Tremor, Myoclonus, Focal Dystonias, and Tics: Introduction
The subject of tremor is considered at this point because of its association with diseases of the basal ganglia and cerebellum. In addition, a group of miscellaneous movement disorders—myoclonus, facial and cervical dyskinesias, focal limb dystonias, and tics—is described in this chapter. These disorders are largely involuntary in nature and can be quite disabling but they have an uncertain pathologic basis, as alluded to in Chap. 4, and an indefinite relationship to the extrapyramidal motor disorders or to other standard categories of neurologic disease. They are brought together here mainly for convenience of exposition.
Tremor
Tremor may be defined as involuntary rhythmic oscillatory movement produced by alternating or irregularly synchronous contractions of reciprocally innervated muscles. Its rhythmic quality distinguishes tremor from other involuntary movements, and its oscillatory nature distinguishes it from myoclonus and asterixis.
A normal, or physiologic, tremor is embedded in the motor system. It is present in all contracting muscle groups and persists throughout the waking state and even in certain phases of sleep. The movement is so fine that it can barely be seen by the naked eye, and then only if the fingers are firmly outstretched; in most instances special instruments are required for its detection though asking the patient to aim a laser pointer at a distant target will often expose it. It ranges in frequency between 8 and 13 Hz, the dominant rate being 10 Hz in adulthood and somewhat less in childhood and old age. Several hypotheses have been proposed to explain physiologic tremor, a traditional one being that it reflects the passive vibration of body tissues produced by mechanical activity of cardiac origin, but this cannot be the whole explanation. As Marsden has pointed out, several additional factors—such as spindle input, the unfused grouped firing rates of motor neurons, and the natural resonating frequencies and inertia of the muscles and other structures—are probably of greater importance. Certain abnormal tremors, namely, the metabolic varieties of postural or action tremor and at least one type of familial tremor, are considered by some to be variants or exaggerations of physiologic tremor—i.e., “enhanced physiologic tremor,” as discussed further on.
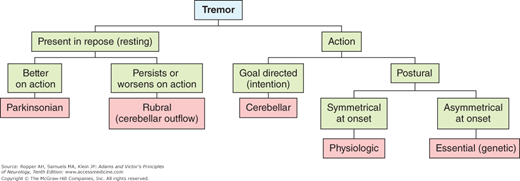
The following types of tremors, the clinical features of which are summarized in Fig. 6-1 and Table 6-1, are encountered most frequently in clinical practice. In clinical analysis they are usually distinguishable on the basis of (1) relation to movement and posture, (2) frequency, (3) the pattern of activity of opposing (agonist-antagonist pairs) muscles, i.e., synchronous or alternating, and (4) affected body parts. Such a classification also differentiates tremors from a large array of nontremorous movements, such as fasciculations, sensory ataxia, myoclonus, asterixis, epilepsia partialis continua, clonus, and rigor (shivering).
TYPE OF TREMOR | FREQUENCY, HZ | PREDOMINANT LOCATION | ENHANCING AGENTS | ATTENUATING AGENTS |
|---|---|---|---|---|
Physiologic (enhanced) | 8–13 | Hands | Epinephrine, β-adrenergics | Alcohol, β-adrenergic antagonists |
Parkinson (rest) | 3–5 | Hands and forearms, fingers, feet, lips, tongue | Emotional stress | L-Dopa, anticholinergics |
Cerebellar (intention, ataxic, “rubral”) | 2–4 | Limbs, trunk, head | Emotional stress | — |
Postural, or action | 5–8 | Hands | Anxiety, fright, β-adrenergics, alcohol withdrawal, xanthines, lithium, exercise, fatigue | β-Adrenergic antagonists in some cases |
Essential (familial, senile) | 4–8 | Hands, head, vocal cords | Same as above | Alcohol, propanolol, primidone |
Alternate beat | 3.5–6 | Hands, head | Same as above | Clonazepam, alcohol, β-adrenergic antagonists |
Orthostatic | 4–8, irregular | Legs | Quiet standing | Repose, walking, clonazepam, valproate |
Tremor of neuropathy | 4–7 | Hands | — | — |
Palatal tremor | 60–100/min | Palate, sometimes facial, pharyngeal, proximal limb muscles | — | Clonazepam, valproate |
Dystonic | Irregular | Concordant with focal dystonia | — | Local botulinum toxin, gestes |
Action tremors are evident during use of the affected body part, as opposed to tremor that is apparent in a position of rest or repose. Action tremors can be conveniently divided into two categories: goal directed action tremor of the ataxic type related to cerebellar disorders (discussed in Chap. 5) and postural tremors, which are either the enhanced physiologic variety or essential tremor (Fig. 6-1). A postural tremor occurs with the limbs and trunk actively maintained in certain positions (such as holding the arms outstretched) and may persist throughout active movement. More particularly, the tremor is absent when the limbs are relaxed but becomes evident when the muscles are activated. The tremor is accentuated as greater precision of movement is demanded, but it does not approach the degree of augmentation seen with cerebellar intention tremor. Most cases of action tremor are characterized by relatively rhythmic bursts of grouped motor neuron discharges that occur not quite synchronously in opposing muscle groups as shown in Fig. 6-2. Slight inequalities in the strength and timing of contraction of opposing muscle groups account for the tremor. In contrast, rest (parkinsonian) tremor, is characterized by alternating activity in agonist and antagonist muscles.
