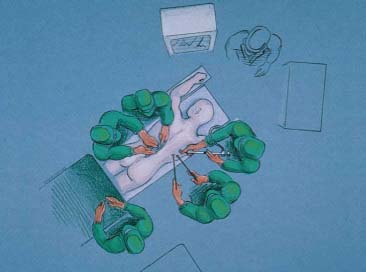
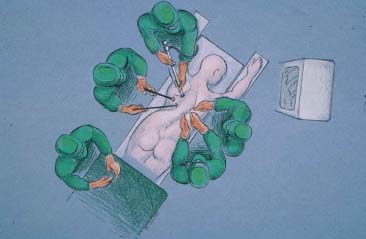
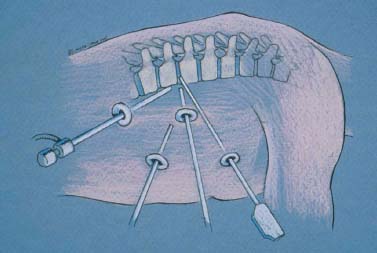
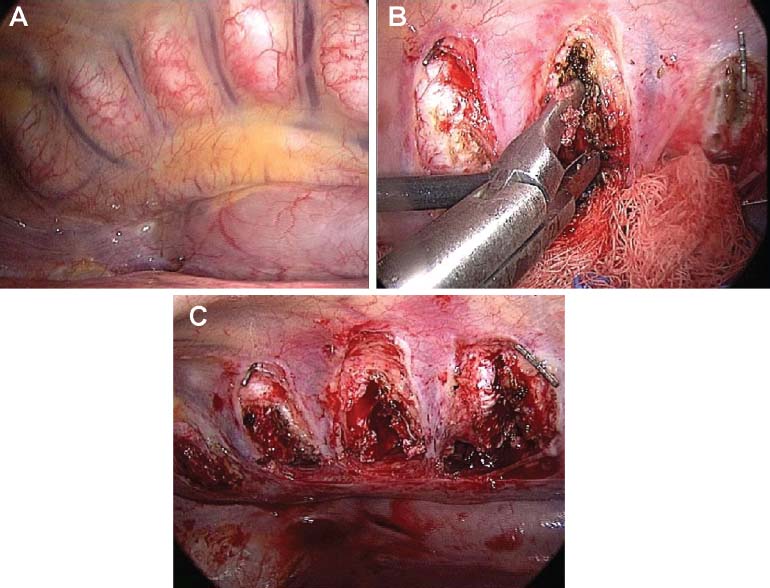
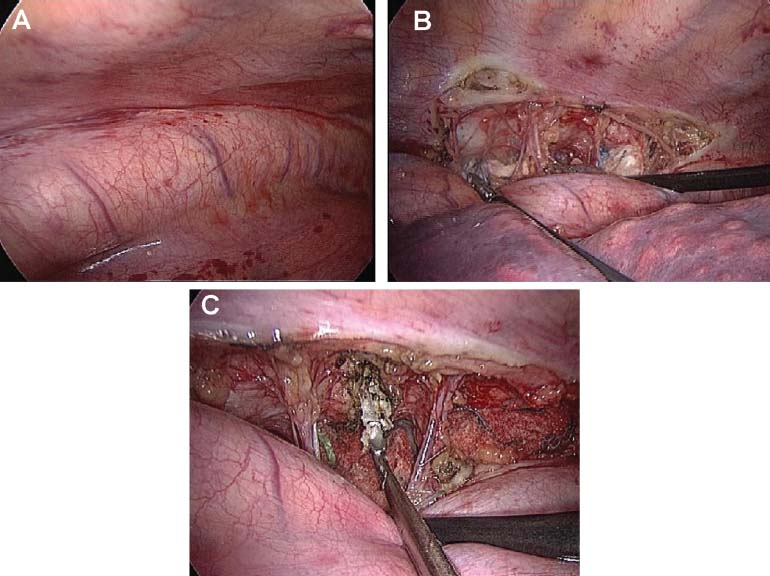
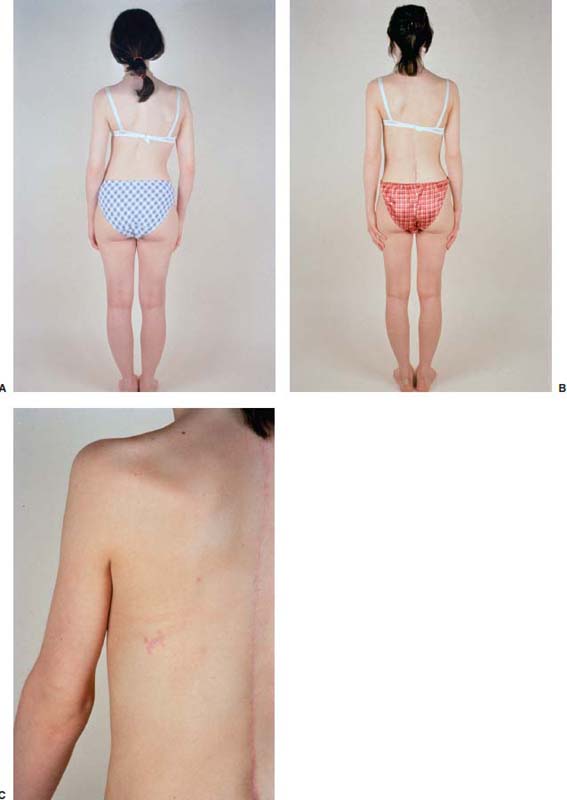
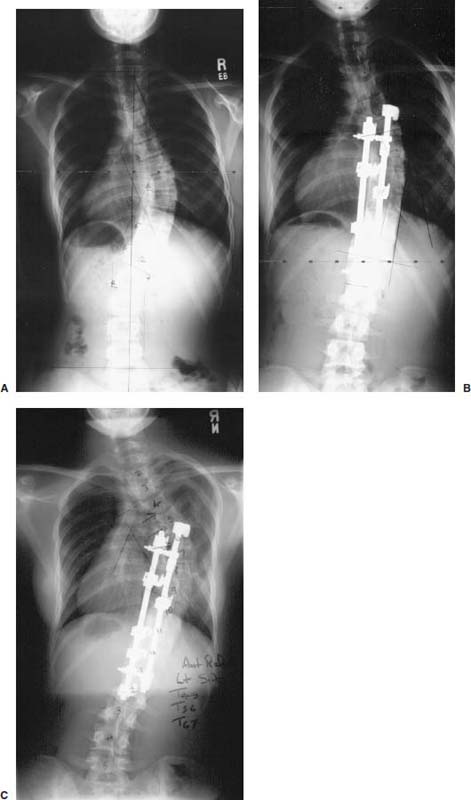
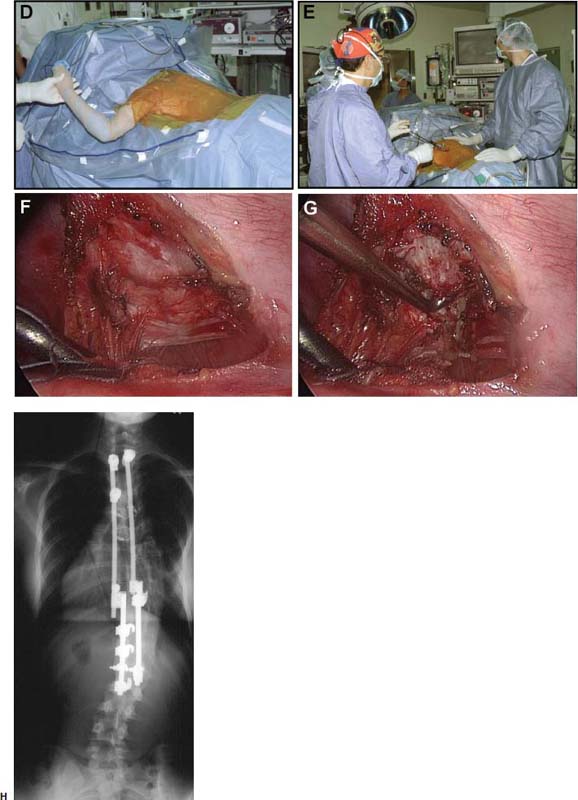
In deformity surgery, anterior release and bone grafting of the thoracic spine is instrumental to maximizing correction, reducing the pseudoarthrosis rate, and preventing further progression of the deformity. Anterior releases were traditionally achieved with the patient in the lateral decubitus position through an open thoracotomy, after rib resection and spreading, on the convex side for scoliotic or on either side for kyphotic deformities. During the thoracotomy, the thoracic organs and tissues are exposed and manipulated and may become desiccated. As a consequence of thoracotomy, patients may develop a measurable reduction in pulmonary and shoulder girdle function and experience significant chronic incisional pain. Thoracotomy is clearly associated with distinct issues related to pain, cosmesis, and morbidity. Video-assisted endoscopic transthoracic exposures to facilitate spinal releases, diskectomies, and osteotomies have been performed with the patient positioned in the lateral decubitus position, mimicking open thoracotomy.1,2 By virtue of improved visualization (due to illumination and magnification of the operative site by the video system), less postoperative incisional pain (due to less muscle dissection and no rib spreading), and more cosmetically acceptable scars, these advances have reduced the thoracotomy-related consequences. Prone position endoscopic transthoracic exposures have been used even more recently to facilitate deformity correction.3 Although the lateral position affords the surgeon a more familiar anatomical alignment and approach, the prone position allows the mediastinal organs to fall away from the spine, obviating the need for retraction, and facilitates simultaneous anterior posterior procedures, eliminating the need for staged or subsequent surgeries. Prior to embarking on any endoscopic exposure, the surgeon must be familiar with open anterior spinal anatomy and surgical techniques. The surgical procedure is the same, but the methods are different enough to challenge even the most experienced spinal surgeon. Whether using the lateral or prone position, the loss of depth perception and the necessity for triangulation may be familiar to a small joint arthroscopist, but the change in working distance and instrument excursion from 4 to 30 cm demands its own learning curve. Indications Many deformity patients, especially adults, are primarily concerned with aesthetic issues and elect to undergo surgery expecting a significant correction of their spinal deformity. Anterior spinal release, either open or endoscopic, is therefore indicated for curves with less than 50% correction on bending films, curves greater than 60 degrees in magnitude, and curves that require rebalancing into the stable zone in the coronal or sagittal plane. The contraindications to endoscopic anterior release include any preexisting lung parenchymal pathology, previous thoracotomy, previous empyema or pleurodesis, inability to tolerate singlelung ventilation, and a thoracic scoliotic curve greater than 75 degrees (i.e., in curves greater than 75 degrees, the chest cavity on the concave side and the rib interspaces are too small to accommodate the 10 mm diameter endoscopic portals and instruments). A further relative contraindication is a narrow anteroposterior chest diameter or significant vertebral rotation at the apex. These anatomic variants limit the working space in the chest cavity, and the rotation in particular may cause the mediastinal organs to obstruct exposure. These variables may be overcome by adding more working portals, but under these circumstances, it may be prudent to use a formal open thoracotomy. FIGURE 16–1 Operating room setup for prone position kyphosis correction. Surgical Technique In preparation for a prone position endoscopic exposure, the patient undergoes selective doublelumen endotracheal intubation. The patient is then positioned prone on a radiolucent spinal frame (Figs. 16–1, 16–2, 16–3). The function of the double-lumen tube is first checked in the supine position, then once again in the prone position. The patient must be continuously monitored throughout the case. The back is prepared and draped widely, extending beyond the anterior axillary line on each side. The spine is first exposed through a posterior midline incision to the tips of the transverse processes over the appropriate fusion levels. The appropriate lung is then deflated by clamping the lumen of the double-lumen tube. While waiting for the lung to deflate, bone graft can be harvested from the posterior iliac crest through a separate incision. FIGURE 16–2 Operating room setup for prone position scoliosis correction. FIGURE 16–3 Operating room setup: patient positioned prone, posterior wound open, instruments in chest, simultaneous approach. For scoliosis correction, the spine can be exposed on the convexity or the concavity, depending on the clinical circumstances and the surgeon’s preference. Release on the convexity may require more portals to gain parallel access to each disk space. In some curves, to release the structural tether, it may be difficult to gain access to the posterolateral corner on the concavity at the proximal and distal levels; however, if thoracoplasty is indicated, then only the convex approach is applicable. Working on the concavity, however, allows for fewer portals and provides direct access to the structural tether (posterolateral corner and costotransverse ligaments) over the entire curve. This concave approach does require more meticulous dissection of the aorta, which unfolds into the concavity of the curve. A theoretical vascular risk exists depending on which approach is selected. The aorta is a thick, resilient structure, less prone to injury, in contrast to the azygous system, with its large friable, tortuous veins that may prove more problematic. For scoliosis cases, the first portal is created opposite the apex of the curve at the midaxillary line. For kyphosis correction, the spine can be approached from either chest at the surgeon’s discretion. In these kyphosis cases, the first portal is created opposite the apex of the kyphosis at the midaxillary line. The first portal becomes the main working portal and is the only portal inserted blindly. It is inserted after blunt dissection with a Kelly forceps just over the top of the rib to avoid damage to the neurovascular bundle or deep structures. The 30-degree endoscope is then inserted and the chest cavity is explored. Two further working portals are created under direct video visualization at the posterior axillary line two interspaces cephalad and caudad to the endoscope portal. The remaining portals are inserted under direct view, with the lung protected. The pattern of portal placement can be either an L or V shape, depending on the chest wall morphology and the level of the spine to be approached (Fig. 16–4). The instruments and scope are interchanged between the portals to facilitate work at different levels. A fourth optional portal, two interspaces cephalad at the midaxillary line, can be used if necessary as a suction portal. FIGURE 16–4 Portal placement: “V” shaped portal distribution with additioonal axillary portal. With the patient prone, the deflated lung and mediastinal structures fall out of view, requiring no retraction (Figs. 16–5A, 16–6B). The spinal levels are identified clinically by counting ribs and are confirmed with an anteroposterior radiograph. Multiple individual transverse pleural incisions are made directly over the disk spaces to be released (Figs. 16–5B, 16–6B). The segmental vessels are preserved, and the sympathetic chain is bluntly dissected out of harm’s way. The anterior longitudinal ligament and anulus are incised with cautery. The nucleus pulposus is evacuated with rongeurs and curettes down to the bleeding subchondral bone end plates. For scoliosis cases, the posterolateral corner, costotransverse ligaments, and rib heads on the concave side are released under direct view to obtain optimal correction (Figs. 16–6C). The convex anulus, however, is left intact to act as a tether to prevent overdistraction and as a pivot point during the posterior correction. For kyphosis cases, the entire anulus is released. With transpedicular instrumentation in place, the disk spaces can be levered open to visualize the posterior longitudinal ligament to ensure complete evacuation of disk material (Figs. 16–6C). During scoliosis cases, the aorta is mobilized with blunt dissection (16–6A,B). It frequently lies in the acute angle between the rib head and the lateral vertebral body. Once mobilized, the aorta is protected during the preparation of the disk space with a small sponge and peanut retractor placed in the interval between the vertebral body and the aorta. Bone graft, either structural tricortical crest or femoral allograft ring in kyphosis cases, or morcellized cancellous iliac crest graft in scoliosis cases, is inserted into the disk spaces with the bone holders or an extra long funnel. The endoscope is removed from the chest, and the portals are closed with a subcutaneous and running subcuticular stitch. A chest tube is inserted through the most convenient portal. Timing the implantation of the posterior instrumentation and obtaining the correction are case specific. For cases of thoracic hyperkyphosis, it is typically easier and advantageous to expose the spine across the proposed levels through the posterior incision first, apply the implants, then enter the chest endoscopically to perform the releases. This allows the operating team to take advantage of the segmental instrumentation to lever open each level one at a time for complete and safe diskectomy. For cases of rigid scoliosis, performing the releases first and assessing segmental mobility may avoid disappointment if the releases are inadequate or the anatomy is not ideal. Doing the releases first allows the case to be converted more easily to a lateral thoracotomy by repositioning the patient before the posterior wound is opened. Complications The major concern of this endoscopic prone approach is unrecognized injury to the spinal cord, lungs, mediastinal organs, or major blood vessels. With good endoscopic technique, each disk space is directly visualized, and the evacuation of the nucleus is performed under direct view. The lungs and mediastinal organs are also in full view and with the prone position fall out of harm’s way, eliminating the need for any retraction and minimizing iatrogenic injuries. Other minor concerns include intercostal neuralgias, infection, and wound breakdown. To minimize the risk of intercostal neuralgias, the portals are created under direct visualization from within the chest cavity, in a predetermined trajectory, with blunt dissection over the top of the appropriate rib. To date, there have been no major complications associated with the prone position endoscopic approach in more than 80 cases. Postoperative Care The postoperative care for these patients is identical to any anteroposterior deformity correction case. The patient is typically monitored in an intensive care or step-down setting for the first 24 hours. A chest tube is in place, with the drainage monitored and daily chest x-rays performed. Drainage is typically scant, but if significant, once the drainage is less than 100 ml per shift, the tube is removed. The patient is encouraged to be out of bed the first morning after surgery, and chest physical therapy and incentive spirometry are initiated. The endoscopic portal incisions are inspected daily, and dressings are changed as necessary. FIGURE 16–5 Endoscopic views of kyphosis correction. (A) Initial view, mediastinal organs fall out of harm’s way. (B) Transverse pleural incisions and diskectomy. (C) Release circumferential to posterior longitudinal ligament. Outcomes Many reports of transthoracic endoscopic techniques have now been published. Overall, the results have been predictable and satisfying for both surgeons and patients. The reported complication rate seems to be equivalent to similar traditional open procedures. The advantages of the endoscopic techniques in postoperative pain relief and preservation of pulmonary function have been realized. The operative time associated with the endoscopic procedure was initially reported as longer, yet as surgeons gained experience, the operative time has improved considerably. It now takes experienced endoscopic spinal surgeons ~20 minutes to place portals and expose the spine, and 10 to 15 minutes to release and bone graft each disk space. Comparisons of the extent of spinal correction in adult deformity to historical cohorts match or exceed the published curve corrections, and published animal studies conclude that the extent of diskectomy and quality of release are comparable to open techniques. The obvious advantage of the endoscopic exposure is the cosmetically appealing incisions and easier recovery for patients (Fig. 16–7). Another advantage is the time saved associated with opening and closing a thoracotomy incision. The transthoracic prone position endoscopic approach as described here allows the surgeon the added opportunity to address anterior and posterior spinal pathology simultaneously. Time and cost will be saved by eliminating the need to reprep and redrape during staged procedures. This technique can be used for other anteroposterior tumor or trauma spinal reconstructions. FIGURE 16–6 Endoscopic views of scoliosis correction. (A) Initial view of aorta unfolded into rib vertebra junction. (B) Longitudinal pleural incision. Preservation of segmental vessels. (C) Resection of annulus and evacuation of nucleus pulposus. Case IIlustration The following case exemplifies the benefits of a simultaneous posterior open, anterior endoscopic approach, which allowed for safe and expeditious access to the concavity of a progressive scoliotic curve in a revision situation, obviating the need for a staged procedure or approaching the curve through the previously scarred right thoracic cavity. This 13-year-old female presented with a progressive scoliosis (Fig. 16–8A) and underwent a posterior instrumentation and fusion (Fig. 16–8B). Within 4 months the curve progressed above the fusion (Fig. 16–8C), and she subsequently underwent a right-sided thoracoplasty. The thoracoplasty further exacerbated the curve progression, resulting in a rigid and unsightly deformity. The treatment options now included a staged procedure with further surgery through the previously operated areas or a simultaneous procedure with an endoscopic transthoracic approach from the left chest (concavity of the curve) to release the rigid curve at the same time as the posterior wound is reopened for revision and extension of the instrumentation. During this procedure the left arm was draped free to allow mobilization of the scapula and placement of high axillary ports (Fig. 16–8D,E).The left chest was virgin territory free of scarring, allowing the exposure of the respective levels to be released and bone grafted (Fig. 16–8F,G). The final correction was dramatic (Fig. 16-8H), and the entire procedure was successfully completed in one surgical setting. Conclusion Thoracoscopic combined anterior release and posterior instrumentation can be safely and effectively performed in the prone position, obviating the need for staged procedures in deformity correction in select patients. It avoids the risks and morbidity associated with staged procedures. Like most endoscopic techniques, it has a learning curve and requires familiarity of the thoracoscopic anatomy in the prone position. FIGURE 16–7 Correction and cosmetic result. (A) Preoperative photo. (B) Postoperative photo. (C) Close-up of scars of incisions used for endoscopic access. FIGURE 16–8 13-year-old female presented with progressive scoliosis. (A) Preoperative x-ray. She underwent a posterior instrumentation and fusion. (B) Postoperative x-ray. Within 4 months the curve progressed. (C) Postthoracoplasty progression. She underwent a combined prone position thoracoscopic anterior release and posterior instrumentation. (D) Intraoperative setup. (E) Intraoperative technique. (F) Intraoperative view of prone approach to concave side. (G) Intraoperative view of disk excision for release. (H) X-ray showing the final correction.
16

Combined Prone Position Thoracoscopic Anterior Release and Posterior Instrumentation for Deformity Surgery


< div class='tao-gold-member'>
Combined Prone Position Thoracoscopic Anterior Release and Posterior Instrumentation for Deformity Surgery
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








