Pain in the Back, Neck, and Extremities: Introduction
We include an extensive chapter on this subject in recognition of the fact that back pain is among the most frequent of medical complaints. Up to 80 percent of adults have low back pain at some time in their lives and, according to Kelsey and White, an even larger percentage will be found at autopsy to have degenerative spine disease. One task of the neurologist is to determine whether a disease of the spine has compressed the spinal cord or the spinal roots. To do this effectively, a clear understanding of the structures involved and some knowledge of orthopedics and rheumatology is necessary.
Pain in the Lower Back and Limbs
The lower parts of the spine and pelvis, with their massive muscular attachments, are relatively inaccessible to palpation and inspection. Although some physical signs and imaging studies are helpful, diagnosis often depends on the patient’s description of the pain and his behavior in different positions and during the execution of certain maneuvers. Seasoned clinicians appreciate the need for a systematic inquiry and method of examination, the descriptions of which are preceded here by a brief consideration of the anatomy and physiology of the spine.
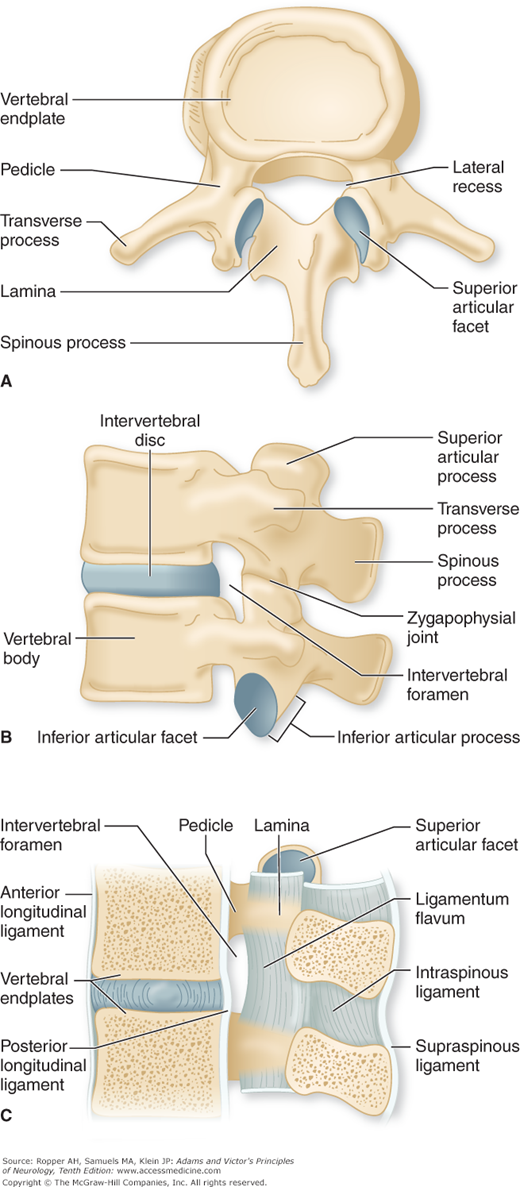
The bony spine is a complex structure, roughly divisible into an anterior and a posterior part. The anterior component consists of the cylindrical vertebral bodies, articulated by the intervertebral discs and held together by the anterior and posterior longitudinal ligaments. The posterior elements are more delicate and extend from the vertebral bodies as pedicles and laminae, which encircle the spinal canal. Large transverse and spinous processes project laterally and posteriorly, respectively, and serve as the origins and insertions of the muscles that support and protect the spinal column. The bony processes are also held together by sturdy ligaments, the most important being the ligamentum flavum, which runs along the ventral surfaces of the laminae. The posterior longitudinal ligament lies opposite it—on the dorsal surfaces of the vertebral bodies. These two ligaments define the posterior and anterior margins of the spinal canal, respectively.
The posterior parts of the vertebrae articulate with one another at the diarthrodial facet joints (also called apophysial or zygapophysial joints), each of which is composed of the inferior facet of the vertebra above and the superior facet of the one below. Figure 11-1 illustrates these anatomic features. The configuration and orientation of the facet joints differs in the cervical, thoracic and lumbosacral parts of the spine. The facet and sacroiliac joints, which are covered by synovia, the compressible intervertebral discs, and the collagenous and elastic ligaments, permit a limited degree of flexion, extension, rotation, and lateral motion of the spine.
Figure 11-1.
A. The lumbar vertebrae viewed from above from B. the side and C. mid-sagittally. A and B show the bony structures and their relationships to the disc space, facet joints and intervertebral foramina. C demonstrates in a cutaway mid-sagittal view, the main ligamentous structures of the spine in relation to the bones and discs. The ligaments and articulations are critical to the mechanical integrity of the spinal column.
The stability of the spine depends on the integrity of the vertebral bodies, pedicles and intervertebral discs and on two types of supporting structures, ligamentous (passive) and muscular (active). Although the ligamentous structures are quite strong, neither they nor the vertebral body–disc complexes have sufficient integral strength alone to resist the enormous forces that may act on the spinal column. Consequently, the stability of the lower back is also largely dependent on the voluntary and reflex activity of the paraspinal, sacrospinalis, abdominal, gluteus maximus, and hamstring muscles.
The vertebral and paravertebral structures derive their innervation from the meningeal branches of the spinal nerves (also known as recurrent meningeal or sinuvertebral nerves). These meningeal branches spring from the posterior divisions of the spinal nerves just distal to the dorsal root ganglia, reenter the spinal canal through the intervertebral foramina, and supply pain fibers to the intraspinal ligaments, periosteum of bone, outer layers of the annulus fibrosus (which enclose the disc), and the capsule of the articular facets. Coppes and associates have found A-δ and C pain fibers extending into the inner layers of the annulus, and even into the nucleus pulposus.
Although the spinal cord itself is insensitive, many of the conditions that affect it produce pain by involving these adjacent structures. For example, the sensory fibers from the lumbosacral and sacroiliac joints enter the spinal cord via the fifth lumbar and first sacral roots. Motor fibers exit through the corresponding anterior roots and form the efferent limb of segmental reflexes.
The spinal roots in the lumbar region, after exiting from the spinal cord, course downward in the subarachnoid space of the spinal canal and are gradually displaced laterally until they angulate and exit at the intervertebral foramina. Prior to entering the proximal foraminal canal, the spinal root lies in a shallow furrow along the inner surface of the pedicle, the lateral recess. The lumbar nerve roots traverse this lateral recess one level superior to their exit through the foramen. The lateral recess is a common site of entrapment of the traversing root by posterolaterally herniated disc material and bony overgrowth.
The parts of the back that possess the greatest freedom of movement, and hence are most frequently subject to injury, are the lumbar, lumbosacral, and cervical. In addition to bending, twisting, and other voluntary movements, many actions of the spine are reflexive in nature and are the basis of erect posture.
Degeneration in the intervertebral discs and ligaments is a consequence of aging and the succession of inevitable minor traumas to the spine. Deposition of collagen and elastin and alterations of glycosaminoglycans combine to decrease the water content of the nucleus pulposus; concomitantly, the cartilaginous endplate becomes less vascular (Hassler). The dehydrated disc thins out and becomes more fragile. Similar changes occur in the annulus of the disc, which frays to an increasing degree with the passage of time, permitting the nucleus pulposus to bulge and, sometimes with injury to the surrounding annulus, to extrude. This process can be observed by MRI, which shows a gradual reduction in the high T2 signal of the nucleus pulposus with the passage of time. In women who had MRI for gynecologic reasons, Powell and coworkers found an increasing frequency of lumbar disc degeneration and bulging, approaching 70 percent by the fiftieth year. Jensen and colleagues recorded similar abnormalities with aging in asymptomatic men and women (see further on).
The problem of degenerative spinal disease has been conceptualized as a series of events having its genesis in shrinkage of the disc that subsequently alters the alignment of the articular facets and vertebral bodies, leading to facet arthropathy and bony spur formation. These reactive changes contribute to stenosis of the spinal canal and directly compromise the lateral recesses of the canal and the intervertebral foramina, where they impinge on nerve roots. Osteoporosis, especially in older women, is a further important cause of vertebral flattening or collapse, additionally narrowing the spinal canal. All of these changes may further conspire to weaken ligaments and allow slippage of one vertebral body on adjacent ones, termed spondylolisthesis.
Of the several symptoms of spinal disease (pain, stiffness, limitation of movement, and deformity), pain is foremost. Four types of pain may be distinguished: local, referred, radicular, and that arising from secondary muscular spasm. These several types of pain can often be discerned from the patient’s description; reliance is placed mainly on the character of the pain, its location, and conditions that modify it.
Local pain is caused by any pathologic process that impinges on structures containing sensory endings, including the periosteum of the vertebral body, capsule of apophysial joints, annulus fibrosus, and ligaments. Destruction of the nucleus pulposus alone produces little or no pain but the annulus is innervated with small nerve fibers and, when subject to disruption, may produce considerable pain. This pain is steady and aching, but it may be intermittent and sharp, and, although not well circumscribed, is felt in or near the affected part of the spine. Pathologic change arising in spinal structures may also evoke discomfort in regions that share common innervation and thereby vaguely simulate the pain of radicular disease. These areas of projection may be considered similarly to the referred pain of the “sclerotomes” discussed in Chap. 8 and just below.
Referred pain in reference to the spine is of two types: one that is projected from the spine to viscera and other structures lying within the territory of the lumbar and upper sacral dermatomes, and another that is projected from pelvic and abdominal viscera to the spine. Pain caused by disease of the upper part of the lumbar spine may be referred to the medial flank, lateral hip, groin, and anterior thigh (sclerotomes; see Chap. 8). This has been attributed to irritation of the superior cluneal nerves, which are derived from the posterior divisions of the first three lumbar spinal nerves and innervate the superior portions of the buttocks. Pain from the lower part of the lumbar spine is usually referred to the lower buttocks and posterior thighs and is a result of irritation of lower spinal nerves, which activate the same pool of intraspinal neurons as the nerves that innervate the posterior thighs. Pain of this type is usually diffuse and has a deep, aching quality, but it tends at times to be more superficially projected. In general, the intensity of the referred pain parallels that of the local pain. Maneuvers that alter local pain have a similar effect on referred pain. McCall and colleagues and Kellgren have verified these areas of reference by the injection of hypertonic saline into the facet joints and the “sclerotomes” they determined are discussed in Chap. 8. But, as Sinclair and coworkers have pointed out, the sites of reference are inexact and cannot be relied on for precise anatomic localization.
In contrast to the movement-altered referred pain that originates in the spine, pain from visceral diseases felt within the abdomen, flanks, or lumbar region, is modified by the state of activity of the viscera and sometimes by assuming an upright or supine posture. In other words, its character and temporal relationships have little relationship to movement of the back.
Radicular or “root” pain has some of the characteristics of referred pain but differs in its greater intensity, distal radiation, circumscription to the territory of a root, and factors that excite it. The mechanism is stretching, irritation, or compression of a spinal root within or central to the intervertebral foramen. The pain is sharp, often intense, and usually superimposed on the dull ache of referred pain; it nearly always radiates from a paracentral position near the spine to some part of the lower limb. Coughing, sneezing, and straining characteristically evoke this sharp radiating pain, although each of these actions may also jar or move the spine and enhance local pain. Any maneuver that stretches the nerve root—e.g., “straight-leg raising” in cases of sciatica—evokes radicular pain. The specific patterns of radicular pain are described in the sections on prolapsed discs further on in the chapter, and the distribution of cutaneous innervation of the spinal roots is shown in Figs. 9-2 and 9-3. The most common pattern is sciatica, pain that originates in the buttock and is projected along the posterior or posterolateral thigh. It results from irritation of the L5 or S1 nerve root. Paresthesia or superficial sensory loss, soreness of the skin, and tenderness in certain regions along the nerve usually accompany radicular pain. If the anterior roots are involved as well, there is weakness, atrophy, or muscular twitching.
In patients with severe circumferential constriction of the cauda equina because of spondylosis (lumbar stenosis), sensorimotor impairment and referred pain are elicited by standing and walking. The symptoms are projected to the calves and the backs of the thighs thereby simulating the exercise-induced symptoms of iliofemoral arterial insufficiency—hence the term spinal claudication has been applied to the activity-induced symptoms of lumbar stenosis (see “Lumbar Stenosis and Spondylotic Caudal Radiculopathy” later in this chapter).
Referred pain from structures of the lower back (sometimes called pseudoradicular) does not, as a rule, project below the knees and is not accompanied by neurologic changes other than sometimes a vague numbness without demonstrable sensory impairment. This is quite in contrast to the pain of root compression. Pain resulting from muscular spasm usually occurs in relation to local spinal irritation and may be thought of as a nocifensive reflex for the protection of the diseased parts against injurious motion. Chronic muscular contraction may give rise to a dull, sometimes cramping local ache. One can sometimes feel the tautness of the sacrospinalis and gluteal muscles and demonstrate by palpation that the pain is localized to them. However, except for the most severe degrees of acute injuries of the back, the spasms are difficult to detect and their contribution to back pain has appeared to us to be relatively small.
In addition to assessing the character and location of the pain, one should determine the factors that aggravate and relieve it, its constancy, and its relationship to activity and to rest, posture, forward bending, coughing, sneezing, and straining. Frequently, the most important lead comes from knowledge of the mode of onset and the circumstances that initiated the pain. Inasmuch as many painful conditions of the back are the result of injuries incurred during work or in automobile accidents, the possibility of exaggeration or prolongation of pain for purposes of compensation must always be kept in mind.
The main goals of the examination of the back are to differentiate pain that is caused by nerve root compression from those of musculoskeletal strains, metastatic spinal tumor, and infectious and inflammatory diseases of the spine and hips.
Some information may be gained by inspection of the back, buttocks, and lower limbs in various positions. The normal spine shows a thoracic kyphosis and lumbar lordosis in the sagittal plane, which in some individuals may be exaggerated. In the coronal plane, the spine is normally straight or shows a slight curvature, particularly in women. One should observe the spine for excessive curvature, a list, flattening of the normal lumbar lordosis, presence of a gibbus (a sharp, kyphotic angulation usually indicative of a fracture), pelvic tilt or obliquity (Trendelenburg sign), and asymmetry of the paravertebral or gluteal musculature. A sagging gluteal fold suggests involvement of the S1 root. In sciatica one may observe a flexed posture of the affected leg, presumably to reduce tension on the irritated nerve root. Or, patients in whom a free fragment of lumbar disc material has migrated posterolaterally may be unable to lie down and extend the spine.
The next step in the examination is observation of the spine, hips, and legs during certain motions. No advantage accrues from determining how much pain the patient can tolerate. More important is to determine when and under what conditions the pain begins or worsens. Observation of the patient’s gait may disclose a subtle limp, a pelvic tilt, a shortening of step, or a stiffness of bearing—indicative of a disinclination to bear weight on a painful leg—the “antalgic gait”. Analysis of this type of gait is covered in greater detail in Chap. 7. One looks for limitation of motion while the patient is standing, sitting, and reclining. When standing, the motion of forward bending normally produces flattening and reversal of the lumbar lordotic curve and exaggeration of the thoracic curve. With lesions of the lumbosacral region that involve the posterior ligaments, articular facets, or sacrospinalis muscles and with ruptured lumbar discs, protective reflexes prevent flexion, which stretches these structures (“splinting”). As a consequence, the sacrospinalis muscles remain taut and prevent motion in the lumbar part of the spine. Forward bending then occurs at the hips and at the thoracolumbar junction; also, the patient bends in such a way as to avoid tensing the hamstring muscles and putting undue leverage on the pelvis. In the presence of degenerative disc disease, straightening up from a flexed position is performed only with difficulty.
Lateral bending is usually less revealing than forward bending but, in unilateral ligamentous or muscular strain, bending to the opposite side aggravates the pain by stretching the damaged tissues. With unilateral sciatica, the patient lists to one side and strongly resists bending to the opposite side, and the preferred posture in standing is with the leg slightly flexed at the hip and knee. When the herniated disc lies lateral to the nerve root and displaces it medially, tension on the root is reduced and pain is relieved by bending the trunk to the side opposite the lesion; with herniation medial to the root, tension is reduced by inclining the trunk to the side of the lesion.
In the sitting position, flexion of the hips can be performed more easily, even to the point of bringing the knees in contact with the chest. The reason for this is that knee flexion relaxes tightened hamstring muscles and relieves the stretch on the sciatic nerve. This feature may also be evident in instances of lumbar disc disease, making the maneuver less sensitive than others.
Examination with the patient in the reclining position yields much the same information as in the standing and sitting positions. With lumbosacral disc lesions and sciatica, passive lumbar flexion causes little pain and is not limited as long as the hamstrings are relaxed, and there is no stretching of the sciatic nerve. Thus, with the knees flexed to 90 degrees, sitting up from the reclining position is unimpeded and not painful; with knees extended, there is pain and limited motion (Kraus-Weber test). With vertebral disease, passive flexion of the hips is free, whereas flexion of the lumbar spine may be impeded and painful.
Among the most helpful signs in detecting nerve root compression is passive straight-leg raising (possible up to almost 90 degrees in normal individuals) with the patient supine. This places the sciatic nerve and its roots under tension, thereby producing radicular, radiating pain from the buttock through the posterior thigh. This maneuver is the usual way in which compression of the L5 or S1 nerve root is detected (Lasègue sign), however, it may also cause an anterior rotation of the pelvis around a transverse axis, increasing stress on the lumbosacral joint and causing milder radiating pain if this joint is arthritic or otherwise diseased. Straight raising of the opposite leg (“crossed straight-leg raising,” Fajersztajn sign) may cause sciatica on the opposite side and is a more specific sign of prolapsed disc than is the Lasègue sign. Several of the many derivatives of the straight-leg raising sign are discussed in the section on lumbar disc disease. Asking the seated patient to extend the leg so that the sole of the foot can be inspected is a way of checking for a feigned Lasègue sign.
A patient with lumbosacral strain or disc disease (except in the acute phase or if the disc fragment has migrated laterally) can usually extend the spine with little or no aggravation of pain. If there is an active inflammatory process or fracture of the vertebral body or posterior elements, hyperextension may be markedly limited. In disease of the upper lumbar roots, hyperextension of the leg with the patient prone is the motion that is most limited and reproduces pain; however, in some cases of lower lumbar disc disease with thickening of the ligamentum flavum, this movement is also painful.
Maneuvers in the lateral decubitus position yield less information but are useful in eliciting joint disease. In cases of sacroiliac joint disease, abduction of the upside leg against resistance reproduces pain in the sacroiliac region, sometimes with radiation of the pain to the buttock, posterior thigh, and symphysis pubis. Hyperextension of the upside leg with the downside leg flexed is another test for sacroiliac disease. Rotation and abduction of the leg evoke pain in a diseased hip joint and with trochanteric bursitis. A helpful indicator of hip disease is the Patrick test: with the patient supine, the heel of the offending leg is placed on the opposite knee, and pain is evoked by depressing the flexed leg and externally rotating the hip.
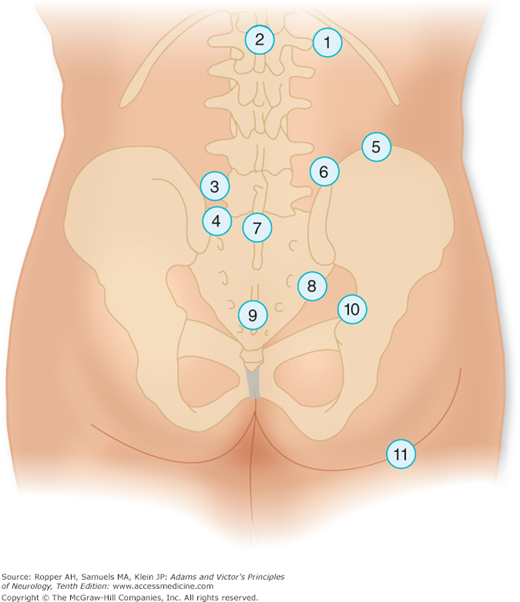
Gentle palpation and percussion of the spine are the last steps in the examination. It is preferable to first palpate the regions that are the least likely to evoke pain. The examiner should know what structures are being palpated (Fig. 11-2). Localized tenderness is seldom pronounced in disease of the spine because the involved structures are so deep. Nevertheless, tenderness over a spinous process or jarring by gentle percussion may indicate the presence of deeper, local spinal inflammation (as in disc space infection), pathologic fracture, metastasis, epidural abscess, or a disc lesion.
Figure 11-2.
(1) Costovertebral angle. (2) Spinous process and interspinous ligament. (3) Region of articular facet (fifth lumbar to first sacral). (4) Dorsum of sacrum. (5) Region of iliac crest. (6) Iliolumbar angle. (7) Spinous processes of fifth lumbar and first sacral vertebrae (tenderness = faulty posture or occasionally spina bifida occulta). (8) Region between posterior superior and posteroinferior spines. Sacroiliac ligaments (tenderness = sacroiliac sprain, often tender, with fifth lumbar or first sacral disc). (9) Sacrococcygeal junction (tenderness = sacrococcygeal injury; i.e., sprain or fracture). (10) Region of sacrosciatic notch (tenderness = fourth or fifth lumbar disc rupture and sacroiliac sprain). (11) Sciatic nerve trunk (tenderness = ruptured lumbar disc or sciatic nerve lesion).