Figure 6-2.
Types of tremor. In each, the lowest trace is an accelerometric recording from the outstretched hand; the upper two traces are surface EMG from the wrist extensor (upper) and flexor (middle) muscle groups. A. A physiologic tremor; there is no evidence of synchronization of EMG activity. B. Essential (familial) tremor; the movements are very regular and EMG bursts occur simultaneously in antagonistic muscle groups. C. Neuropathic tremor; movements are irregular and EMG bursts vary in timing between the two groups. D. Parkinsonian (“rest”) tremor; EMG bursts alternate between antagonistic muscle groups. Calibration is 1 s. (Courtesy of Dr. Robert R. Young.)
The type of action tremor that seems merely to be an exaggeration of the above-described physiologic tremor, can be brought out in most normal persons. It has the same fast frequency as physiologic tremor (about 10 Hz; Fig. 6-2) but with greater amplitude. Such a tremor, best elicited by holding the arms outstretched with fingers spread apart, is characteristic of intense fright and anxiety (hyperadrenergic states), certain metabolic disturbances (hyperthyroidism, hypercortisolism, hypoglycemia), pheochromocytoma, intense physical exertion, withdrawal from alcohol and other sedative drugs, and the toxic effects of several drugs—lithium, nicotinic acid, xanthines (coffee, tea, aminophylline), cocaine, methylphenidate, other stimulant drugs and corticosteroids. Young and colleagues have determined that the enhancement of physiologic tremor that occurs in metabolic and toxic states is not a function of the central nervous system but is instead a consequence of stimulation of muscular beta-adrenergic receptors by increased levels of circulating catecholamines.
A special type of postural action tremor, closely related to the enhanced physiologic tremor, occurs as the most prominent feature of the early stages of alcohol withdrawal. Withdrawal of other sedative drugs (benzodiazepines, barbiturates) following a sustained period of use produces much the same effect. LeFebvre-D’Amour and colleagues have described two tremors of slightly different frequency, one of which is indistinguishable from essential tremor (see below). Either of these may occur as the individual emerges from a relatively short period of intoxication (“morning shakes”). A number of alcoholics, on recovery from the withdrawal state, exhibit a persistent tremor of essential (familial) type, described below. The mechanisms involved in alcohol withdrawal symptoms are discussed further in Chap. 42.
This, the commonest type of tremor, is of lower frequency (4 to 8 Hz) than physiologic tremor and is unassociated with other neurologic changes; thus it is called “essential.” It is usually at the lower end of this frequency range and of variable amplitude. Aside from its rate the identifying feature is its appearance or marked enhancement with attempts to maintain a static limb posture. Like most tremors, essential tremor is worsened by emotion, exercise, and fatigue. One infrequent type of essential tremor is faster than the usual essential tremor and of the same frequency (6 to 8 Hz) as enhanced physiologic tremor. Essential tremor may increase in severity to a point where the patient’s handwriting becomes illegible and he cannot bring a spoon or glass to his lips without spilling its contents. Eventually, all tasks that require manual dexterity become difficult or impossible. The pathophysiology of this tremor and its treatment are discussed further on.
Typical essential tremor very often occurs in several members of a family, for which reason it has been called familial or hereditary essential tremor. Inheritance is in an autosomal dominant pattern with high penetrance. The idiopathic and familial types cannot be distinguished on the basis of their physiologic and pharmacologic properties and probably should not be considered as separate entities. This condition has been referred to as “benign essential tremor,” but this is hardly so in many patients in whom it worsens with age and greatly interferes with normal activities.
Essential tremor most often makes its appearance late in the second decade, but it may begin in childhood and then persist. A second peak of increased incidence occurs in adults older than 35 years of age. Both sexes are affected. It is a relatively common disorder, with an estimated prevalence of 415 per 100,000 persons older than the age of 40 years (Haerer et al). As described by Elble, the tremor frequency diminishes slightly with age while its amplitude increases.
The tremor practically always begins in the arms and is usually almost symmetrical; in approximately 15 percent of patients, however, it may appear first in the dominant hand. A severe isolated arm or leg tremor should suggest another disease (Parkinson disease or focal dystonia, as described further on).
