Disorders of Stance and Gait: Introduction
Certain disorders of motor and sensory function manifest themselves most clearly as impairments of upright stance and locomotion; their evaluation depends on knowledge of the neural mechanisms underlying the peculiarly human function of standing and bipedal walking. The analysis of stance, carriage, and gait is a rewarding exercise; with some experience, the examiner can sometimes reach a neurologic diagnosis merely by noting the manner in which the patient enters the office. Considering the frequency of falls that result from gait disorders and their consequences, such as hip fracture, and the resultant need for hospital and nursing home care, this is an important subject for all physicians. The substantial dimensions of the social and economic problem of falls and the elderly have been described by Tinetti and Williams.
Normal Gait
Obviously, gait varies considerably from one person to another and it is a commonplace observation that a person may be identified by the sound of his footsteps, notably the pace and the lightness or heaviness of tread. The manner of walking and the carriage of the body may even provide clues to an individual’s personality and occupation. Sherlock Holmes expressed pride in his talent for reading such clues. It is said that Charcot could often make the correct diagnosis, even before seeing the patient, based on the sound of patient walking down the hallway on the way to the examining room. Furthermore, the gaits of men and women differ, a woman’s steps being quicker and shorter. The changes in stance and gait that accompany aging—the slightly stooped posture and slow, stiff tread as described in Chap. 29, on aging—are so familiar that they are not perceived as abnormalities.
The normal gait seldom attracts attention but it should be observed with care if slight deviations from normal are to be appreciated. The body is erect, the head is straight, and the arms hang loosely and gracefully at the sides, each moving rhythmically forward with the opposite leg. The feet are slightly externally rotated, the steps are approximately equal, and the medial malleoli almost touch as each foot passes the other. The medial edges of the heels, as they strike the ground with each step, lie almost along a straight line. As each leg moves forward, there is coordinated flexion of the hip and knee, dorsiflexion of the foot, and a barely perceptible elevation of the hip, so that the foot clears the ground. Also, with each step, the thorax advances slightly on the side opposite the swinging lower limb. The heel strikes the ground first, and inspection of the shoes will show that this part is most subject to wear.
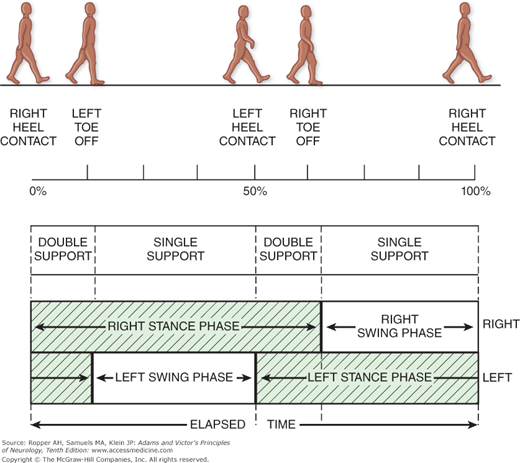
The normal gait cycle, defined as the period between successive points at which the heel of the same foot strikes the ground, is illustrated in Fig. 7-1, based on the studies of Murray and coworkers, and of Olsson. In this figure, the cycle is initiated by the heel strike of the right foot. The stance phase, during which the foot is in contact with the ground, occupies 60 to 65 percent of the cycle. The swing phase begins when the right toes leave the ground. For 20 to 25 percent of the walking cycle, both feet are in contact with the ground (double-limb support). In later life, when the steps shorten and the cadence (the rhythm and number of steps per minute) decreases, the proportion of double-limb support increases (see further on). Surface electromyograms show an alternating pattern of activity in the legs, predominating in the flexors during the swing phase and in the extensors during the stance phase.
Figure 7-1.
The normal gait cycle, based on the studies of Olsson and of Murray et al. See text for details.
When analyzed in greater detail, the requirements for locomotion in an upright, bipedal position may be reduced to the following elements: (1) antigravity support of the body, (2) stepping, (3) the maintenance of equilibrium, and (4) a means of propulsion. Locomotion is impaired in the course of neurologic disease when one or more of these mechanical principles are prevented from operating normally.
The muscles of greatest importance in maintaining the erect posture are the erector spinae and the extensors of the hips and knees. The upright support of the body is provided by righting and antigravity reflexes, which allow a person to arise from a lying or sitting position to an upright bipedal stance and to maintain firm extension of the knees, hips, and back, modifiable by the position of the head and neck. These postural reflexes depend on the afferent vestibular, somatosensory (proprioceptive and tactile), and visual impulses, which are integrated in the spinal cord, brainstem, and basal ganglia. Transection of the neuraxis between the red and vestibular nuclei leads to exaggeration of these antigravity reflexes—decerebrate rigidity.
Stepping, the second element, is a basic movement pattern present at birth and integrated at the spinal midbrain and diencephalic levels. It is elicited by contact of the sole with a flat surface and a shifting of the center of gravity—first laterally onto one foot, allowing the other to be raised, and then forward, allowing the body to move onto the advancing foot. Rhythmic stepping movements can be initiated and sustained in decerebrate or “spinal” cats and dogs. This is accomplished through the activity of interneurons that are organized as rhythmic “locomotor generators,” akin to the pattern generators that permit the rhythmic movement of wings or fins. There is no clear evidence for a similar system of locomotor control in monkeys or humans, in whom the spinal mechanisms for walking cannot function independently of vaguely organized higher command centers. The latter are located in the posterior subthalamic region, caudal midbrain tegmentum, and pontine reticular formation; they control the spinal gait mechanisms through the reticulospinal, vestibulospinal, and tectospinal pathways in the ventral cord (see Eidelberg and colleagues and Lawrence and Kuypers). In the human, the brainstem locomotor regions are also activated by frontal cortical areas.
The frontal lobe is absolutely integral to initiating and engaging the gait cycle. The presence of a true “gait center” in the cerebrum is uncertain, although frontal lesions can devastate gait as discussed further on. Most often, it has been the supplementary motor areas relating to the legs (superior frontal gyri on both sides) that are implicated as pointed out by Della Sala and colleagues but Benson and coworkers have emphasized that the frontal periventricular areas are disproportionately involved when subcortical vascular disease compromises walking. The gait disorder of frontal lobe disease has a number of special characteristics including difficulty with starting to walk, short steps, widened base, difficulty lifting the feet off the floor (the magnetic gait) and a tendency to fall backwards (retropulsion). In all likelihood, the medial frontal lobes embody automatic programs for walking that are intimately tied to adjacent networks in the striatum.
Equilibrium involves the maintenance of balance in relation to gravity and to the direction of movement in order to retain a vertical posture. The center of gravity during the continuously unstable equilibrium that prevails in walking must shift within narrow limits from side to side and forward as the weight is borne first on one foot, then on the other. This is accomplished through the activity of highly sensitive postural and righting reflexes that have both peripheral (stretch reflexes) and central (vestibulocerebellar reflexes) components. These reflexes are activated within 100 ms of each shift in the support surface and require reliable afferent information from the visual, vestibular, and proprioceptive systems.
Propulsion is provided by leaning forward and slightly to one side and permitting the body to fall a certain distance before being checked by the support of the leg. Here, both forward and alternating lateral movements must occur. But in running, where at one moment both feet are off the ground, a forward drive or thrust by the trailing leg is also required.
Abnormal Gaits
Because normal body posture and locomotion require intact vestibular function, proprioception, and vision (we see where we are going and adjust our steps), the effects of deficits in these senses are worth noting. A blind person—or a normal one who is blindfolded or walks in the dark—moves cautiously, with arms slightly forward to avoid collisions, and shortens his step slightly on a smooth surface; with shortening of the step, there is less rocking of the body and the gait is unnaturally stiff and cautious.
Patients with a chronic vestibulopathy show unsteadiness in standing and walking, often without widening their base, and an inability to descend stairs without holding onto the banister. They complain of a particular type of imbalance, usually with movement but at times when standing still—a sensation that may be likened to being on the deck of a rolling ship. Running and turning quickly are even more impaired, with lurching in all directions. The patient has great difficulty in focusing his vision on a fixed target when he is moving or on a moving target when he is either stationary or moving. When the body is in motion or the head is moved suddenly, objects in the environment may appear momentarily blurred or actually jiggle up and down or from side to side (oscillopsia). Driving a car or reading on a train is difficult or impossible; even when walking, the patient may need to stop in order to read a sign. These abnormalities indicate a loss of stabilization of ocular fixation by the vestibular system during body movements (the vestibular-ocular reflex, or VOR). An elderly person has difficulty compensating for these abnormalities. Proof that the gait of such persons with vestibulopathy is dependent on visual clues comes from their performance blindfolded or in the dark, when their unsteadiness and staggering increase to the point of falling. When standing with eyes closed, they sway more than normal but generally do not fall over (i.e., they do not have a Romberg sign, as described below). The diagnosis is confirmed by testing labyrinthine function (caloric and rotational testing, electronystagmography, and posture platform testing).
Chronic disorders of vestibular function in relation to gait disorders are most often the result of prolonged administration of aminoglycoside antibiotics or other toxic medications, which destroy the hair cells of the vestibular labyrinth. Vestibular suppressants, such as meclizine and similar medications, mostly anticholinergic and antihistaminic that are available over the counter, can lead to decreased function of the vestibular system, with a persistent gait disorder, if used for more than a few weeks. This also occurs in some patients in the late stages of Ménière disease and, infrequently, for no definable reason. The literature is replete with references to a “multimodal” gait disorder in the elderly that is the result of an ostensible aging of the vestibular organ, together with impaired proprioceptive function caused by distal neuropathy in the elderly, and impaired vision.
A loss of proprioception—as occurs in patients with severe large-fiber polyneuropathy, posterior nerve root lesions (e.g., tabes dorsalis, lumbosacral compression), or interruption of the posterior columns in the spinal cord (multiple sclerosis, vitamin B12 deficiency, spondylotic or tumor compression)—abolishes or seriously impairs the capacity for independent locomotion. After years of training, such patients still have difficulty in initiating gait and in forward propulsion. As J. Purdon Martin illustrated, they hold their hands slightly in front of the body, bend the body and head forward, walk with a wide base and irregular, uneven steps, but still rock the body. If they are tilted to one side, they fail to compensate for their abnormal posture. If they fall, they cannot rise without help; they are sometimes unable to crawl or to get into an “all fours” posture. They have difficulty in getting up from a chair. When standing, if instructed to close their eyes, they sway markedly and fall (Romberg sign); this sign is the clearest indication that the origin of the problem is a loss of proprioceptive sensibility.
With lesions of the basal ganglia, both in monkeys and in humans, the posture of the body and the postural responses to perturbations in equilibrium are faulty. There is difficulty in taking the first step; once it is taken, and in extreme cases, the body pitches forward and a fall can be prevented only by catch-up stepping (propulsive festination). Similarly, a step backward may induce a series of quickening steps in that direction (retropulsive fesitnation). Corrective righting reflexes are clearly faulty when the patient is pushed off balance (Denny-Brown). These abnormalities are elaborated further on, under “Parkinsonian and Festinating Gait.”
Pain in the hips or knees can lead to a disorder (antalgic gait) that can be challenging to distinguish from neurological causes of gait problems. Slowness of the swing phase and reduction in the amount of time spent with the painful limb in contact with the ground may be clues to recognizing rheumatological and orthopedic causes of a gait disorder.
When confronted with a disorder of gait, the examiner must observe the patient’s stance and the dominant positions of the legs, trunk, and arms, and their interrelationship. It is good practice to watch patients as they walk into the examining room, when they are apt to walk more naturally than during the performance of commanded tasks. They should be asked to stand with feet together and head erect, with eyes open and then closed. A normal person can stand with feet together and eyes closed while moving the head from side to side, a test that blocks both visual and vestibular cues and induces certain compensatory trunk and leg movements that depend solely on proprioceptive afferent mechanisms (Ropper). As already mentioned, the Romberg sign—marked swaying or falling with the eyes closed but not with the eyes open—usually indicates a loss of postural sense, not of cerebellar function, although with vestibular or cerebellar disease there may be an exaggeration of swaying. Swaying due to of nervousness may be overcome by asking the patient to touch the tip of his nose alternately with the forefinger of one hand and then the other.
Next, the patient should be asked to walk, noting in particular any hesitation in starting and negotiating turns, width of base, length of stride, foot clearance, arm swing, and cadence. A tendency to veer to one side, as occurs with unilateral cerebellar or vestibular disease, can be brought out by having the patient walk around a chair. When the affected side is toward the chair, the patient tends to walk into it; when it is away from the chair, there is a veering outward in ever-widening circles. More delicate tests of gait are walking a straight line heel to toe (“tandem walking test”), walking backward, and having the patient arise quickly from a chair, walk briskly, stop and turn suddenly, walk back, and sit down again. Turning the patient three full revolutions with eyes open, first right and then left, each time followed by asking the patient to walk naturally, allows the examiner to stress the vestibular apparatus and to compare the two sides. The patient affected by a vestibular or cerebellar process will veer to the side of a lesion. Marching in place with eyes closed (Unterberger, or Fukada stepping tests) also reveals a rotation in the yaw plane (rotation around the vertical axis), indicating an asymmetrical disorder in the plane of the horizontal semicircular ducts or their connections.
It is instructive to observe the patient’s postural reaction to a sudden push or tug backward at the shoulders and forward or to the side. With postural instability of any type there is a delay or inadequacy of corrective actions. Finally, the patient may be asked to hop on one leg and to jog. If all these tests can be successfully executed, it may be assumed that any difficulty in locomotion is not because of impairment of a proprioceptive, labyrinthine-vestibular, basal ganglionic, or cerebellar mechanism. Detailed musculoskeletal and neurologic examination is then necessary to determine which of several other disturbances of function is responsible for the patient’s disorder of gait.
The following types of abnormal gait (Table 7-1) are so distinctive that, with practice, they can be recognized at a glance and interpreted correctly.
CADENCE | STEP LENGTH | BASE | OTHER ASSOCIATED SIGNS | |
|---|---|---|---|---|
Cerebellar | Irregular | Slightly short | Wide | Erratic shifting of weight and step |
Sensory ataxic (tabetic) | Normal | Short | Slightly wide | Excessive force in step resulting in stamping of feet; Romberg sign |
Steppage | Normal | Normal | Normal | Overlifting and slapping of feet |
Plegic | Slow | Short | Narrow | Circumduction and scraping of affected leg(s) |
Dystonic | Slow | Normal | Erratic | Twisting athetoid movements interrupt walking |
Parkinsonian-festinating | Slow until festination | Short | Normal | Quickening step, forward leaning, shuffling, may have trouble with gait initiation |
Waddling-myopathic | Normal | Normal | Slightly wide | Overlifting of hip(s) |
Toppling | Slow until fall | Short | Widened (protective) | Sudden loss of balance |
Normal pressure hydrocephalus | Slow | Short | Slightly wide | Numerous problems with axial body movement |
Frontal lobe | Slow | Greatly shortened | Slightly wide (protective) | Difficulty starting and stopping; tendency for feet to “stick” to floor |
Aging and marche à petit pas | Slow | Slightly shortened | Slightly widened | Cautious, slight forward lean |
The main features are a wide base (separation of legs), unsteadiness, irregularity of steps, and lateral veering. Steps are uncertain, some are shorter and others longer than intended, and the patient may compensate for these abnormalities by shortening his steps or even keeping both feet on the ground simultaneously, which creates the appearance of shuffling. Cerebellar gait is often referred to as “reeling” or “drunken,” but these terms are not correct and are characteristic instead of intoxication and of certain types of labyrinthine disease, as explained further on.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree