FIGURE 56.1 CRPS I of Upper Extremity. Patient had minor injury to right hand following a fall. Edema and erythema are evident along with allodynia, hyperalgesia, and decreased range of motion of hand. Patient failed to get significant relief from medication and stellate ganglion block. A spinal cord stimulator was placed for patient. The results of stimulation are presented in Video 56.1. (See color plates.)![]()
DIAGNOSIS OF COMPLEX REGIONAL PAIN SYNDROME
A. IASP diagnostic criteria.
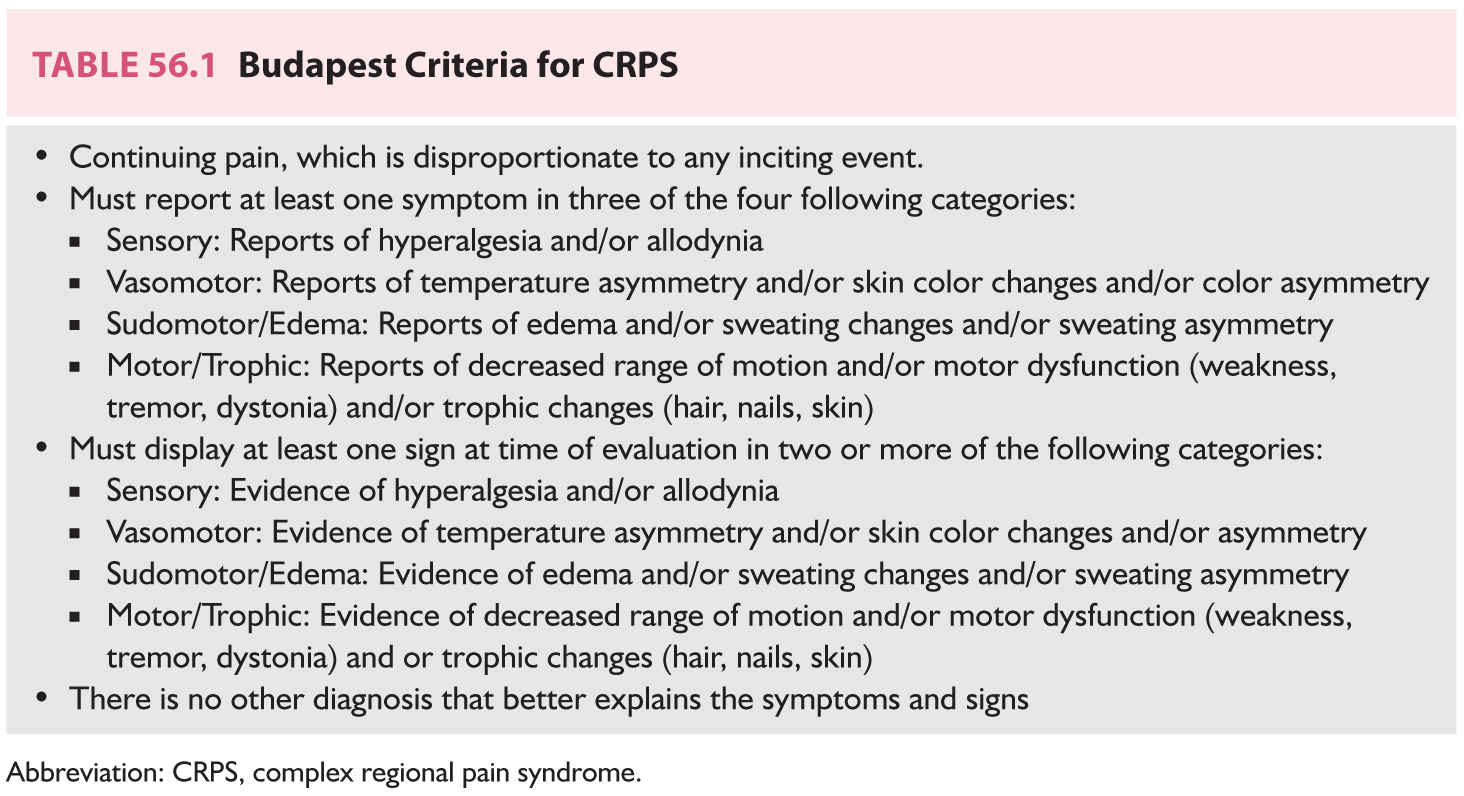
The diagnosis of CRPS as adopted by the IASP in 2012 is based upon a set of criteria known as the Budapest Criteria. They are presented in Table 56.1. The criteria list symptoms and signs in the following categories: sensory, vasomotor, sudomotor, and motor. At least one symptom in three of four of these categories and one sign in two categories must be present for the CRPS diagnosis. Pain must be chronic and disproportionate to any inciting event. No other diagnosis should better explain the symptoms and signs. In research settings, in order to maximize specificity, all four of the symptom categories and two of the sign categories must be present for a positive diagnosis.