Tenderness over the interspinous ligaments or over the region of the articular facets between the fifth lumbar and first sacral vertebrae is consistent with lumbosacral disc disease (Fig. 11-2, sites 2 and 3). Tenderness in this region and in the sacroiliac joints is also a frequent manifestation of ankylosing spondylitis. Arthritic changes at a facet may cause the same tenderness. Tenderness over the costovertebral angle often indicates genitourinary disease, adrenal disease, or an injury to the transverse process of the first or second lumbar vertebra (Fig. 11-2, site 1). Tenderness on palpation of the paraspinal muscles may signify a strain of muscle attachments or injury to the underlying transverse processes of the lumbar vertebrae. Focal pain in the same parasagittal line along the thoracic spine points to inflammation of the costotransverse articulation between spine and rib (costotransversitis). Other sites of tenderness and the structures implicated by disease are shown in the figure.
In palpating the spinous processes, it is important to note any deviation in the lateral plane (this may be indicative of fracture or arthritis) or in the anteroposterior plane. A “step-off” forward displacement of the spinous process and exaggerated lordosis are important clues to the presence of spondylolisthesis (see further on).
Many of the processes discussed above can coexist, especially in the older individual, who may have hip and lumbar spine osteoarthropathy. This makes the interpretation of various signs difficult unless the symptoms are first analyzed properly.
On completion of the examination of the back and legs, one turns to a search for motor, reflex, and sensory changes in the lower extremities (see “Herniation of Lumbar Intervertebral Discs,” further on in this chapter).
Depending on the circumstances, these may include a blood count, erythrocyte sedimentation rate, and C-reactive protein (especially helpful in screening for spinal osteomyelitis, epidural abscess, or myeloma). Other useful blood tests are calcium, alkaline phosphatase, and prostate-specific antigen (if one suspects metastatic carcinoma of the prostate); a serum protein immunoelectrophoresis (myeloma proteins); in special cases, a tuberculin test or serologic test for Brucella; a test for rheumatoid factor; and human leukocyte antigen (HLA) typing (for ankylosing spondylitis), all in the appropriate settings.
Radiographs of the lumbar spine may be useful in the routine evaluation of low back pain and sciatica and can be performed with the patient in flexed and extended positions in the anteroposterior, lateral, and oblique planes. Readily demonstrable in plain films are narrowing of the intervertebral disc spaces, bony facetal or vertebral overgrowth, displacement of vertebral bodies (spondylolisthesis), and an unsuspected infiltration of bone by cancer. However, in cases of suspected disc herniation or tumor infiltration of the spinal canal, one generally proceeds directly to MRI. Administration of gadolinium at the time of MRI enhances regions of inflammation and tumor but is not particularly helpful in cases of degenerative and disc disease of the spine. T2-weighted MRI performed with elimination of the hyperintense signal of fat (“fat suppression”, i.e., the short T1 inversion recovery or “STIR” sequence), allows inflammation and edema to be visualized in the bone marrow and paravertebral soft tissues that normally contain fat. The current generation of MRI scanners has largely replaced conventional myelography for the examination of spinal disease but the latter, when combined with CT, provides detailed information about the dural sleeves that surround the spinal roots as occur with arachnoiditis, disclosing subtle truncations caused by laterally situated disc herniations and at times revealing surface abnormalities of the spinal cord, such as arteriovenous malformations. When metallic devices such as a pacemaker preclude the performance of MRI, CT myelography remains very useful for diagnosis.
Nerve conduction studies and electromyography (EMG) are particularly helpful in suspected root and nerve diseases as indicated further on in the discussion of spinal nerve root disease. However, as for all the aforementioned tests, they must be interpreted in the context of the history and clinical examination; otherwise they are subject to over interpretation.
Anatomic variations of the spine are frequent and, though rarely themselves the source of pain and functional derangement, they may predispose an individual to discogenic and spondylotic complications by virtue of altering the mechanics and alignment of the vertebrae or size of the spinal canal.
A common anomaly is fusion of the fifth lumbar vertebral body to the sacrum (“sacralization”) or, conversely, separation of the first sacral segment, giving rise to 6, rather than the usual 5 lumbar vertebrae (“lumbarization”). However, neither of these is consistently associated with any type of back derangement. Another less-common finding is a lack of fusion of the laminae of one or several of the lumbar vertebrae or of the sacrum (spina bifida). Occasionally, a subcutaneous mass, hypertrichosis, or hyperpigmentation in the lumbar or sacral area overlying the bony separation betrays the condition, but in most patients it remains occult until it is disclosed radiologically. The anomaly may be accompanied by malformation of vertebral joints and usually induces pain only when aggravated by injury. The neurologic aspects of defective fusion of the spine (dysraphism) are discussed in Chap. 38, with developmental abnormalities of the nervous system.
Many other congenital variants affect the lower lumbar vertebrae: asymmetrical facet joints, abnormalities of the transverse processes, are seen occasionally in patients with low back symptoms, but apparently with no greater frequency than in asymptomatic individuals. Spondylolysis consists of a congenital and probably genetic bony defect in the pars interarticularis (the segment at the junction of pedicle and lamina) of the lower lumbar vertebrae. It is remarkably common, affecting approximately 5 percent of the North American population and mainly a disease of children (peak incidence between 5 and 7 years of age). The defect assumes importance in that it predisposes to subtle fracture of the pars articularis, sometimes precipitated by slight trauma but often in the absence of an appreciated injury. In some young individuals, it is unilateral and may cause unilateral lumbar aching back pain that is accentuated by hyperextension and twisting. In the usual bilateral form, small fractures at the pars interarticularis allow the vertebral body, pedicles, and superior articular facets to move anteriorly, leaving the posterior elements behind. This leads to an anterior displacement of one vertebral body in relation to the adjacent one, spondylolisthesis. Considerable dull, aching back pain can result.
The main cause of spondylolisthesis in older adults is degenerative arthritic disease of the spine as discussed further on. Patients with progressive vertebral displacement and neurologic deficits require surgery. Reduction of displaced vertebral bodies before fusion and direct repair of pars defects are possible in special cases. Back pain is relieved in the majority of cases.
These constitute by far the most frequent causes of low back pain. In severe acute injuries from direct impact the examiner must be careful to avoid further damage and movements should be kept to a minimum until an approximate diagnosis has been made. If the patient complains of pain in the back and cannot move the legs, the spine may have been fractured and the cord or cauda equina compressed or crushed. (See Chap. 44 for further discussion of spinal cord injury.) Lesser degrees of injury, such as sprains and strains, are ubiquitous and can be handled with less caution because they do not involve compression of neural structures or displacement of spinal elements.
The terms lumbosacral strain, sprain, and derangement are used loosely, and it is probably not possible to differentiate them. Furthermore, what was formerly referred to as “sacroiliac strain” or “sprain” is now known to be caused by, in some instances, disc disease. The term acute low back strain may be preferable for minor, self-limiting injuries that are usually associated with lifting heavy loads when the back is in a mechanically disadvantaged position, or there may have been a fall, prolonged uncomfortable postures such as in air travel or car rides, or sudden unexpected motion, as may occur in an auto accident.
Nonetheless, the discomfort of acute low back strain can be severe, and the patient may assume unusual postures related to spasm of the lower lumbar and sacrospinalis muscles. The pain is usually confined to the lower part of the back, in the midline, across the posterior waist, or just to one side of the spine. The diagnosis of lumbosacral strain is dependent on the biomechanics of the injury or activity that precipitated the pain. The injured structures are identified by the localization of the pain, the finding of localized tenderness, augmentation of pain by postural changes—e.g., bending forward, twisting, or standing up from a sitting position, and by the absence of signs of radicular involvement. In more than 80 percent of cases of acute low back strain of this type, the pain resolves in a matter of several days or a week, even with no specific treatment.
Sacroiliac joint and ligamentous strain is the most likely diagnosis when there is tenderness over the sacroiliac joint and pain radiating to the buttock and posterior thigh, but this always needs to be distinguished from the sciatica of a herniated intervertebral disc (see further on). Strain is characteristically worsened by abduction of the thigh against resistance and may produce pain that is also felt in the symphysis pubis or groin.
The pain of muscular and ligamentous strains is usually self-limiting, responding to simple measures in a relatively short period of time. The basic principle of therapy in both disorders is to avoid reinjury and reduce the discomfort of painful parts. As a result of several studies that have failed to demonstrate a benefit of bed rest, the recent practice has been to mobilize patients as soon as they are able and to prescribe exercises designed to stretch and strengthen trunk (especially abdominal) muscles, overcome faulty posture, and increase the mobility of the spinal joints. Despite this approach, the authors can affirm from personal experience that some injuries produce such discomfort that arising from a bed or chair is simply not possible in the early days after injury (see Vroomen et al). Lying on the side with knees and hips flexed, or supine with a pillow under the knees favor relief of pain. With strains of the sacrospinalis muscles and sacroiliac ligaments, the optimal position is hyperextension, which is effected by having the patient lie with a small pillow under the lumbar portion of the spine or by lying prone. Local physical measures—such as application of ice in the acute phase and, later, heat diathermy and massage—often relieve pain temporarily. Nonsteroidal antiinflammatory drugs (NSAIDs) may be given liberally during the first few days. Muscle relaxants (e.g., cyclobenzaprine, carisoprodol, metaxalone, and the diazepams) serve mainly to make bed rest more tolerable but have little primary effect. Traction, formerly a popular treatment, is infrequently used. When weight bearing is resumed, discomfort may be diminished by a light lumbosacral support, but many orthopedists refrain from prescribing this aid.
Spinal manipulation—practiced by chiropractors, osteopaths, and others—has always been a contentious matter partly because of unrealistic therapeutic claims made in treating diseases other than low back derangements. A type of slow muscle stretching and joint distraction (axial traction on a joint) administered by physiatrists and physical therapists is quite similar. It must be recognized that many patients seek chiropractic manipulation for back complaints, often before seeing a physician, and may not disclose this information. When the supporting elements of the spine (pedicles, facets, and ligaments) are not disrupted, chiropractic manipulation of the lumbar spine has provided acute relief to a number of our patients with low back strain or facet pain. At issue is the durability of the effect, particularly the need for repeated spinal adjustments. One randomized British trial has shown manipulation to be faster than analgesics and bed rest in returning patients to work after minor back injury (Meade et al). Some trials have corroborated this finding (Hadler et al), whereas others have not, or, often, the results have been ambiguous. In the study by Cherkin and colleagues comparing chiropractic, physical therapy (McKenzie method), and simple instruction to the patient from a booklet, manipulation yielded a slightly better outcome at the end of a month. Despite several hypotheses offered by practitioners of spinal manipulation, the mechanism of pain relief is not known. The cracking sound created by rapid distraction of the facet joints (and attributed to gas coming out of solution in the joint fluid) seems not to be necessary for pain relief. It is unlikely that mundane low back pain represents minor subluxation, as claimed by chiropractors. In the authors’ clinical experience, chronic low back pain, discussed below, has been less successfully treated by manipulative procedures than has acute pain, but there are some patients who testify to improvement in their clinical state and admittedly, the medical profession has little to offer in most cases of chronic low back pain. The results for acute and chronic back pain with another popular approach, acupuncture, have been even more uncertain, most studies showing it to be no more effective than a sham treatment (Tudler et al). It should be emphasized, however, that the chronic use of NSAIDs or narcotic analgesics is hazardous and is not an appealing alternative.
Often the symptoms of low back strain are recurrent and more chronic in nature, being regularly exacerbated by bending or lifting, suggesting that postural, muscular, and arthritic factors play a role. This is the most common syndrome seen in spine clinics, more often in men than in women.
Insidiously, or after some unusual activity, raising the question of trauma, especially if it happens in the work-place, the patient develops aching pain in the low back, increased by certain movements and attended by stiffness. The pain may additionally have a restricted radiation into the buttocks and posterior thigh, thereby simulating root compression. There are no motor, sensory, or reflex abnormalities. Radiographs and imaging procedures usually reveal some combination of osteoarthropathy, changes in vertebral discs, osteoarthritic changes in apophysial joints, and sometimes osteoporosis or slight spondylosis, or they may be entirely normal. Treatment with short-duration bed rest, analgesics, and physiotherapy, as outlined for acute strains, helps to relieve the symptoms, and the majority of patients recover within a few weeks, only to have a recurrence of similar pains in the future. Recurrent attacks are typical of degenerative spine disease that affects the vertebrae and facet joints. Usually, the origin of the pain cannot be assigned with certainty to spinal, joint, or muscular injury, but direct percussion tenderness of one vertebral segment always raises concern of metastatic disease as noted above. Quite often, changing the firmness of the mattress (in either direction) is helpful. Compensation relating to injuries at work or to an accident and related legal matters often add to the disability, but there are, of course, many legitimate injuries that occur in these circumstances.
Fractures of lumbar vertebral bodies are usually the result of flexion injuries. Such trauma may occur in a fall or jump from a height (if the patient lands on his feet, the calcanei may also be fractured) or as a result of an auto accident or other violent injury. If the injury is severe, it may cause a fracture dislocation, a “burst” fracture of one or more vertebral bodies, or an asymmetrical fracture of a pedicle, lamina, or spinous process; most often, however, there is asymmetrical loss of height of a vertebral body (wedge compression fracture), which may be extremely painful at the onset. When compression or other fractures occur with minimal trauma (or spontaneously), the bone has presumably been weakened by some pathologic process. Most of the time, particularly in older individuals, osteoporosis is the cause of such an event, but there are many other causes, including osteomalacia, hyperparathyroidism, prolonged use of corticosteroids, myeloma, metastatic carcinoma, and a number of other conditions that are destructive of bone. Spasm of the lower lumbar muscles, limitation of all movements of the lumbar section of the spine, and the radiographic appearance of the damaged lumbar portion (with or without neurologic abnormalities) are the basis of clinical diagnosis. The pain is usually immediate, although occasionally it may be delayed for days.
A fractured transverse process, which is almost always associated with high-impact rotary injury of the spine and causes tearing of the paravertebral muscles and a local hematoma, produces deep tenderness at the site of the injury and limitation of all movements that stretch the lumbar muscles. The imaging findings, particularly MRI, confirm the diagnosis. In some circumstances, tears of the paravertebral musculature may be associated with extensive bleeding into the retroperitoneal space; this produces paraspinal or groin pain and proximal leg weakness with loss of the patellar reflex on the affected side. There may be a delayed subcutaneous hematoma in the flanks (Grey-Turner sign).
A problem not easily classified but having a distinctive clinical profile that should be known to neurologists is that of an osteoid osteoma. These benign tumors characteristically cause severe nocturnal pain located in one region of the parasagittal spine that awakens the patient from a peaceful sleep; also typical is complete relief after aspirin or small doses of other NSAIDs. MRI or CT is required to detect the lesion, as it may not be evident on plain radiographs of the spine. The typical appearance is a well-demarcated lytic lesion surrounded by a rim of bony sclerosis.
For the mundane thoracic and lumbar fracture associated with osteoporosis, bed rest, and analgesics are usually adequate. In the past two decades several mechanical approaches to reducing pain have been investigated. The injection of various materials directly into the fracture site within the vertebral body (vertebroplasty) attained popularity because of reports of marked pain relief. Several large trials have addressed the use of vertebroplasty and given conflicting results. The best conducted of these, with a placebo control groups (see Buchbinder et al and Kallmes et al) concluded that there was no durable benefit, however, these two studies included patients with fractures up to a year old. Having witnessed a few patients with almost immediate and remarkable relief of severe pain, we are uncertain of the best course but acknowledge that this is probably not an effective treatment for the majority of patients. Further discussion can be found in the review by Ensrud and Schousboe.
This condition is a major cause of severe and chronic or recurrent low back and leg pain. It occurs mainly during the third and fourth decades of life when the nucleus pulposus is still gelatinous. The disc between the fifth lumbar or first sacral vertebrae (L5-S1) is most often involved, and, with decreasing frequency, that between the fourth and fifth (L4-L5), third and fourth (L3-L4), second and third (L2-L3), and—quite infrequently—the first and second (L1-L2) lumbar vertebrae. Relatively rare but well described in the thoracic portion of the spine, disc disease is again frequent in the cervical spine at the fifth and sixth and the sixth and seventh cervical vertebrae (see further on).
INTERVERTEBRAL DISC SPACE | ROOT AFFECTED | PAIN REFERRAL | WEAKNESS | REFLEX CHANGE | ADDITIONAL FEATURES |
|---|---|---|---|---|---|
C4-C5 | C5 | Shoulder, trapezius | Supra- and infraspinatus deltoid, slight biceps weakness | Slightly diminished biceps jerk | |
C5-C6 | C6 | Trapezius ridge and tip of shoulder, radiation to anterior upper arm, thumb, and index finger | Biceps, brachioradialis, extensor carpi radialis | Diminished biceps and supinator jerk | Tenderness over spine or scapula and suprascapular region; paresthesias in thumb and index finger |
C6-C7 | C7 | Shoulder, axilla, posterolateral arm, elbow, and middle finger | Triceps, wrist extensors | Diminished or absent triceps jerk | Tenderness over medial scapula and supraclavicular region or triceps. May complain of paresthesias in most of the fingers |
C7-T1 | C8 | Medial forearm | Intrinsic hand muscles | Slight or no decrease in triceps jerk | Mimics ulnar palsy |
L2-L3 | L3 | Anterior thigh, over knee | Thigh adductor, quadriceps | Absent or diminished knee jerk | |
L3-L4 | L4 | Anterolateral thigh, medial foreleg | Anterior tibial, sometimes with partial foot drop | Diminished or normal knee jerk | |
L4-L5 | L5 | Posterolateral gluteal sciatica; lateral thigh, anterolateral foreleg, dorsal foot, lateral malleolus and great or second and third toe | Extensor hallucis longus and extensor digitorum brevis; some weakness of anterior tibialis, sometimes with foot drop | Unaffected (except posterior tibial) | Pain with straight-leg raising and variant tests; tenderness over fourth lumbar lateral process and lateral gluteal region |
L5-S1 | S1 | Midgluteal sciatica; posterior thigh, posterolateral leg, lateral foot, heel, or lateral toes | Plantar-flexor and hamstring weakness | Absent or diminished ankle jerk | Pain with straight-leg raising and variant tests; tenderness over lumbosacral (L5-S1) joint and sciatic notch; discomfort walking on heels |
The cause of a herniated lumbar disc in any individual case is often not identifiable and flexion injury is often imputed, but a considerable proportion of patients do not recall an inciting episode. Degeneration of the annulus and the posterior longitudinal ligaments, and changes nuclei pulposis itself may have taken place silently or have been manifest by mild, recurrent lumbar ache. A sneeze, lurch, or other trivial movement may then cause the nucleus pulposus to prolapse, pushing the frayed and weakened annulus posteriorly. Fragments of the nucleus pulposus protrude through rents in the annulus, usually to one side or the other (sometimes in the midline), where they impinge on one or more nerve roots and cause the characteristic sciatic or other radicular pains and neurologic signs. In more severe cases of disc disease, a small piece of the nucleus may be entirely extruded as a “free fragment”, sometimes called a sequestered disc fragment, and be mobile enough to affect a root at an adjacent level or to give rise to unusual precipitating features of radicular pain. Large protrusions cause pain by compressing the adjacent root against the articular apophysis or lamina. The protruded material may become reduced in size over time, presumably from desiccation, but often there is continued chronic irritation of the root or a discarthrosis with posterior osteophyte formation.
The fully developed syndrome of the common prolapsed intervertebral lower lumbar disc consists of (1) pain in the sacroiliac region, radiating into the buttock, thigh, and the calf, a symptom broadly termed sciatica; (2) a stiff or unnatural spinal posture; and often (3) some combination of paresthesia, weakness, and reflex impairment.
The pain of herniated intervertebral disc varies in severity from a mild aching discomfort to severe knife-like stabs that radiate the length of the leg and are superimposed on a constant intense ache. Sciatic pain is usually perceived by the patient as originating deep in the buttock and radiating to the posterolateral thigh; it may progress to the calf and ankle—to the medial malleolus (L4), lateral malleolus (L5), or heel (S1); however, distal radiation to the foot is less frequent. There are variations in the sciatic syndrome. Abortive forms may produce aching discomfort only in the lower buttock or proximal thigh and occasionally only in the lower hamstring or upper calf. With the most severe pain, the patient is forced to stay in bed, avoiding the slightest movement; a cough, sneeze, or strain is intolerable. The most comfortable position may be lying on the back with legs flexed at the knees and hips and the shoulders raised on pillows to obliterate the lumbar lordosis. For some patients, a lateral decubitus position is more comfortable. Free fragments of disc that find their way to a lateral and posterior position in the spinal canal may produce the opposite situation, one whereby the patient is unable to extend the spine and lie supine. Sitting and standing up from a sitting position may be particularly painful. It is surprising to patients that a lumbar disc protrusion may cause little or no back pain. If there is back discomfort, it tends to be just paraspinal on the side of sciatica and mainly in the acute stages.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree