Complications related to surgical procedure
Intracranial hemorrhage
Epilepsy
Air embolism
Follett KA
n = 299
2
–
–
Deuschl G
n = 78
3.8
–
–
Kleiner-Fisman G
n = 921
3.9
1.5
–
PahwaR
n = 360
2.9
2.9
–
15.3.2 Risk Factors for Intracranial Hemorrhage
The risk factors for intracranial hemorrhage have been reported to include a previous history of hypertension and older age (Sansur et al 2007; Elias et al. 2009; Ben-Haim et al. 2009). Xiaowu et al. (2011) have indicated that the incidence rate of intracranial hemorrhages increased 2.5 times in patients with hypertension than in other patients.
With respect to surgical methods, patients undergoing stereotactic coagulation had 5.4 times higher incidence rate of hemorrhage than those undergoing DBS (Xiaowu et al. 2011; Terao et al. 2003; Blomstedt and Hariz 2006). When the electrodes penetrate the ventricular wall or pass through a gyrus, the rate of hemorrhagic complications increases (Elias et al. 2009; Ben-Haim et al. 2009; Zrinzo et al. 2011). The usage of microelectrode recording techniques has been shown to increase the hemorrhagic rate (Zrinzo et al. 2011). Limiting the electrode penetration frequency has been shown to decrease the rate (Gorgulho et al. 2005). There have been two different reports on hemorrhagic risks with the use of the simultaneous multi-microelectrode technique (so called Ben-Gun method): one has shown an increase (Park et al. 2011), while the other has reported the same risk of hemorrhage as the single microelectrode technique (Temel et al. 2007).
15.3.3 How to Avoid Hemorrhages
While deciding between treatment with coagulation or DBS, the patient’s risk factors for hemorrhage should be considered. DBS surgery is more beneficial for the patients with risk factors, such as elderly patients or patients with a previous history of hypertension.
The use of gadolinium-enhanced magnetic resonance imaging (MRI) is recommended for surgical navigation and for determining the electrode trajectory from the surface of the cortex to the target sites to prevent injuring any enhanced vessels. Electrode trajectory penetrating ventricular wall should be avoided. It is also recommended that attention is given to maintaining the patient’s blood pressure in the normal range during the operation. The frequency of the use of microelectrode technique in DBS surgery should be minimized.
We experienced six cases of nonsymptomatic intracranial hemorrhages among 308 patients undergoing stereotactic procedures. The sites of the hemorrhages in our cases were divided into two types. One involved deep-seated hemorrhages that occurred in the basal ganglia around the electrode track, and the other involved shallow subcortical hemorrhages, which sometimes occurred around the outer area of the electrode track (Fig. 15.1). The former type of hemorrhage seemed to be caused by damage to the vessels by the electrodes, especially microelectrodes (Fig. 15.1a). The latter type of hemorrhage seemed to be due to venous congestion caused by coagulation of the surface vein of cerebral cortex (Fig. 15.1b). After we recognized that one case of subcortical hemorrhage was caused by the thoughtless coagulation of seemingly minor thin veins, we stopped performing coagulations of any cortical veins in the stereotactic operative procedure.
