicle is removed to expose the disc space.
– A Woodson elevator is used to carefully palpate the ventral epidural space to identify the lesion.
– For disc herniations, the disc space is entered just lateral to the dura. Disc material is removed with rongeurs. The high-speed drill is then used to create a cavity encompassing the disc space as well as the adjacent vertebral bodies (Fig. 43.1). The drill is angled to extend the cavity medially, maintaining a thin margin of disc annulus or posterior vertebral wall between the drill tip and the ventral dura. A small down-going curette is then used to gently push the disc herniation into the cavity, allowing removal with rongeurs.3
– Note that the ventral dura is not well visualized with this technique. For more centralized masses, an instrument such as a down-going curette is used to localize the mass by palpation. The curette is then used to push the mass into the cavity (Fig. 43.1).
– For retropulsed bone or tumor, more of the vertebral body is removed to create the cavity into which the epidural mass is pushed.
– For larger masses, a bilateral transpedicular approach can be used.
– With bilateral approaches, fusion should be considered.
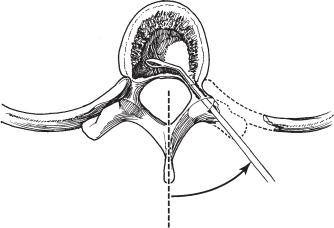
Fig. 43.1 To allow access to the interior of the vertebral body, it may be necessary to resect the rib, rib head, and transverse process. (From Vaccaro AR, Albert TJ, Spine Surgery: Tricks of the Trade 2nd ed, Thieme; pg. 89, Fig. 25.2.)
IV. Complications
– Infection
• Discitis
– Durotomy
• Pseudomeningocele formation
– Transient/permanent neurologic injury
• Spinal cord injury if excessive retraction is applied to the dura during the decompression
– Inadequate visualization of the ventral epidural space, resulting in suboptimal anterior decompression
V. Postoperative Care
– Consider neurologic intensive care unit for close monitoring, particularly for patients with preexisting neurologic deficit or significant comorbidities.
– Routine postoperative imaging is not required.
– Urgent MRI is needed if new neurologic deficit is present.
VI. Outcomes
– In properly selected patients, neurologic outcomes for symptomatic thoracic disc herniations treated by the transpedicular approach are similar to outcomes for the transthoracic approach.
VII. Surgical Pearls
– Review axial and sagittal images on computed tomography (CT) to understand the pedicular anatomy; may use three-dimensional reconstruction.
– When anatomy is distorted due to prior surgery or fusion mass, fluoroscopy and pedicle marker may be used to localize the pedicle as for pedicle screw placement.
– If anterior decompression is unsafe due to scarring with anterior dura or fragment indenting spinal cord, consider opening dura for adequate visualization of spinal cord in relation to the anterior pathology.
– Anterior unintended durotomy or cerebrospinal fluid (CSF) leak can be treated locally with Duragen (Integra Life Sciences Corp., Plainsboro, NJ) or Dura-Guard (Synovis, St. Paul, MN) and a sealant agent
– Postoperative lumbar drain should be considered with durotomy.
Common Clinical Questions
1. What is the main disadvantage of the transpedicular approach for anterior decompression?
2. A large central calcified disc herniation is best approached via which technique?
3. Is fusion necessary after a transpedicular approach?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