B. Differential diagnosis.
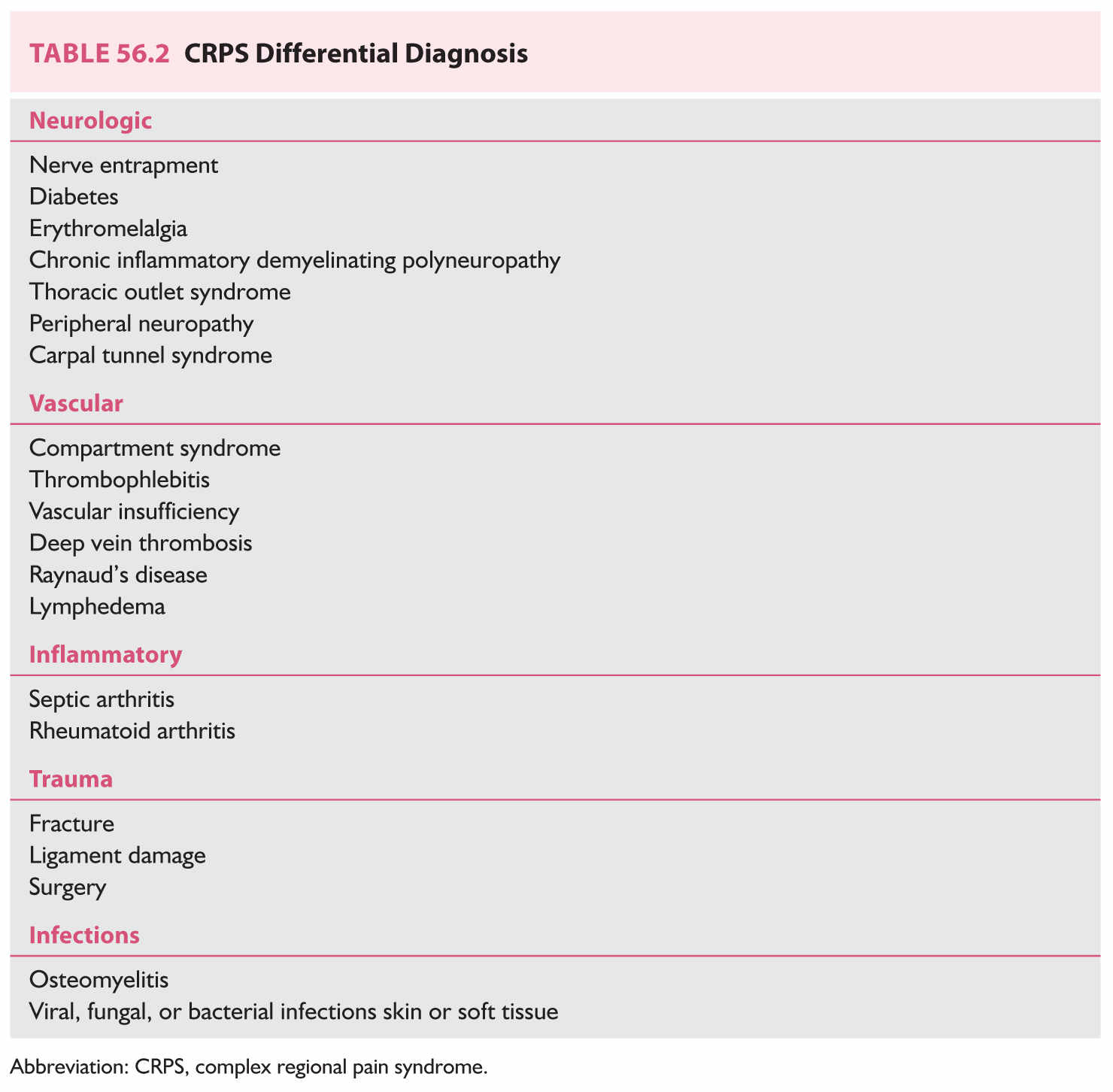
At least some of the symptoms and signs of CRPS can present in a variety of other conditions. Therefore, the differential diagnosis can be somewhat extensive. Conditions with features of CRPS can include neuropathies, vascular disorders, inflammatory disorders, infection, and trauma. A differential diagnosis list is presented in Table 56.2.
C. Diagnostic tests.
A standardized test for CRPS does not exist. The diagnosis of CRPS is based on history and clinical findings. The use of tests is often done to exclude other diagnoses. Both imaging tests and tests of sympathetic nervous system activity are employed typically comparing the affected to the unaffected limb.
1. Imaging techniques.
a. Plain film radiography.
Plain film radiographs are performed on the affected distal extremity. Some of the features on plain radiograph suspicious for a diagnosis of CRPS include soft tissue swelling, osteopenia, cortical bone resorption, and articular erosion. Plain radiography is also useful in identifying or ruling out other bone diseases (e.g., Paget’s disease).
b. Triple-phase bone scan.
Bone scintigraphy is a nuclear imaging test that helps diagnose and follow several types of bone disease. It typically uses a technetium 99 m tracer and gamma counter. It can be used to detect a number of bone-related conditions including malignant lesions, infection (osteomyelitis), arthritis, fractures not evident on plain film, and potentially metabolic bone diseases (e.g., Paget’s disease, osteomalacia).
The triple-phase bone scan is more useful in CRPS diagnosis than plain film radiography. The scan has three phases: (1) Phase 1 (Blood flow)—images are obtained immediately after imaging and demonstrate the perfusion to a region; (2) Phase 2 (Blood pool)—images are obtained 1 to 5 minutes after injection and demonstrate relative vascularity of the region; (3) Phase 3 (Bone scan)—images are obtained 1.5 to 4 hours after injection and reflect tracer uptake within bone demonstrating relative bone turnover. The third phase has been shown to be the most reliable phase for supporting a diagnosis of CRPS. The images consistent with a diagnosis of CRPS are characterized by diffusely increased periarticular uptake to joints of the affected extremity.
2. Sympathetic function tests.
Clinical features of CRPS I can include sympathetic nervous system dysfunction. Changes in both vasomotor and sudomotor activity can occur in the affected extremity.
a. Sympathetic block.
A diagnostic/therapeutic block of the stellate ganglion (upper extremity CRPS) or lumbar sympathetic nerve block (lower extremity CRPS) can be performed with local anesthetic to assess the involvement of the sympathetic nervous system. An increase of skin temperature of 1 to 1.5°C is generally considered to be evidence of a successful block when associated with relief of pain.
b. Thermal testing.
Temperature in the affected and nonaffected extremity in CRPS can be assessed by placing temperature sensors on the surface of both extremities. More detailed assessment of temperature can be done with infrared thermography. Early acute CRPS I often presents as a warm, red, edematous extremity, whereas chronic CRPS more often presents as a cold, mottled, and sweaty extremity.
c. Quantitative sudomotor axon testing.
QSART is a test to assess postganglionic sympathetic cholinergic function by evaluating resting and stimulated sweat production. Increased sweat production in the affected extremity is consistent with a CRPS I diagnosis.
3. Nerve function.
Electromyography and nerve conduction velocity studies can also be considered in order to rule out some neuropathies (see Table 56.2) from CRPS I. However, these studies may be difficult to obtain given the degree of pain some CRPS I patients have in the affected extremity.
EPIDEMIOLOGY
A. Occurrence.
The incidence and prevalence of CRPS are not well established. A large population-based study in the United States showed an incidence of 5.5/100,000 and a prevalence of 21/100,000 for CRPS I. In the same study CRPS II had an incidence of 0.8/100,000 and a prevalence of 4/100,000.
B. Gender, age, race.
The incidence of CRPS I is three to four times more common in women compared to men. CRPS can occur at any age. However, it is less likely to occur in the pediatric population. It is more likely to occur in adolescence than in younger patients. Again, there is a female predominance. The highest incidence of CRPS I occurs between 40 and 70 years of age with a peak in the 40- to 50-year age group. It has been suggested that CRPS in adults and children is more common in Caucasian populations. However, there is insufficient data on which to make a definitive conclusion. CRPS appears to affect all races.
C. Location.
In adults with CRPS I the upper extremity (60%) is typically more often affected than the lower extremity (40%) with equal involvement of left and right sides of the body. In pediatric CRPS I a lower extremity (80%) is more commonly involved again with typically equal left and right sides of the body.
D. Common causes.
In the general population the most common precipitating events for CRPS I include fractures (45%), sprains (18%), and surgery (12%).
PATHOPHYSIOLOGY
Several mechanisms involving both the peripheral and central nervous systems (CNS) have been proposed in the development of CRPS. The syndrome is likely caused by the interaction of several mechanisms rather than a single one. However, it is not clear how and in what proportion these various mechanisms interact to produce CRPS.
A. Inflammation.
Several of the classic inflammatory signs occur in CRPS including pain, edema, erythema, and warmth. These findings are especially evident in early acute CRPS. This acute phase of CRPS has sometimes been identified as “warm CRPS.” Chronic CRPS is more often associated with a cold, mottled, and sweaty extremity. This has been sometimes identified as “cold CRPS.” Both classic inflammatory mechanisms as well as neurogenic inflammation likely contribute to the clinical features in an extremity affected by CRPS. Inflammatory mediators (e.g., cytokines, tumor necrosis factor) as well as proinflammatory neuropeptides (e.g., substance P, calcitonin gene-related peptide) have been found to be present at elevated levels in the affected extremity of patients with CRPS. These substances are involved in the processes leading to vasodilation and protein extravasation resulting in a warm, red, edematous extremity.
B. Immune mechanisms.
Immune mechanisms have also been proposed as being involved in CRPS. An elevation of proinflammatory monocytes as well as mast cells has been seen in patients with CRPS I. It has been suggested that an autoimmune process may contribute to CRPS.
C. Peripheral and central sensitization.
Peripheral and central sensitization are likely both involved in the pathology of CRPS. This is evidenced by the presence of spontaneous pain, allodynia, and hyperalgesia in the CRPS-affected extremity.
Changes in the sensitivity of peripheral nociceptors occur as a result of the effects of proinflammatory mediators. The actions of these mediators result in an increase in firing of the nociceptors at lower thresholds—a process known as peripheral sensitization. This results in primary hyperalgesia.
Changes in the CNS are also evident in CRPS. Central sensitization occurs in the dorsal horn of the spinal cord. N-methyl-d-aspartate receptor mechanisms appear to be involved in this process. Microglia in the spinal cord may also be involved in central sensitization. The net effect is an increased throughput of nociceptive signals likely involved in the chronicity of the CRPS pain state. Central sensitization is directly involved in secondary hyperalgesia.
D. Sympathetic nervous system.
Alterations in sympathetic nervous system function can also be seen after injury in CRPS. This is evident by occurrence of changes in skin temperature, skin color, and sweating in the extremity affected by CRPS.
The type of autonomic dysfunction likely depends on the time frame of the disease. Acute “warm CRPS” more likely involves sympathetic nervous system inhibition with resultant erythema and warmth (vasodilation) in the affected limb. As the syndrome becomes more chronic (“cold CRPS”), sympathetic nervous system hyperactivity may become more evident, manifesting in vasoconstriction and a cold, mottled appearance and sweaty extremity. It has been demonstrated in CRPS that there are newly expressed catecholamine receptors on nociceptive nerve fibers. Therefore, an increase in sympathetic nervous system activity or in circulating catecholamines can result in an increased firing of nociceptive neurons. This phenomenon is known as sympatho-afferent coupling. Activation of these receptors would be expected to increase pain.
E. CNS changes.
CNS changes also play an important role in CRPS. Both alterations in CNS function and structure appear to be present in CRPS. Imaging and functional studies (e.g., functional magnetic resonance imaging) have identified changes in brain regions including primary and secondary somatosensory cortex, motor cortex, and the insula and cingulate cortex. Thus, alterations in cortical function and structure likely contribute to the CRPS presentation, in particular, the motor and sensory deficits seen in the CRPS patient.
F. Psychological changes.
As has been done with other chronic pain disorders it has been questioned that patients with CRPS have certain psychological issues. This has not been demonstrated to be the case. Depression as in the chronic pain population is common in CRPS (25% to 50%). A greater degree of anxiety in response to injury or surgery has been identified as a factor contributing to patients more likely to develop and have a poorer outcome with CRPS.
CLINICAL PRESENTATION AND COURSE
A. Precipitating events.
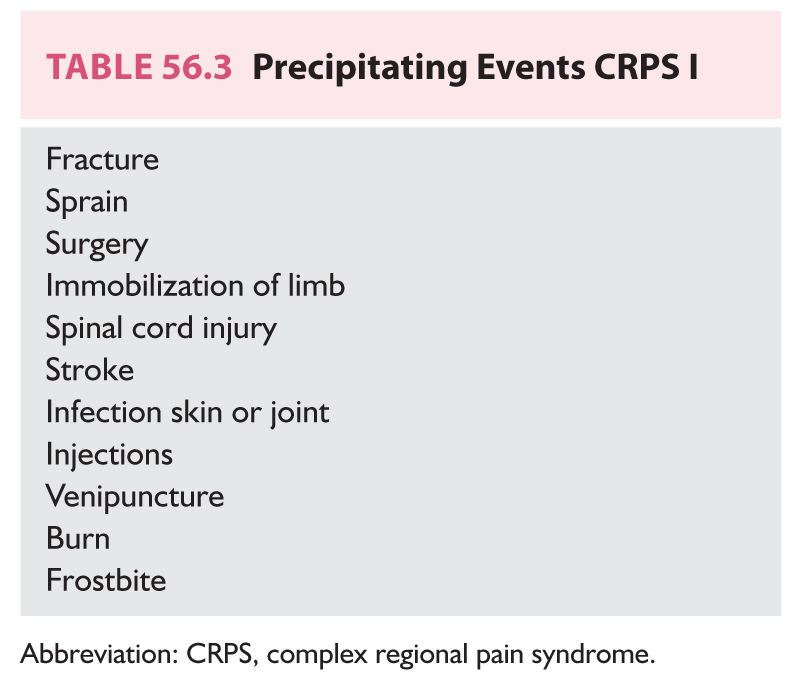
CRPS presents with a triad of sensory, autonomic, and motor disturbances. CRPS I typically presents after tissue injury. Most commonly it presents after fracture (e.g., wrist, ankle) or sprain. However, there are other potential precipitating events (Table 56.3). About 10% of patients do not recall a specific event. CRPS II is associated with an identifiable nerve injury. This could be from trauma (e.g., brachial plexus avulsion) or surgery (e.g., carpal tunnel).
B. Sensory changes.
CRPS is characterized by pain disproportionate in intensity and/or duration to what would be expected with the initial injury. The pain is not in an area typically associated with a single dermatome. Spontaneous pain accompanied by allodynia and hyperalgesia is present. The pain is typically characterized as burning and tingling but has also been described as a deep, dull aching pain.
C. Autonomic/trophic changes.
Initially, patients with CRPS present with a warm, erythematous and edematous extremity. This acute presentation often develops into a chronic presentation characterized by a cold, mottled extremity. Sudomotor changes can also occur evidenced typically by hyperhidrosis and accompanied by trophic changes. The trophic changes can include thin, shiny skin as well as changes in hair distribution, loss more common than gain. Atrophy of muscle and bone loss (osteopenia) can also be present.
D. Motor changes.
A majority of patients with CRPS will develop motor changes. Most commonly this will manifest as extremity weakness. Tremor, myoclonus, and dystonia have also been described.
E. Spread of CRPS.
CRPS may spread from the originally affected limb. Proximal spread in the affected limb is not uncommon. It can also spread to other extremities. Spread from one upper extremity to the contralateral extremity is more common than spread to an ipsilateral lower extremity. All four limbs may be affected.
F. Stages in Presentation of CRPS.
It is generally accepted that there are at least two identifiable presentations of CRPS—acute, so called “warm CRPS” and chronic so called “cold CRPS.” There can be considerable overlap in these presentations. The acute phase of CRPS is evidenced by a warm, erythematous, edematous extremity with spontaneous pain as well as allodynia and hyperalgesia. Chronic CRPS manifests as an extremity that is cold, mottled, and sweaty. Spontaneous pain, allodynia, and hyperalgesia can be present but often to a lesser degree than acute CRPS. Trophic changes and motor dysfunction are also present in CRPS. These features may be more prominent in chronic CRPS. There is no clear time course for either stage. However, the inflammatory changes characteristic of acute CRPS have been shown to be significantly diminished in treated patients with CRPS at 1 year.
Classically, CRPS I has been divided into three sequential stages or phases—stage 1 (acute), stage 2 (dystrophic), and stage 3 (atrophic). Stage 1 has been characterized by pain, sensory abnormalities, edema, and sudomotor changes with less motor change. Stage 2 has been characterized by more significant pain and sensory changes as well as trophic and motor changes. Finally, stage 3 has been characterized by a decrease in pain and sensory abnormalities with persisting vasomotor changes (vasoconstriction) and advanced trophic and motor disturbances. It has been proposed that these classic stages are more likely to represent distinct subtypes of CRPS rather than sequential stages of the syndrome.
TREATMENT OPTIONS
CRPS can be a very challenging syndrome to effectively treat. While some data suggest that acute CRPS may resolve with conservative medical treatment, chronic CRPS is a challenging condition that likely requires a multidisciplinary approach that includes medical, interventional, psychological, physical therapy (PT) and occupational therapy (OT) components. Review of the most recent literature regarding treatment modalities for CRPS demonstrates that there is little support from high-quality randomized controlled trials (RCTs) for many of the most accepted treatment strategies. Therefore, until more high-quality studies can be done to support specific treatments, clinicians must rely on collective clinical experience by experts in the field and standards of care. The currently accepted treatment modalities for CRPS are discussed in this section.
A. Pharmacologic therapy.
1. Anti-inflammatory treatments.
Systemic anti-inflammatory medications [nonsteroidal anti-inflammatory drugs (NSAIDs)] are often started as a primary treatment modality in patients with symptoms of CRPS. Many times, anti-inflammatories have been initiated prior to referral to a pain specialist. To date, it has not been possible to gather good data from trials regarding efficacy of NSAIDs because of a wide range of intervention strategies and outcomes. Symptomatic relief reported by patients taking NSAIDs is also variable.
2. Systemic glucocorticoids.
An early trial of oral corticosteroids is often used in the acute phase of CRPS. The rationale is to inhibit the expression of proinflammatory cytokines (e.g., tumor necrosis factor, interleukin 1), production of inflammatory mediators (e.g., prostaglandins), and reduce the expression of neuropeptides in afferent neurons. The goals are to decrease the inflammatory component believed to be part of acute CRPS and to decrease the likelihood of developing peripheral and central sensitization.
There is very low-quality evidence that oral corticosteroids improve CRPS symptoms when compared to placebo. Oral prednisolone has been used for CRPS. Currently accepted dosages are 30 to 40 mg/day of oral prednisolone for 2 weeks followed by a scheduled taper.
3. Anticonvulsants.
Gabapentin, a medication originally designed to treat epilepsy, currently has a wide range of applications in chronic pain conditions. Gabapentin binds with high affinity to the alpha-2-delta subunit of voltage-gated calcium channels in both peripheral and central neurons. It is believed to exert its effect by stabilizing abnormal hyperexcitability in these neurons. One RCT suggests that gabapentin may have a small effect on pain in CRPS, with a somewhat larger effect on sensory deficits.
There is evidence that participants taking gabapentin experience a variety of adverse events more frequently than those taking placebo. It is typically dosed three times daily up to a maximum of 3,600 mg/day. Dosing should be reduced in patients with impaired renal function.
4. Antidepressants.
Antidepressants are another class of medication, which are commonly utilized in chronic pain conditions including CRPS. They have been shown to exert direct effects on neuropathic pain as well as treat frequently encountered comorbid psychiatric conditions including depression and anxiety. There are a wide range of agents within this class of drugs and selection is often empiric.
Amitriptyline, a tricyclic antidepressant, is the prototypical antidepressant agent used to treat chronic pain. Low doses of the medication (10 to 25 mg) are started orally at bedtime as it can cause sedation and may help with concurrent sleep disturbance. Amitriptyline can be slowly titrated to clinical effect. Side effects include sedation, orthostatic hypotension, dry mouth, blurred vision, and urinary retention.
Duloxetine, a serotonin and norepinephrine reuptake inhibitor, is a newer class of antidepressant medication used to treat major depression as well as chronic pain. Duloxetine has also been effective in treating pain and fatigue associated with other pain conditions such as fibromyalgia.
While there are no RCTs to provide data on the efficacy of antidepressants in CRPS specifically, they are frequently used in conjunction with other medications to treat CRPS-related symptoms. Patient response is variable.
Opioids are rarely effective in pain conditions with a large neuropathic component such as CRPS. Opioids are occasionally added short-term if additional pain control is needed to facilitate fuller participation in functional therapies.
6. Sympathetics.
Calcium-channel blockers are occasionally used as part of a medication regimen in patients with CRPS. In particular, they are utilized in cases of CRPS that appear to have more of a component of sympathetic dysregulation. The rationale is that they produce vasodilatory effects, improving blood flow to the affected area. Side effects may include increase in pain symptoms, arterial hypotension, myocardial depression, and cold intolerance.
Clonidine, a centrally acting a2-agonist, can also be used in cases with suspected inappropriate sympathetic activity. It acts by decreasing sympathetic outflow resulting in vasodilation. Clonidine may be administered transdermally over the affected area. It works by inhibiting norepinephrine release from peripheral presynaptic adrenergic terminals, leading to decreases in hyperalgesia in the areas directly below the patch. Less data are available to support the use of systemic clonidine. Side effects more prominently associated with systemic clonidine include sedation, arterial hypotension, and bradycardia.
7. Inhibition of osteoclastic activity.
The efficacy of bisphosphonates in CRPS has been demonstrated in RCTs. Effects on pain, swelling, and mobility are apparent. One agent that is used is alendronate.
B. Interventional therapy.
1. Sympathetic ganglion blocks.
Based on the understanding that CRPS can have a significant component of sympathetic dysregulation as part of its pathophysiology, directed injections targeting sympathetic ganglia are commonly used as an adjunct to medication and PT and OT. Stellate ganglion sympathetic blockade is utilized for patients with CRPS of the upper extremity, and lumbar sympathetic blockade is utilized for CRPS of the lower extremity. If the sympathetic block is helpful, meaning the patient experiences a subjective improvement in pain relief extending longer than the duration of the local anesthetic or has an objective improvement in function of the affected limb, the injections can be repeated at 1- to 2-week intervals. There is no evidence that sympathetic blocks are curative for CRPS. However, they can be effective if they produce a decrease in pain symptoms allowing the patient to participate more fully in PT and OT.
A stellate ganglion block is performed by injecting local anesthetic at the anterior tubercle of C6, also known as Chassaignac’s tubercle. A successful stellate ganglion block is evidenced by an increase in temperature in the affected extremity (≥1 to 1.5°C) along with pain relief. In addition, an ipsilateral Horner’s syndrome and hoarseness due to a transient, recurrent laryngeal nerve palsy may also occur. Other potential complications include respiratory distress secondary to phrenic nerve block, inadvertent vertebral artery injection with seizures, inadvertent epidural or intrathecal injection of local anesthetic resulting in high spinal, osteitis of transverse process or soft tissue infection, pneumothorax, and brachial plexus dysfunction.
A lumbar sympathetic block is performed by targeting the sympathetic ganglia supplying the legs. The target ganglia are located at anterolateral portions of the L2–L4 vertebral bodies. Potential complications include pain or infection at the injection site, epidural or intrathecal injection of local anesthetic, intravascular injection, and trauma to adjacent structures including the kidney and bowel. Again, a successful block is evidenced by an increase in temperature (≥1 to 1.5°C) in the affected extremity with pain relief.
2. Spinal cord stimulation.
If the above-mentioned modalities are ineffective, or if sympathetic blocks are effective for only short amounts of time, it is reasonable to proceed to a trial of spinal cord stimulation (SCS). The principles of SCS are based upon a theory proposed by Patrick Wall, a neurophysiologist and Ronald Melzack, a psychologist, known as the gate-control theory. This theory proposes that second-order neurons at the level of the dorsal horn act as a “gate” through which noxious stimuli from the periphery must pass in order to reach the higher centers of pain perception in the brain. However, if these same nerve fibers simultaneously receive a non-noxious stimulus, this can serve to “close the gate.” Noxious pain signals from the periphery will thus be inhibited from ascending to the brain. SCS functions by creating this non-noxious stimulus that closes the gate. The spinal cord stimulator lead is placed directly into the epidural space during a trial. During the trial, the stimulator is activated in order to achieve coverage over the painful body region. The trial typically lasts 5 to 7 days. If it is successful, the patient can then proceed to implantation of a permanent spinal cord stimulator.
There is evidence to suggest that SCS + physiotherapy is more effective than physiotherapy alone. Additionally, there is evidence that SCS is effective at improving patients’ own perception of overall improvement for up to 2 years.
3. Sympathectomy.
Surgical sympathectomy is a procedure that has been used to treat multiple conditions with sympathetically mediated pain for many years. Some of these syndromes include hyperhydrosis, Raynaud’s, and CRPS. The procedure involves extensive ablation of the thoracic sympathetic ganglia (T1–T6/7) for conditions affecting the upper extremities and the lumbar sympathetic chain (L2–L4) for lower extremity symptoms. Initially, these were done as open surgical procedures. With medical advancements, these procedures can be done endoscopically or via percutaneous neurolysis with radiofrequency or chemical destruction (alcohol or phenol).
Review of available literature revealed a high failure rate (up to 35%), which was attributed to poor patient selection. Other suggested causes of procedure failure include incorrect diagnosis, inadequate resection, reinnervation, and contralateral innervations. In addition to initial failure, there is also concern for post-sympathectomy neuralgia, which can occur 6 months to 2 years after the initial ablation procedure. One study reports a 44% rate of occurrence of this syndrome.