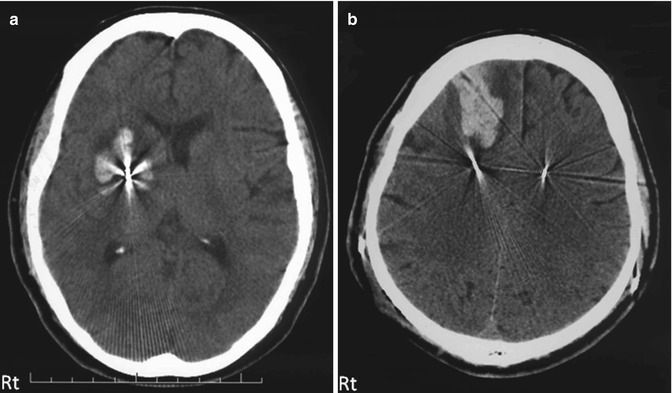
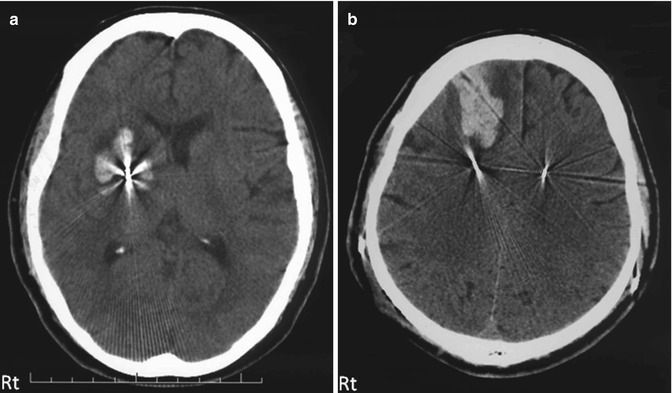
Fig. 15.1
Two different types of intracranial hemorrhagic complications. (a) Deep-seated hemorrhage that occurred in the basal ganglia around the electrode track and that was thought to be due to damage to the vessels by the electrodes, especially the microelectrodes. (b) Shallow subcortical hemorrhage, which sometimes occurred in the outer area of the electrode track. This type of hemorrhage was thought to be due to venous congestion caused by coagulation of the surface veins of the cerebral cortex
We ordinarily use semi-microelectrodes for unit recording as their tips are not as sharply pointed as the tips of microelectrodes. For these procedures, we first use a dull-point catheter to make an electrode root to 10 mm above the target, which is considered the essential area for unit recording. We think that this procedure also reduces the hemorrhagic risk.
15.4 Mechanical Complications
15.4.1 Incidence Rate of Mechanical Complications
The incidence rates that are reported in studies with a large number of and published after 2006 and are related to DBS systems range from 4 to 9.7 %, and these incidences include the mechanical failure of the IPG, pull out or migration of the intracranial electrode, and breakage of the electrodes or extension cords (Seijo et al. 2007; Tabbal et al. 2007; Voges et al. 2007. Boviatsis et al. 2011; Dashti et al. 2008; Fernandez et al. 2011; Hu et al. 2011).
Deuschl et al. (2006) have reported one case (1.3 %) of abnormal DBS stoppage among 78 DBS patients. Follet et al. (2010) have reported an incidence rate of 2 % for malfunctions among 299 DBS patients in their VACSP study, but the reasons for these malfunctions were not reported. Kleiner-Fisman et al. (2006) have reported that 4.4 % of patients underwent reoperations because of malfunctions of the DBS system, infections, or migration of the intracranial electrodes among 921 patients in their meta-analysis study of STN-DBS. Pahwa et al. (2006) have also reported a rate of 2.9 % for electrode migration cases and a rate of 2.0 % for the inappropriate positioning of the electrodes in an AAN review (Table 15.2). That review has also reported that 5 % of 360 cases (18 cases) underwent replacement surgery for the intracranial electrode due to breakage, migration, or inadequate positioning of electrodes, 4.4 % of cases (16 cases) underwent replacement surgery of extension cord, 4.2 % of cases (15 cases) underwent replacement surgery of IPG due to malfunction of IPG, and 0.6 % of cases (2 cases) developed allergic reactions to DBS systems.
Table 15.2
Incidence rate for complications related to DBS machinery trouble or related to wiring
Complications related to DBS machinery trouble or related to wiring | |||
|---|---|---|---|
Infection | Erosion or ulcer of the skin | Malfunction of DBS systems | |
Follett KA n = 299 | 7.7 | – | 2 |
Deuschl G n = 78 | 2.6 | 3.8 | 1.3 |
Kleiner-Fisman G n = 921 | – | – | – |
PahwaR n = 360 | 2.9 | 1 | 4.9 |
15.4.2 Risk Factors of Mechanical Complications
Fernandez et al. (2011) have indicated that the most frequent place for breakage of the electrode or extension cord is the connection area of the intracranial electrode and the extension cord, and there is a tendency for breakage when this part is subjected to a twisting force.
15.4.3 How to Avoid Mechanical Complications
In order to avoid mechanical complications, the wiring, the angles and positions of the intracranial electrodes, the extension cords, and especially the connection of these two cords have to be taken into account. Wiring with sharp angle should be avoided particularly for intracranial electrodes around burr holes or for extension cords around the IPG implantation site. In ordinary patients with involuntary movement, such as Parkinson’s disease, sub-pectoral muscle implantation of the IPG as well as subcutaneous implantation is a preferable method from a cosmetic point of view, and it has an advantage in the prevention of skin erosion or infection of the skin above the IPG. However, sub-pectoral muscle implantation is not preferable for the patients who have a well-developed pectoral major muscle, such as male patients with generalized dystonia. In these patients, strong involuntary contractions of the pectoral muscle can cause stress to the extension wire and subsequently lead to breakage of the wires at the entrance under the pectoral muscle.
15.4.4 Effects of Electromagnetic Fields on DBS Systems
It is required that patients be informed to pay attention to electromagnetic fields in their surroundings or to machines that generate electromagnetic waves in their daily life. According to the Medtronic, Inc. manual of DBS system, it is recommended that cellular phones or radios be kept at least 10 cm away from IPGs. In addition, it is possible that IPGs can be shut off by passing through security gates at the airport or stores and, thus, it is recommended that patients pass through the middle of the gate. It is also recommended that doctors turn down the stimulation voltage of Soletra IPGs to 0 volt and then switch off the Soletra IPGs when they use monopolar electrodes or when computed tomographic scans are performed (Medtronic 2010a).
15.4.5 MRI Measurements After DBS System Implantation
After two MRI-related accident reports, in which one patient developed permanent (Henderson et al. 2005) and the other developed transient neurological deficits (Spiegel et al. 2003), there has been debate about the MRI sequences permissible after DBS implantation. A product company has proposed guidelines for performing MRI on patients with implanted DBS systems, and they have adopted a specific absorption rate (SAR) of less than 0.1 W/kg (Medtronic 2010b). However, several clinical and experimental reports have cast doubts on the adequacy of this SAR value. Baker et al. have reported in their phantom experiments that the linearity between the SAR and temperature increases with MRI measurements differed between MRI machines, and they concluded that the SAR value is an unreliable guideline of MRI safety (Baker et al. 2004). A subcommittee of the Society of Japanese Stereotactic and Functional Neurosurgery conducted a survey on the performance of MRI on patients with DBS implantation in 49 facilities in 2010 in Japan. This survey has revealed that a total of 2,136 MRI procedures that used SAR values above 0.1 W/kg have been performed on patients who had undergone DBS surgeries in these institutions, and no accidents have been reported. Similar to the Japanese survey, Larson et al. (2008) have reported the performance of 1,071 MRI scans on 405 cases with SAR values of 3 W/kg with no accidents. Nazzaro et al. (2010) have reported 1,092 MRI scans that used SAR values above 0.1 W/kg on 249 patients with DBS systems without any accidents. Tagliati et al. (2009) have surveyed 40 institutions comprising 3,304 patients with implanted DBS systems. In their report, all 3,304 patients had undergone at least one MRI, and only one IPG stoppage in one patient was reported. When considering the disadvantages of not conducting MRIs on elderly patients with diseases such as Parkinson’s disease, we strongly hope that these SAR guidelines will be reconsidered and the MRI-tolerable IPG will be developed as soon as possible.
15.5 Infections, Skin Erosions
15.5.1 Incidence Rate of Infection and Skin Erosion
The incidence rate of skin erosion above the DBS system or infection of the DBS system has been reported to range from 2.9 to 7.7 % (Bhatia et al. 2008; Bhatia et al. 2011a; Sillay et al. 2008). Deuschl et al. (2006) have reported two cases (2.6 %) of infection and three cases (3.8 %) of skin erosion around the DBS system among 78 DBS patients. Follet et al. (2010) have reported a rate of 7.7 % of infection around implanted DBS systems among 299 DBS patients in their VACSP study. Pahwa et al. (2006) have reported a rate of infection of 2.9 % (ten cases) after DBS implantation in their AAN review (Table 15.2). Bhatia et al. (2011b) have conducted a meta-analysis of 35 studies published from 1997 to 2009 comprising 3,550 patients and reported an average infection rate of 4.7 %. The most commonly identified pathogen was Staphylococcus aureus, which was found in 62 % (8/13 infected patients among 139 DBS patients) of the cases reported by Gorgulho et al. (2009) and in more than 50 % of the cases reported in the meta-analysis by Bhatia et al (2011a).
15.5.2 Risk Factors for Infections Related to DBS Implantation
Bhatia et al. (2011a) have stated the following specific risk factors in their meta-analysis: (1) frontal subcutaneous connector bulk, (2) straight frontal skin incision, (4) age under 58 years, and (5) age over 65 years. There are two reports on the externalization of electrodes, with one indicating that it is a risk factor of infection (Constantoyannis et al. 2005) and the other reporting that there is no relation to DBS infection (Bhatia et al. 2011a).
15.5.3 How to Avoid the Side Effects of Infections or Skin Erosions
A strategy that avoids infections and skin problems is a matter to consider during all of DBS surgeries, however, it requires much attention to avoid these problems for the patients with ages that fit into the risk factors (age under 58 and over 65), for the patients who have a thin scalp or who have an increased susceptibility to infection, such as patients with diabetes mellitus. Patient management and precautions on handling the DBS device should be made as they are for ventriculo-peritoneal shunt surgery, such as bathing the patients and washing their head and body thoroughly before the operation, not opening the package containing the DBS system until immediately before its use, and avoiding grasping the DBS system with the surgeons’ hand instead of with a surgical instrument. Hockey-stick or crescent incisions, are recommended, instead of linear incisions, which cross over the burr hole, or intracranial electrodes. In addition, placing the stimulating electrodes, extension wires, and connectors under or around the skin incision should be avoided. For patients with very thin scalp, there are several ways worth considering for the placement of the connector. One is to drill out skull to make a space for connector placement, which is actually not easy to do because of the limited exposed area by skin incision for burr-hole surgery. We otherwise recommend that the connectors be placed at patient’s neck area under his jaw where it will be surrounded by loose soft tissue without any underlying bone. It is also recommended that the electrodes and connecting wires be placed as deep as possible, especially under the scalp area.
15.6 Epilepsy and Air Embolisms
15.6.1 Incidence Rate of Epilepsy and Air Embolisms
Epilepsy has also been reported as a complication related to DBS therapy. Its incidence reported in the literature has widely varied from 0 to 13 %. Kleiner-Fisman et al. (2006) have reported that 1.5 % of the patients in their meta-analysis study of STB-DBS developed epilepsy. Pahwa et al. (2006) have also reported that 2.9 % of the patients in their AAN review developed epilepsy (Table 15.1). In their meta-analysis of DBS complications described in 32 reports from 1991 to 2008, Coley et al. (2009) have reported that 2.4 % of patients developed epilepsy among 1,445 patients in 14 out of 16 reports (two of the reports were omitted because of data duplication, and no descriptions of seizures as a complication). A total of 74 % of these seizures occurred around the time of electrode implantation, and many of these patients suffered intracranial hemorrhages. Coley et al. (2009) have also indicated that the risk of seizures associated with the chronic stimulation period is 0.5 %. Chang et al. (2011) have reported that air embolisms occurred in 1.3 % (6 out of 467 cases) of DBS surgeries, but there have been no reports of air embolism complications in the large number case studies (Table 15.1).
15.6.2 Risk Factors of Epilepsy and Air Embolisms
Pouratian et al. (2011) have chosen the following three possible risk factors of seizure complications in an univariate analysis: 1) abnormal postoperative imaging, such as hemorrhages, edema, or ischemia; 2) age over 60; and 3) transventricular electrode trajectories, but only abnormal postoperative imaging was identified as a significant factor in a multivariate analysis. Chang et al. (2011) have reported no statistically significant relationships of air embolisms during surgery with patients’ ages, diagnoses, or DBS targets.
15.6.3 How to Avoid Epilepsy and Air Embolism Complications
As for the risk factors for seizure complications, these causes are merely related to subcortical damage during DBS procedure. It is recommended that procedures be followed that avoid hemorrhagic risks and that the penetrations by electrodes be limited to prevent brain injury and edema.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