The tremor may remain limited to the upper limbs or a side-to-side or nodding movement of the head; tremor of the chin may be added or may occur independently. In certain cases of essential tremor, there is involvement of the jaw, lips, tongue, and larynx, the latter imparting a severe quaver to the voice (voice tremor). Infrequently, the tremor of the head or voice precedes that of the hands. The head tremor is also postural in nature and disappears when the head is supported. It has also been noted that the limb and head tremors tend to be muted when the patient walks. In some of our patients whose tremor remained isolated to the head for a decade or more, there has been little if any progression to the arms and almost no increase of the amplitude of movement.
The lower limbs are usually spared or only minimally affected. In the large series of familial tremor cases by Bain and colleagues, solitary jaw or head tremor was not found but we have observed isolated head tremor, as noted. Most patients with essential tremor will have identified the amplifying effects of anxiety and the ameliorating effects of alcohol on their tremor. We have also observed the tremor to become greatly exaggerated during emergence from anesthesia in a few patients.
Electromyographic studies reveal that the tremor is generated by more or less rhythmic and almost simultaneous bursts of activity in pairs of agonist and antagonist muscles (Fig. 6-2B). Less often, especially in the tremors at the lower range of frequency, the activity in agonist and antagonist muscles alternates (“alternate beat tremor”), a feature more characteristic of Parkinson disease, which the tremor then superficially resembles (see below). Tremor of either pattern may be disabling, but the less common, slower, alternate-beat tremor tends to be of higher amplitude, is more of a handicap, and is usually more resistant to treatment.
A curious fact about essential tremor of the typical (non–alternate-beat) type is that it can be suppressed by a small amount of alcohol in more than 75 percent of patients; but once the effects of the alcohol have worn off, the tremor returns and may even worsen for a time. Of more therapeutic interest, essential tremor is inhibited by the beta-adrenergic antagonist propranolol (between 80 and 200 mg per day in divided doses or as a sustained-release preparation) taken orally over a long period of time. Often it takes several days or weeks for the effect to be evident. The benefit is variable and often incomplete; most studies indicate that 50 to 70 percent of patients have some symptomatic relief but may complain of side effects such as fatigue, erectile dysfunction, and bronchospasm.
The mechanism and site of action of beta-blocking agents is not known with certainty. It is blockade of the beta-2 adrenergic receptor that most closely aligned with reduction of the tremor. Several but not all of the other beta-blocking drugs are similarly effective to propranolol; metoprolol and nadolol, which are better tolerated than propranolol, are the ones most extensively studied, but they have yielded less consistent results than propranolol. The relative merits of different drugs in this class are discussed by Louis and by Koller et al (2000). Young and associates have shown that neither propranolol nor ethanol, when injected intraarterially into a limb, decreases the amplitude of essential tremor. These findings, and the delay in action of medications, suggest that their therapeutic effect is due less to blockade of the peripheral beta-adrenergic receptors than to their action on structures within the central nervous system. This is in contrast to the earlier mentioned muscle receptor-mediated effect of adrenergic compounds in physiologic tremor. It is possible that this ambiguity regarding the action of beta-blocking drugs is the result of their effect on physiological tremor that is superimposed on essential tremor.
The barbiturate drug primidone has also been effective in controlling essential tremor and may be tried in patients who do not respond to or cannot tolerate beta-blocking medications, but many patients cannot tolerate the side effects of drowsiness, nausea, and slight ataxia. Treatment should be initiated at 25 mg per day and increased slowly to 75 mg per day in order to minimize these effects. Gabapentin, topiramate (see Connor), mirtazipine, a variety of benzodiazepines and a large number of other drugs have been used with variable success, but at the moment should probably be considered second-line therapies; these alternatives are discussed by Louis. Amantadine also has a modest effect on tremor and may be used as an adjunct.
The alternate-beat, slow, high-amplitude, kinetic-predominant type of essential tremor is more difficult to suppress but has reportedly responded to clonazepam (Biary and Koller); in our experience, however, this approach has not been as successful. Alcohol and primidone have also had less effect than they do in typical essential tremor. Indeed, the tremor has often been resistant to most attempts at suppression, for which reason surgical approaches are now being used (see further on).
Injections of botulinum toxin into a portion of a limb can reduce the severity of essential tremor locally, but the accompanying weakness of arm and hand muscles often proves unacceptable to the patient. The same medication injected into the vocal cords can suppress severe voice tremor as described in a series of cases by Adler and colleagues as well as by others, but caution must be exercised to avoid paralyzing the cords. Doses as low as 1 U of toxin injected into each cord may be effective, with a latency of several days. The long-term repeated use of this treatment has not been adequately studied for essential-type limb or voice tremor.
In resistant cases of essential tremor of the fast or slow variety, stimulation by electrodes implanted in the ventral medial nucleus thalamus or the internal segment of the globus pallidus (of the same type used to treat Parkinson disease) has produced a durable response over many years; details can be found in the small study reported by Sydow and colleagues.
Adams and coworkers described a disabling action tremor in patients with chronic demyelinating and paraproteinemic polyneuropathies. It is a particularly prominent feature of the polyneuropathy caused by immunoglobulin M (IgM) antibodies to myelin-associated glycoprotein (MAG) as mentioned in the preceding chapter. The movements simulate a coarse essential, or ataxic, tremor and typically worsen if the patient is asked to hold his finger near a target. The EMG pattern is more irregular than that in essential (familial) tremor (Fig. 6-2C). Pedersen and colleagues have found it to vary greatly in amplitude with considerable side-to-side oscillation, which is induced by co-contracting muscle activity; they also found little suppression of the tremor with loading of the limb, unlike most other organic tremors. It is hypothesized that there is a disturbance of muscle spindle afferents.
Some cases of acute or chronic inflammatory neuropathy or ganglionopathy may be marked by a similar and prominent ataxic tremor and a faster action tremor. A special type of Guillain-Barré syndrome (Fisher variant) is characterized by a tremor that is indistinguishable from ataxia. Also, the inherited disease, peroneal muscular atrophy (Charcot-Marie-Tooth disease), may be associated with tremor of the essential type but the two may be coincident rather than directly related; this combination of symptoms was the basis on which Roussy and Levy incorrectly set it apart as a distinct disease. Chapter 46 discusses these polyneuropathies.
True action tremors are seen in a number of other clinical settings. A coarse action tremor, sometimes combined with myoclonus, accompanies various types of meningoencephalitis (e.g., in the past it was quite common with syphilitic general paresis) and certain intoxications (methyl bromide and bismuth).
This is a coarse, rhythmic tremor with a frequency of 3 to 5 Hz. Electromyographically, it is characterized by bursts of activity that alternate between opposing muscle groups. The tremor is most often localized in one or both hands and forearms and less frequently in the feet, jaw, lips, or tongue (Fig. 6-2D). It occurs when the limb is in an attitude of repose and is suppressed or diminished by willed movement, at least momentarily, only to reassert itself once the limb assumes a new position. Even though it is termed a “resting” tremor, maintaining the arm in an attitude of repose requires a certain degree of muscular contraction, albeit slight. If the tremulous hand is completely relaxed, as it is when the arm is fully supported at the wrist and elbow, the tremor usually disappears; however, the patient rarely achieves this state. Usually he maintains a state of slight tonic contraction of the trunk and proximal muscles of the limbs. Under conditions of complete rest, i.e., in all except the lightest phases of sleep, the tremor disappears, as do most abnormal tremors except various forms of myoclonus.
Parkinsonian tremor is “alternating” in the sense that it takes the form of flexion–extension or abduction–adduction of the fingers or the hand; pronation–supination of the hand and forearm is also a common presentation. Flexion–extension of the fingers in combination with adduction–abduction of the thumb yields the characteristic “pill-rolling” tremor of Parkinson disease. It continues and may worsen while the patient walks, unlike essential tremor; indeed, it may first become apparent to the patient during walking. When the legs are affected, the tremor takes the form of a flexion–extension movement of the foot, sometimes the knee. In the jaw and lips, it is seen as up-and-down and pursing movements, respectively. The eyelids, if they are closed lightly, tend to flutter rhythmically (blepharoclonus), and the tongue, when protruded, may move in and out of the mouth at about the same tempo as the tremor elsewhere.
The cogwheel effect, a ratchet-like interruption perceived by the examiner on passive movement of an extremitiy (the Negro sign). It is said by many authors to be no more than a palpable tremor superimposed on rigidity and as such, is not specific for Parkinson disease although it is most prominent in that condition. This explanation is called into question by the numerous cases in which Parkinson patients display minimal or no resting tremor but nonetheless have the cogwheel phenomenon as mentioned in Chap. 4. Cogwheeling can be brought out by having the patient engage the opposite limb, such as tracing circles in the air; this Froment sign, was originally described in essential tremor.
The parkinsonian tremor frequency is surprisingly constant over long periods, but the amplitude is variable. Emotional stress augments the amplitude and may add to the effects of an enhanced physiologic or essential tremor. With advance of the disease, increasing rigidity of the limbs obscures or reduces it. It is curious how little the tremor interferes with voluntary movement; for example, it is possible for a tremulous patient to raise a full glass of water to his lips and drain its contents without spilling a drop; this is not always the case with “benign” essential tremor, as already emphasized.
Almost always in Parkinson disease, the tremor is asymmetric and at the outset may be entirely unilateral. The tremor of postencephalitic parkinsonism (which is now virtually extinct) often had greater amplitude and involved proximal muscles. In neither disease is there a close correspondence between the degree of tremor and the degree of rigidity or akinesia. A bilateral parkinsonian type of tremor may also be seen in elderly persons without akinesia, rigidity, or mask-like facies. In some of these patients, the tremor is followed years later by the other manifestations of Parkinson disease, but in others it is not, the tremor remaining unchanged for decades or progressing very slowly, unaffected by anti-Parkinson drugs. This probably equates with the earlier mentioned alternate-beat type of essential tremor. Patients with the familial (wilsonian) or acquired form of hepatocerebral degeneration may also show a tremor of parkinsonian type, usually mixed with ataxic tremor and other extrapyramidal motor abnormalities. An alternating tremor may be seen in toxic-drug induced parkinsonism but it is relatively symmetric and tends not to be a prominent feature.
Parkinsonian tremor is suppressed to some extent by the anticholinergic drugs benztropine, trihexyphenidyl, and other anticholinergic drugs such as ethopropazine, a phenothizine derivative; it is also suppressed less consistently but sometimes impressively by L-dopa and dopaminergic agonist drugs, which are the mainstays of treatment for Parkinson disease as discussed in Chap. 39.
The situation is made more difficult because a parkinsonian tremor is often associated with an additional tremor of faster frequency; the latter is of essential type and responds better to beta-blocking drugs than to anti-Parkinson medications. Stereotactic lesions or electrical stimulation in the basal ventrolateral nucleus of the thalamus diminishes or abolishes tremor contralaterally; other stimulation sites such as the internal segment of the globus pallidus and the subthalamic nucleus are also effective but possibly to a lesser degree. Chapter 39 discusses treatment of Parkinson disease in greater detail.
As discussed in Chap. 5, the word intention is ambiguous in this context because the tremor itself is not intentional and occurs not when the patient intends to make a movement but only during the most demanding phases of active performance. In this sense it is a kinetic or action tremor, but the latter term has connotations of the essential tremor to neurologists, as described earlier. The term ataxic is a suitable substitute for intention, because this tremor is always combined with cerebellar ataxia and adds to it, as described in Chap. 5. Its salient feature is that it requires for its full expression the performance of an exacting, precise, projected movement. The tremor is absent when the limbs are inactive and during the first part of a voluntary movement but as the action continues and fine adjustments of the movement are demanded (e.g., in touching the tip of the nose or the examiner’s finger), an irregular, more or less rhythmic (2- to 4-Hz) interruption of forward progression with side-to-side oscillation appears and may continue for several beats after the target has been reached. Unlike essential and parkinsonian tremors, the oscillations occur in more than one plane but are mainly horizontal and perpendicular to the trajectory of movement. The tremor and ataxia may seriously interfere with the patient’s performance of skilled acts. In some patients there is a rhythmic oscillation of the head on the trunk (titubation), or of the trunk itself, at approximately the same rate. As already indicated, this type of tremor points to disease of the cerebellum or its connections, particularly via the superior cerebellar peduncle, but certain peripheral nerve diseases may occasionally simulate it.
There is another, higher amplitude tremor associated with cerebellar ataxia, in which every movement, even lifting the arm slightly or maintaining a static posture with the arms held out to the side, results in a wide-ranging, rhythmic 2- to 5-Hz “wing-beating” movement, sometimes of sufficient force to throw the patient off balance. In such cases, the lesion is usually in the midbrain, involving the rostral projections of the dentatorubrothalamic fibers and the medial part of the ventral tegmental reticular nucleus. Because of the location of the lesion in the region of the red nucleus, Holmes originally called this a rubral tremor. However, experimental evidence in monkeys indicates that the tremor is produced not by a lesion of the red nucleus per se but by interruption of dentatothalamic fibers that traverse this nucleus—i.e., the cerebellar efferent fibers that form the superior cerebellar peduncle and brachium conjunctivum (Carpenter). This type of tremor is seen most often in patients with multiple sclerosis and Wilson disease, occasionally with vascular and other lesions of the tegmentum of the midbrain and subthalamus, and rarely as an effect of antipsychosis medications. Beta-adrenergic blocking agents, anticholinergic drugs, and L-dopa have little therapeutic effect. It is abolished by a surgical or ischemic lesion in the opposite ventrolateral nucleus of the thalamus. Thalamic stimulation may be particularly helpful in severe cases that are the result of demyelinating lesions in the cerebellar peduncles.
Chapter 5 and the section further on, “Pathophysiology of Tremor,” discuss the mechanisms involved in the production of intention, or ataxic tremor.
This is a strongly familial episodic tremor disorder of the chin and lower lip that begins in childhood and may worsen with age. Psychic stress and concentration are known to precipitate the movements, which are described by Danek as “trembling.” Rare instances involve other facial muscles. The disorder must be distinguished from a similar tremor of the chin that is part of essential tremor, facial myokymia or fasciculations, and palatal tremor. The disorder results from a mutation on chromosome 9.
This is a rare but striking tremor isolated to the legs that is remarkable by its occurrence only during quiet standing and its cessation almost immediately on walking. It is difficult to classify and more relevant to disorders of gait than it is to tremors of other types. The frequency of the tremor has been recorded as approximately 14 to 16 Hz, making it difficult to observe and more easily palpable. Nonetheless, it may produce considerable disability as the patient attempts to stabilize himself in response to the tremulousness. An important accompanying feature is the sensation of severe imbalance, which causes the patient to assume a widened stance while standing; these patients are unable to walk a straight line (tandem gait). We have observed prominent tonic contraction of the legs during standing, seemingly in an attempt to overcome imbalance (see Heilman; and Thompson, Rothwell, Day et al). The arms are affected little or not at all. Often the first step or two when the patient begins to walk are halting, but thereafter, the gait is entirely normal. Because falls are infrequent, the condition is often attributed to hysteria. Tremulousness is not present when the patient is seated or reclining, but in the latter positions it can be evoked by strong contraction of the leg muscles against resistance.
Electromyographic recordings demonstrate rhythmic cocontraction of the gastrocnemius and anterior tibialis muscles. Although some authors, such as Wee and colleagues, have classified the disorder as a type of essential tremor, most of its characteristics suggest otherwise. Sharott and coworkers consider it an exaggerated physiologic tremor in response to imbalance; others have found an intrinsic rhythm at approximately 16 Hz generated by the damaged spinal cord in patients with myelopathy, suggesting a spinal origin for the tremor.
Some cases have responded to the administration of clonazepam, gabapentin, primidone, or sodium valproate alone or in combination but it often proves difficult to treat. A few intractable cases have been treated with an implanted spinal cord stimulator (Krauss et al, 2005).
Tremors may be an incipient feature of dystonia. When the underlying dystonic posturing is not overt, the tremor may be ascribed to the essential variety or to hysteria. Dystonic tremor is focal, superimposed, for example on torticollis, or it may be evident in a dystonic hand. The movement is not entirely rhythmic, sometimes jerky, and often intermittent. These cases are discussed further on in the section on focal dystonia. In addition, a fair number of patients with dystonia have an essential tremor.
Tremor may be a quite dramatic manifestation of hysteria. It simulates many types of organic tremor, thereby causing difficulty in diagnosis. Psychogenic tremors are usually restricted to a single limb, often in the dominant hand; they are gross in nature, are less regular than the common static or action tremors, and diminish in amplitude or disappear if the patient is distracted as, for example, when asked to make a complex movement with the opposite hand. If the examiner restrains the affected hand and arm, the tremor may move to a more proximal part of the limb or to another part of the body (“chasing the tremor”). Other useful features in identifying hysterical tremor are exaggeration of the tremor by loading the limb—e.g., by having the patient hold a book or other heavy object—which reduces almost all other tremors with exception of those produced by polyneuropathy. Hysterical tremor persists in repose and during movement and is less subject than nonhysterical tremors to the modifying influences of posture and willed movement. Tremors of this type often acquire the frequency of a willed movement in a different limb. This can be brought out by asking the patient to rhythmically tap with the unaffected limb.
Not all tremors correspond exactly with those described above and several of them may coexist. There is frequently a variation in one or more of the particulars from the typical pattern, or one type of tremor may show a feature ordinarily considered characteristic of another. In some parkinsonian patients, for example, the tremor is accentuated rather than dampened by active movement; in others, the tremor may be very mild or absent in repose and become obvious only with movement of the limbs. As mentioned above, a patient with a typical parkinsonian tremor may, in addition, show a fine essential tremor of the outstretched hands and occasionally even an element of ataxic tremor as well. In a similar way, essential or familial tremor may, in its advanced stages, assume the aspects of a cerebellar tremor. Further examples include patients with essential or familial tremor or with cerebellar degeneration who display a rhythmic parkinsonian tremor in relation to sustained postures.
In patients with tremor of either the parkinsonian, postural, or intention type, Narabayashi has recorded rhythmic burst discharges of unitary cellular activity in the nucleus intermedius ventralis of the thalamus (as well as in the medial pallidum and subthalamic nucleus) synchronous with the beat of the tremor. Neurons that exhibit the synchronous bursts are arranged somatotopically and respond to kinesthetic impulses from the muscles and joints involved in the tremor. A stereotaxic lesion in this region of the thalamus abolishes the tremor. The effectiveness of a thalamic lesion may be a result of interruption of pallidothalamic and dentatothalamic projections or, more likely, of projections from the ventrolateral thalamus to the premotor cortex, as the impulses responsible for tremor are ultimately transmitted by the lateral corticospinal tract. Some of what is known about the physiology of specific tremors is noted in the following paragraphs.
To date, only a few cases of essential tremor have been examined postmortem, and these have disclosed no consistent lesion to which the tremor could indisputably be attributed (Herskovits and Blackwood; Cerosimo and Koller). A singular case of a 90-year-old woman studied by Louis and colleagues, demonstrated more extensive cerebellar cortical and dentate nucleus cell loss and reactive changes than had been previously recognized.
The question of the existence and locus of a generator for essential tremor as opposed to the unbalancing of a feedback loop system is unresolved. As indicated by McAuley, various studies that demonstrate rhythmic activity in the cortex corresponding to the tremor activity are more suggestive of a common source elsewhere than of a primary generator in the cortex. Based on electrophysiologic recordings in patients, two likely origins of oscillatory activity are the olivocerebellar circuits and the thalamus. Whether a particular structure possesses an intrinsic rhythmicity or, as currently favored, the tremor is an expression of reciprocal oscillations in circuits of the dentato–brainstem–cerebellar or thalamic–tegmental systems is not at all clear. Studies of blood flow in patients with essential tremor by Colebatch and coworkers affirm that the cerebellum is rhythmically activated; on this basis they argue that there is a release of an oscillatory mechanism in the olivocerebellar pathway. Dubinsky and Hallett demonstrated that the inferior olives also become hypermetabolic when essential tremor is activated, but this has been questioned by Wills and colleagues who recorded increased blood flow in the cerebellum and red nuclei, but not in the olive. These proposed mechanisms are reviewed by Elble and serve to emphasize the points made here.
Although this disorder is familial, a single genetic site has not yet been established; several candidate polymorphisms are promising.
The anatomic basis of parkinsonian tremor is not known. In Parkinson disease, the visible lesions predominate in the substantia nigra, and this was true also of the postencephalitic form of the disease. In animals, however, experimental lesions confined to the substantia nigra do not result in tremor; neither do lesions in the striatopallidum. Moreover, not all patients with lesions of the substantia nigra have tremor; in some there is only bradykinesia and rigidity. In a group of patients poisoned with the toxin MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine), a meperidine analogue that destroys the neurons of the substantia nigra pars compacta (see Chaps. 4 and 39), only half developed a tremor, which had more of the characteristics of a proximal action or postural tremor than of a rest tremor as discussed by Burns and colleagues. In all likelihood, these inconsistencies reflect the complex influence of dopamine on a number of basal ganglionic structures outlined in Chap. 4.
Ward and others have produced a Parkinson-like tremor in monkeys by placing a lesion in the ventromedial tegmentum of the midbrain, just caudal to the red nucleus and dorsal to the substantia nigra. He postulated that interruption of the descending fibers at this site liberates an oscillating mechanism in the lower brainstem; this presumably involves limb innervation via the reticulospinal pathway. Alternative possibilities are that the lesion in the ventromedial tegmentum interrupts the brachium conjunctivum, or a tegmental-thalamic projection, or the descending limb of the superior cerebellar peduncle, which functions as a link in a dentatoreticular-cerebellar feedback mechanism, a hypothesis similar to the one proposed for essential tremor (see Fig. 5-3). The differential effect of drugs on tremor and bradykinesia suggest that they must have separate mechanisms.
This has been produced in monkeys by inactivating the deep cerebellar nuclei or by sectioning the superior cerebellar peduncle or the brachium conjunctivum below its decussation. A lesion of the nucleus interpositus or dentate nucleus causes an ipsilateral tremor of ataxic type, as one might expect, associated with other manifestations of cerebellar ataxia. In addition, such a lesion gives rise to a “simple tremor,” which is the term that Carpenter applied to a “resting” or parkinsonian tremor. He found that the latter was most prominent during the early postoperative period and was less enduring than ataxic tremor. Nevertheless, the concurrence of the two types of tremor and the fact that both can be abolished by ablation of the contralateral ventrolateral thalamic nucleus suggest that they have related neural mechanisms, at least in monkeys.
This is a rare disorder consisting of rapid, rhythmic, involuntary movements of the soft palate. For many years it was considered to be a form of uniphasic myoclonus (hence the terms palatal myoclonus and palatal nystagmus). Because of the persistent rhythmicity, it is now classified as a tremor. There are two forms of this movement, according to Deuschl and colleagues. One is essential palatal tremor that reflects the rhythmic activation of the tensor veli palatini muscles; it has no known pathologic basis. The palatal movement may impart a repetitive audible click, which ceases during sleep. The second, more common form is a symptomatic palatal tremor caused by a diverse group of brainstem lesions that interrupt the central tegmental tract(s); these columns contain descending fibers from midbrain nuclei to the inferior olivary complex (a component of the Guillain-Mollaret triangle described below and in Chap. 5 and Fig. 5-3). The frequency of the tremor varies greatly and is 26 to 420 cycles per minute in the essential form and 107 to 164 cycles per minute in the symptomatic form.
Symptomatic palatal tremor, in contrast to the essential type and all other tremors, persists during sleep and is sometimes associated with ocular myoclonus that is synchronized with the palatal movements. In some cases, the pharynx as well as the facial and extraocular muscles (pendular or convergence nystagmus), diaphragm, vocal cords, and even the muscles of the neck and shoulders partake of the persistent rhythmic movements. A similar phenomenon, in which contraction of the masseters occurs concurrently with pendular ocular convergence, has been observed in Whipple disease (oculomasticatory myorhythmia).
Magnetic resonance imaging (MRI) reveals no lesions to account for essential palatal tremor; in the symptomatic form, however, there are tegmental brainstem lesions and conspicuous enlargement of the inferior olivary nucleus unilaterally or bilaterally. With unilateral palatal tremor, it is the contralateral olive that becomes enlarged. It has been proposed that the lesions in the symptomatic form interrupt the circuit (dentate nucleus–brachium conjunctivum–red nucleus-central tegmental tract–olivary nucleus–dentate nucleus) that Lapresle and Ben Hamida called the triangle of Guillain-Mollaret (Fig. 5-3). The lesions have been vascular, neoplastic, especially demyelinating, or traumatic, and have been found mainly in midbrain or pontine portions of the central tegmental fasciculus.
The physiologic basis of palatal tremor remains conjectural. Matsuo and Ajax postulated a denervation hypersensitivity of the inferior olivary nucleus and its dentate connections, but others have suggested that the critical event is denervation not of the olive but of the nucleus ambiguus and the dorsolateral reticular formation adjacent to it. Dubinsky and colleagues have suggested that palatal tremor may be based on the same mechanism as postural tremor—i.e., presumably a disinhibition of the olive and a rhythmic coupling of neurons in the olive induced by a lesion of the dentato-olivary pathway.
The use of drugs in treating this movement disorder has met with variable success. Clonazepam (0.25 to 0.5 mg/d, increasing gradually to 3.0 to 6.0 mg/d), sodium valproate (250 mg/d, increasing to 1,000 mg/d), and gabapentin (up to 2,100 mg) have suppressed the movement in some cases, particularly the last of these drugs, which reportedly has had a dramatic effect in some patients. Also, tetrabenazine and haloperidol have been helpful on occasion. Selective injection of the palatal muscles with botulinum toxin, while technically demanding, affords modest relief; it is particularly helpful in eliminating the annoying ear clicking.
Asterixis
The movement disorder known as asterixis was described by Adams and Foley in patients with hepatic encephalopathy but it occurs with a variety of systemic metabolic disorders. It consists of arrhythmic lapses of sustained posture that allow gravity or the inherent elasticity of muscles to produce a movement, which the patient then corrects, sometimes with overshoot. Later, Leavitt and Tyler and then Young and Shahani demonstrated that the initial interruption or lapse in posture is associated with EMG silence for a period of 35 to 200 ms. By interlocking EMG and electroencephalogram (EEG) recordings, Ugawa et al found that a sharp wave, probably generated in the motor cortex, immediately precedes the period of EMG silence. This confirmed that asterixis differs physiologically from both tremor and myoclonus, with which it was formerly confused; it has incorrectly been referred to as a “negative tremor.”
Asterixis is most readily evoked by asking the patient to hold his arms outstretched with hands dorsiflexed or to dorsiflex the hands and extend the fingers while resting the forearms on the bed or the arms of a chair. Flexion movements of the hands may then occur arrhythmically once or several times a minute. The same lapses in sustained muscle contraction can be provoked in any muscle group—including, for example, the protruded tongue, the closed eyelids, or the flexed trunk muscles. Sometimes, asterixis can be elicited best by asking the patient to place his hand flat on a table and raise the index finger.
This sign was first observed in patients with hepatic encephalopathy but was later noted with hypercapnia, uremia, and other metabolic and toxic encephalopathies. Asterixis may also be evoked by phenytoin and other anticonvulsants, usually indicating that these drugs are present in excessive concentrations. Similar rapid lapsing movements of the head or arms sometimes appear during drowsiness in normal persons (“nodding off”).