C. Physical and behavioral therapy.
1. PT and OT.
Many of the pharmacologic and procedural interventions described above are used as a means to allow the patient with CRPS to participate more fully in PT and OT. PT and OT continue to be the mainstay of therapy of CRPS in order to restore function and avoid atrophy and contractures in the affected limb. Patient education regarding the extent to which they should participate in PT and OT and the amount of pain control they should have is important. There should be an understanding that with any physical exercise there may be some increase in pain symptoms. However, it is imperative not to undergo inappropriately aggressive PT, which can result in extreme pain, edema, distress, fatigue, and exacerbation of inflammatory and sympathetic symptoms. The therapy should be directed at gradual increases in strength and flexibility of the affected limb. Some experts have also advocated the use of massage to facilitate lymphatic drainage and improve edema. At this time, this is not a strong evidence to suggest that there is an advantage to lymphatic drainage techniques.
Desensitization therapy is a graded approach to helping a patient overcome associated allodynia and hyperesthesia. In this therapy, the affected limb is incrementally exposed to a wide range of sensations including light touch with soft and coarse fabrics and temperature changes achieved by submerging the limb in cool and warm water baths. The goal of the therapy is to retrain the hyperactive nerves in the affected area to begin interpreting and transmitting sensory input in a normalized fashion.
Transcutaneous electrical nerve stimulation (TENS) is a portable device composed of an electrical generator and conducting pads, which can be applied directly to the skin over the area of pain. The unit provides a buzzing sensation of varying intensities and is again based upon the gate theory described in section on SCS. A trial with a TENS unit can be performed during PT sessions. If it is successful in alleviating pain symptoms, the patient may benefit from having a TENS unit at home to use as needed.
In the setting of chronic pain, comorbid conditions such as depression, anxiety, suicidal ideation, and opioid dependence are commonly present. This is certainly true for CRPS, and the help of a trained behavioral specialist is often a helpful adjunct to medications and interventions.
Psychotherapeutic management of CRPS typically involves counseling, whereby a patient is instructed on pain coping strategies. Attempts are made to identify past or current stressors that may be contributing to the patient’s pain perception. Cognitive-behavioral therapy (CBT), including biofeedback, relaxation, and hypnosis, may also be explored. Finally, additional psychiatric diagnoses that may be present should be identified and treated accordingly.
COMPLEX REGIONAL PAIN SYNDROME IN CHILDREN
Currently, the diagnosis of CRPS in patients under the age of 18 is made using the same criteria used to diagnose adults. Regarding demographics in pediatric patients, there appears to be higher incidence of CRPS in girls, and it seems to be more common in Caucasians. There also appears to be a higher incidence of CRPS affecting the lower extremities compared to the upper extremities.
Although there is a commonly held belief among clinicians that CRPS in children is in some way intrinsically different from CRPS in adults, there is not sufficient empiric evidence to support this claim. Initially, this was based on a series of case reports from the 1970s giving the perception that children may have a milder course of the disease or that they respond more favorably to conservative therapy. Consequently, there were suggestions that CRPS was a self-limited disease in children and risks of side effects from various therapies were not warranted. However, a more recent longitudinal study of adult patients diagnosed with CRPS as children found that on long-term follow-up 52% of these patients still experienced pain and 36% had documented recurrence of CRPS.
A commonly accepted viewpoint is that intensive PT may offer complete resolution of CRPS symptoms in children. Therefore, all other treatment modalities should be utilized for the main goal of facilitating a PT regimen. Numerous studies in the past have supported this claim, some of which reported cure rates of greater than 90% with regimens of intensive PT and no injections or medications. Some experts have suggested that children may have a greater willingness to actively participate in PT, which may lead to the perceived higher resolution of symptoms with PT compared to adults. Many pediatric centers also advocate a trial of TENS as part of a multimodality approach to CRPS. There are no prospective RCTs validating any medication regimens in the treatment of pediatric CRPS. Therefore, there is a wide range of clinical practice utilizing various combinations of tricyclic and other antidepressants, anticonvulsants, steroids, NSAIDs, and opioids to facilitate more meaningful participation in PT. Additionally, there are no prospective RCTs directly comparing outcomes in pediatric CRPS with or without sympathetic blocks. Advocacy of their use is variable among clinicians.
Multiple authors have written about psychological aspects of children with CRPS. Some have even suggested that pediatric CRPS is entirely a psychological or psychosomatic disease process. This misconception likely came from the presentation of CRPS, namely, pain, which is out of proportion to the inciting event and pain patterns, which cross multiple dermatomes and areas of innervations by single nerves. Based on multiple studies, the current consensus is that children who are considered “overachievers” or have significant enmeshment with their parents may have a higher incidence of CRPS. However, aside from this, there is no compelling evidence that children with CRPS are psychologically unique compared with other children with chronic pain or adults with CRPS. A pediatric psychologist, who is trained specifically in chronic pain, is an invaluable addition to the multidisciplinary approach to treating CRPS. They are especially helpful in identifying other psychiatric diagnoses or external stressors (i.e., school or academic stressors, bullying, or psychological/physical abuse) that may be creating obstacles for improvement in symptoms. In addition to meeting with the patient as part of a multidisciplinary team approach, a pediatric psychologist also can meet individually with the child to help cultivate pain management techniques such as relaxation, meditation, and CBT.
At this time, there are emerging therapies for CRPS that go beyond the current standard of care. Some of these therapies have already been studied and advocated by other countries around the world.
Free radical scavengers have been proposed for use in the treatment of CRPS. Both intravenous (IV) (mannitol) and topical [50% dimethyl sulfoxide (DMSO)] preparations have been studied. One RCT has shown some improvement in pain and inflammatory signs with application four times daily of 50% DMSO to the affected area. The rationale for this therapy is based on the understanding that there may be episodes of ischemia followed by reperfusion and increased free radical damage to tissues and nerves. Others have also advocated the use of oral Vitamin C and N-acetyl-cysteine for the same purpose.
NMDA receptor antagonists have also been studied and utilized. The prototypical NMDA receptor antagonist, ketamine, has been administered both topically and via a series of daily subanesthetic infusions in patients with refractory CRPS symptoms. Some placebo-controlled studies have demonstrated that this may be useful. Care should be taken with the administration of ketamine. Potential side effects include sympathetic stimulation, increased secretion production, and psychiatric manifestations including disturbing dreams and hallucinations.
When common treatment modalities are not effective, several studies have investigated the initiation of a 5-day IV lidocaine administration with an escalating dose schedule. The rationale for this therapy is based on studies demonstrating upregulation of tetrodotoxin-resistant sodium channels on primary nociceptive afferent fibers and small dorsal root ganglia pain transmission neurons following peripheral nerve injury. IV lidocaine selectively inhibits these channels and, therefore, decreases neural transmission in a use-dependent manner. One study of 49 patients with refractory CRPS demonstrated a significant decrease in pain parameters and other symptoms and signs of CRPS following a 5-day continuous lidocaine infusion. The pain reduction lasted an average of 3 months and was particularly effective for thermal and mechanical allodynia. Careful monitoring for local anesthetic toxicity is necessary, as faster infusion rates and a duration of treatment longer than 5 days have resulted in dizziness, dysphoria, and hypotension.
Other new and emerging modalities include IV immunoglobulin, oral tadalafil, and low-dose naltrexone. Given the wide range of treatments with different mechanisms of action, it is again apparent that CPRS is a very complex condition and often requires a varied multimodality approach to effectively treat it.
CONCLUSION
CRPS is a challenging condition that often requires a multidisciplinary approach that includes medical, interventional, psychological, and PT and OT components. A wide range of pharmacologic approaches is used in practice. Interventional procedures are also often added to these medication regimens. There is little RCT-supported data for any of these pharmacologic and interventional modalities and current standard of care is based upon expert opinion. PT/OT and pain psychology are important adjuncts to this multidisciplinary approach as well.
Key Points
• CRPS is a chronic pain condition characterized by pain out of proportion to the inciting event. Diagnosis based on the Budapest Criteria relies upon clinical findings including sensory (allodynia, hyperalgesia), vasomotor, sudomotor, and trophic changes.
• CRPS is divided into type I and type II. The distinguishing feature is the presence of an identifiable nerve injury in CRPS II.
• CRPS is a diagnosis of exclusion. The differential diagnosis may include vascular disorders, inflammatory disorders, infection, trauma, and surgery.
• Standard diagnostic testing does not exist for CRPS. Imaging such as X-rays and triple-phase bone scan as well as sympathetic testing, nerve testing, and thermal testing can be used to support the diagnosis.
• CRPS I in adults is more common in women and has the highest incidence between ages 40 and 70. CRPS is more common in the upper extremity in adults.
• Common inciting events for CRPS I include fractures, sprains, and surgery.
• The pathophysiology of CRPS is complex and likely multimodal including components of inflammation, immune mechanisms, peripheral and central sensitization, CNS changes, sympathetic dysregulation, and psychological changes.
• Early CRPS presents with a warm, erythematous, and edematous extremity. Chronic CRPS is characterized by a cold, mottled, and sweaty extremity with trophic changes.
• CRPS can spread from one limb to another.
• There is little RCT data to support most pharmacologic treatments for CRPS. Current standards of care are based on expert opinion and on current understanding of CRPS pathophysiology and on medication use in other chronic pain disorders.
• Sympathetic blocks including stellate ganglion block and lumbar sympathetic block can be useful in the diagnosis and treatment of CRPS.
• SCS is a potentially useful treatment modality in patients with CRPS not controlled with medications and sympathetic blocks.
• PT and OT remain cornerstones of therapy for CRPS treatment focusing on range of motion, muscle strength, and desensitization.
• CRPS in children is diagnosed using same criteria as adults. It is more common in females as in adults. Unlike adults, CRPS more commonly affects the lower extremity in children.
• Treatment of CRPS in children utilizes a multidisciplinary approach including pain physician, child psychologist, social worker, and physical therapist. Intensive PT is considered paramount in the treatment of CRPS in children.
• New therapeutic options are being investigated for the treatment of CRPS. These include free radical scavengers, IV immunoglobulin, tadalafil, and low-dose naltrexone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree