CHAPTER 268 Current Status and Future Direction of Management of Spinal Cord Injury
Spinal cord injury (SCI) costs society in excess of 7 billion dollars annually1,2 and bears the greater cost of human suffering related to impaired ambulation, sensation, and bowel, bladder, and sexual function. Advances in supportive care have significantly improved the survival of patients with SCI in recent years2; however, physicians currently have little else to offer these devastated patients. Fortunately, the last decade has seen tremendous scientific advancement in this field. Several emerging therapeutics are showing promise in early-phase clinical trials, and there is a real possibility that one or more efficacious therapies will soon enter clinical practice. It is thus increasingly important for neurosurgeons and purveyors of emergency and critical care to be familiar with these advances. Other advances such as cell replacement therapy are more distant on the horizon but also have strong potential for translation.
This chapter aims to review current treatments of acute SCI, as well as those that are on the horizon. Supportive and surgical care is reviewed in greater detail elsewhere in this text, as is the treatment of chronic SCI.3,4
Pathophysiology of Spinal Cord Injury and A Basis for Therapeutics
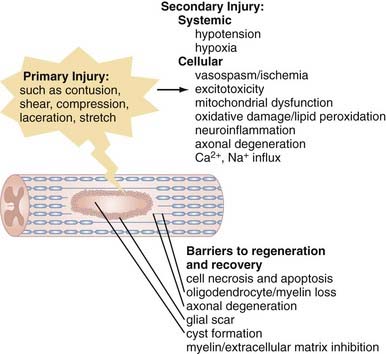
The pathophysiology of SCI can be conceptually divided into two critical phases: the initial primary injury and subsequent secondary injury.5–9 Primary injury refers to the initial traumatic insult to the spinal cord, which results in immediate severing of axons and death of spinal cord cells.10 Secondary injury invariably follows and leads to progressive tissue damage for weeks and even years after the initial insult.11–13 It results from a complex series of interrelated events seen on a number of physiologic levels. Hypotension and hypoxia are important preventable causes of secondary injury at a clinical level and must be recognized and either prevented or treated proactively. Numerous secondary injury mechanisms also occur on the cellular level, and although their delayed time course theoretically provides a window for therapeutic intervention,14 we are currently less capable of arresting these processes, which include vasospasm and localized ischemia,15,16 delayed cell damage and apoptosis,17–19 ion-mediated cell damage and excitotoxicity,13,20 and neuroinflammation,21 as well as mitochondrial dysfunction6 and oxidative cell damage (Fig. 268-1).22,23
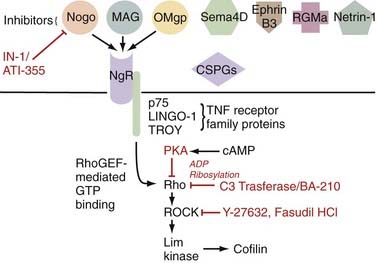
Additionally problematic is the fact that regeneration within the central nervous system (CNS) is poor after an insult.24 Trophic factor levels and the endogenous stem cell response are insufficient after injury.12 Moreover, the myelin normally essential for neuronal function becomes a major inhibitor of axonal growth after injury (Fig. 268-2).25,26 A number of myelin-associated inhibitors of axonal regrowth have been identified, the first being Nogo.27–29 Subsequently identified were myelin-associated glycoprotein and oligodendrocyte-myelin glycoprotein, as well as guidance molecules (semaphorin 4D, ephrin B3, repulsive guidance molecule A, netrin-1) and chondroitin sulfate proteoglycans of the extracellular matrix (NG2, versican, neurocan, brevican, phosphacan), which have the same inhibitory effects.30–33 Of therapeutic significance, all these inhibitors of axonal regeneration appear to signal via activation of the guanosine triphosphatase (GTPase) Rho.34 Glial scarring is also an obstacle in that it is a barrier to neural outgrowth and may promote neuropathic pain.35–37
Although these obstacles are formidable, neural preservation and repair are highly feasible. Only a fraction of spinal cord axons must be intact to facilitate ambulation,38 and residual axons cross the injury even in the face of severe SCI.38,39 Furthermore, many of these axons are viable but dysfunctional only because of oligodendrocyte loss and demyelination.40,41 Agents that improve cell survival, replace lost cells, or enhance function of the surviving neurological substrate even modestly may thus be of great functional significance. Additionally, in a landmark finding, Aguayo and David demonstrated that central neurons have the capacity to regenerate in environments free of the inhibitors typically found in the CNS.42 Therapies that neutralize myelin inhibitors and antagonize Rho are showing great promise in early-phase human clinical trials.43 With this in mind, optimism of both patients and physicians is thus justified.
Current Treatment of Spinal Cord Injury
Spine surgery is a rapidly changing field, and although operative nuances have seen dramatic change even in recent years, the reality is that decompression, realignment, and stabilization remain the primary offerings of the spine surgeon for the acutely spinal cord injured. SCI guidelines44–48 and pharmacotherapy have been more recent important additions to the clinical armamentarium.
Initial Management
The top priority in managing acute SCI is assessment and stabilization of vital signs, with strict adherence to the advanced trauma life support protocol.49,50 After stabilization, patients with SCI should be transferred expeditiously to the nearest trauma center that can provide definitive care.44 During transport, the cervical spine must be immobilized by stabilizing both the body and head44; merely stabilizing the head allows the body and thus the cervical spine to move and risks iatrogenic injury. After transfer it is also imperative to remove a patient from rigid spine boards immediately, preferably within 4 hours of being placed on such a board, to prevent pressure-induced ulceration.50 Initial management should be provided in a critical care unit experienced in intensive neurological monitoring and invasive blood pressure monitoring.
Breathing
Respiratory insufficiency is an important cause of early mortality after SCI. High cervical injuries (C3-5) paralyze the diaphragm and cause respiratory arrest. Lower cervical injuries affect the intercostal muscles, typified by paradoxical breathing. Paralysis of the intercostal musculature is associated with an approximate 70% decrease in forced vital capacity and maximal inspiratory force because inspiration causes chest wall collapse until the onset of spasticity.51 Patients who compensate initially can fatigue rapidly, and indeed, a third of patients with cervical injuries will require intubation in the first 24 hours. It is thus useful to monitor vital capacity in such patients; intubation should be considered in patients whose vital capacity is less than 1 L, particularly if there is evidence of fatigue.51 Hypoxia is an important cause of secondary SCI and must be avoided.
Circulation
Fluid administration is generally considered first-line therapy in this situation52; however, a restricted heart rate makes these patients susceptible to fluid overload.51 Early consideration of vasoactive agents is recommended, in particular an agent such as dopamine with both α- and β-adrenergic activity, to counter peripheral vasodilation, in addition to providing chronotropic support to the heart (Table 268-1).51 It is recommended that mean arterial pressure be maintained higher than 85 mm Hg for the first 7 days after SCI.44,53
TABLE 268-1 Vasoactive Agents for Spinal Cord Injury
| DRUG | DOSE RANGE | MECHANISM OF ACTION |
|---|---|---|
| Dopamine* | 1-10 µg/kg/min | α Agonist at low doses, β agonist at higher doses |
| Dobutamine | 5-15 µg/kg/min | Only β-adrenergic |
| Epinephrine | 1-8 µg/min | α Agonist and β agonist, may promote cardiac dysrhythmia |
| Norepinephrine | 1-20 µg/min | Mainly β-adrenergic, mildly α-adrenergic |
| Phenylephrine | 10-100 µg/min | Only α-adrenergic |
The ideal pressor for spinal cord injury counters peripheral dilation (α-agonists), as well as impaired cardiac chronotropy (β-agonists).
* Dopamine has both properties and is an excellent choice for many patients with spinal cord injury.
Adapted from Ball PA. Critical care of spinal cord injury. Spine. 2001;26:S27-S30.
Clinical Assessment
A number of valid clinical assessment tools have also been devised. The American Spinal Injury Association (ASIA) impairment scale, alternatively known as the International Standard for Neurological Classification of Spinal Cord Injury, was first published in 1982 and now represents the international standard for postinjury evaluation of neurological function.54 Its simplified form, the ASIA impairment scale, bears the same form as the earlier Frankel scale and maintains backward compatibility with it. The modified Benzel classification system, used in the GM1 ganglioside trial,84 may be used in future trials because it addresses some of the perceived deficits of the ASIA impairment scale: it subdivides ASIA D into three different grades to reduce the ceiling effect and additionally assesses walking and sphincter function.
Imaging
When SCI is present, imaging is used to confirm the injury and delineate the anatomy of the lesion. If possible, magnetic resonance imaging (MRI) is optimal and delineates soft tissues involved in the injury. Spinal cord compression is important to note and can be quantified with reproducible techniques.56 Moreover, several MRI parameters, including the degree of cord compression, the severity of spinal cord swelling, and the presence of intraparenchymal hemorrhage, have been shown to predict adverse neurological outcomes after SCI.57 As discussed later, a growing body of evidence suggests benefit from early decompression of the compressed spinal cord, which must then be considered. In the cervical cord, decompression may be performed by either closed or open means.
Spinal Cord Decompression
Closed Reduction
There are a number of contraindications to cervical traction, as outlined in Table 268-2, and great care must be taken in patients with abnormal spinal anatomy, such as those with ankylosing spondylitis, in whom the risk for iatrogenic injury is high. Most studies report a greater than 80% success rate, and about 80% of patients improve neurologically after traction.44 Reports of neurological worsening with traction have raised fear of exacerbating or inducing disk herniation and resulting SCI.58,59 The literature suggests that although the prevalence of disk herniation is high in patients with SCI, its clinical relevance is doubtful.60 Nonetheless, our group prefers to perform MRI before traction in neurologically intact patients who have “everything to lose” but prefer traction as a first step in patients with any SCI. Guidelines pertinent to closed decompression are presented in Table 268-3.
TABLE 268-2 Contraindications to Cervical Traction
TABLE 268-3 Recommendations from the 2002 Acute Spinal Cord Injury Guidelines Pertinent to Closed Reduction; All Recommended as Therapeutic Options
MRI, magnetic resonance imaging.
From Hadley MN, Walters B, Grabb P, et al. Guidelines for the management of acute cervical spine and spinal cord injuries. Clin Neurosurg. 2002;49:407-498.
Timing of Decompression
A significant body of animal research has demonstrated neurological benefit from early decompression of the injured spinal cord; however, such benefit is less clear in humans, particularly in polytrauma patients, who are often medically unstable in the acute postinjury phase.61–63 Despite the fact that early spine surgery appears to be safe in polytrauma patients,61 the question of whether early decompression for acute human SCI is or is not beneficial for neurological recovery remains incompletely answered.61
Decompression of Central Cord Syndrome
Central cord syndrome is uniquely challenging with respect to determining the optimal timing of intervention given that most patients are initially seen without spinal instability and experience substantial spontaneous neurological improvement. In addition, a historic and influential publication from Schneider and associates in 1954, which first described central cord syndrome,64 reported several poor outcomes arising from early decompression. The result was a recommendation to consider central cord syndrome a unique clinical entity and to avoid early procedures because of perceived risk to the spinal cord. Despite the tenuous evidence supporting it, this recommendation has persisted in the literature, although recent evidence challenges this conclusion.65
Even though attempts have been made to identify factors that influence neurological outcome after central cord syndrome65–68 and specifically address whether early surgery is beneficial,69–71 a prospective trial is needed. Fortunately, investigators at the University of Maryland have registered a phase II, single-center randomized clinical trial to examine the timing of decompression in patients with central cord syndrome. This trial seeks to randomize 30 patients to decompression within 5 days or after 6 weeks of injury. The study will compare ASIA, Functional Independence Measure, and Spinal Cord Independence Measure scores; the degree of canal compromise and spinal cord compression; and syrinx size. Patients will be monitored for 1 year.
Venous Thrombosis Prophylaxis
Patients with SCI are at very high risk for venous thromboembolism in light of their tissue injury and venous stasis resulting from paralysis. The acute SCI guidelines recommend a combination of low-molecular-weight heparin, rotating beds, adjusted-dose heparin, pneumatic compression stockings, or electrical stimulation as prophylaxis for deep venous thrombosis.44 Low-dose heparin therapy or oral anticoagulation alone is not recommended as prophylactic treatment, but vena cava filters are recommended for patients who fail anticoagulation or cannot undergo anticoagulation. A 3-month duration of prophylaxis for deep venous thrombosis and pulmonary embolism is recommended.
Guidelines
In recent years, the neurotrauma field has been significantly advanced by the establishment of guidelines. The acute SCI guidelines were published in 2002 and focus on pharmacotherapy, traction, intensive care management, and surgery.44 These guidelines will help standardize management of patients with SCI and will thus play an important role in future SCI clinical trials. Key recommendations from these guidelines have been discussed in the preceding sections.
A parallel effort in establishing guidelines for chronic SCI was published in 2005 by the Consortium for Spinal Cord Medicine, whose clinical practice guidelines deal with rehabilitative aspects of care. These guidelines cover outcome measures, autonomic dysreflexia, respiratory function, thromboembolism, pressure ulcers, bowel function, and depression.72
Pharmacotherapy and Completed Randomized Controlled Trials for Acute Spinal Cord Injury
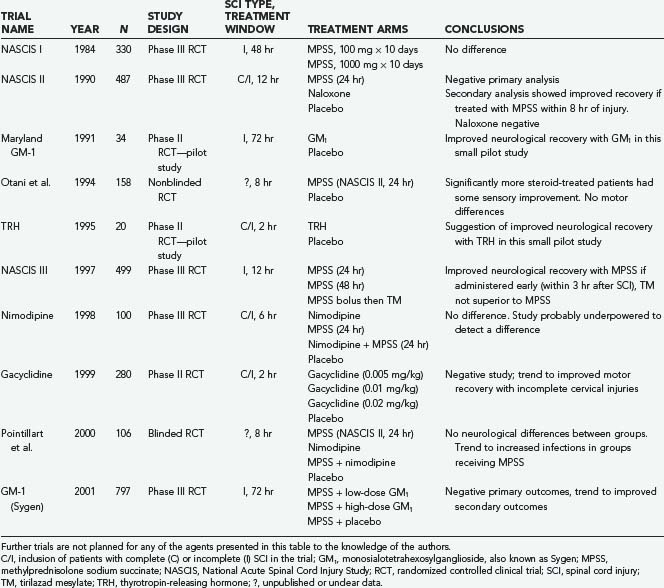
A number of pharmacotherapies have been developed with the aim of ameliorating secondary injury processes; however, only methylprednisolone sodium succinate (MPSS) has found clinical application thus far. Other agents investigated in large multicenter prospective randomized controlled trials include tirilazad mesylate, GM1 ganglioside, thyrotropin-releasing hormone (TRH), gacyclidine, naloxone, and nimodipine (Table 268-4).
Methylprednisolone Sodium Succinate (Solu-Medrol)
Corticosteroids have been used for neurotrauma for decades but have only recently been subject to intensive scientific scrutiny. Their neuroprotective effects include antioxidant properties, enhancement of spinal cord blood flow, reduced calcium influx, reduced axonal dieback, and attenuated lipid peroxidation.23,24 After the accumulation of preclinical data that were generally supportive of a neuroprotective role in animal models of acute SCI,73 MPSS was studied in five prospective human acute SCI trials,74 thus making it the most extensively studied drug for acute SCI.75
Three landmark National Acute Spinal Cord Injury Study (NASCIS) trials examined the use of MPSS for acute SCI. The first NASCIS trial, published in 1984,61 compared high-dose with low-dose MPSS; placebo was judged unethical because benefit from steroids was presumed.75 Neurological improvement was not significantly different in the two groups, although a statistically significant increase in wound infection was noted in the high-dose group, as well as increased rates of gastrointestinal hemorrhage, sepsis, pulmonary embolism, delayed wound healing, and death.62
Animal studies completed subsequent to NASCIS I suggested that higher doses may be required for neuroprotection.63 NASCIS II was thus designed to examine a higher dose of MPSS with comparison to placebo and the opioid antagonist naloxone given within 24 hours of injury.66 In the overall analysis there was no neurological benefit in the MPSS-treated group; however, a post hoc analysis74 (reportedly planned a priori65) found that patients receiving the drug within 8 hours of injury benefited neurologically, notably including those with complete injuries.79 As in NASCIS I, MPSS administration was associated with an increase in wound infection and pulmonary embolism.79
The NASCIS III trial was designed and powered to explore the beneficial effects of MPSS administration within 8 hours of injury reported in NASCIS II.68,69 This was the only NASCIS trial to assess functional outcome; it used the Functional Independence Measure and compared the 24-hour infusion used in NASCIS II with a 48-hour infusion of MPSS and a group receiving tirilazad mesylate, a 21-aminosteroid believed to be an antioxidant without glucocorticoid effects.70 Overall, this trial demonstrated no sustained benefit with MPSS administration. A post hoc analysis noted that patients receiving an MPSS bolus 3 to 8 hours after injury demonstrated improved neurological function at 6 weeks and 6 months but not at 1 year when administered MPSS for 48 rather than 24 hours. This led to the recommendation that within 3 hours of injury, a 24-hour infusion would suffice, but if initiated within 3 to 8 hours of injury, a 48-hour MPSS regimen was better than the 24-hour NASCIS II regimen. The 48-hour regimen represents the highest dose of MPSS prescribed for any clinical condition71 and was associated with a twofold higher rate of severe pneumonia, a fourfold higher rate of severe sepsis, and a sixfold higher incidence of death when compared with the 24-hour group.74
Two other prospective human SCI trials involving corticosteroids have been published. Although Otani and coauthors76 reported benefit from MPSS administration, Pointillart and colleagues77 reported none. Nonetheless, both studies were small and plagued by methodologic problems, which limits their interpretation as either positive or negative studies.
Scrutiny of the aforementioned trials has led to two predominant concerns regarding the use of MPSS for acute SCI.74,78–82 First, the benefits noted have been modest and have come from secondary analyses. Second, high rates of adverse events were consistently associated with MPSS administration. Our personal view is that MPSS administration remains justified for acute SCI (with 8 hours) in nondiabetic and nonimmunocompromised patients given the severity of SCI deficits and current lack of alternatives.83
GM1 Ganglioside (Sygen)
Gangliosides are complex glycolipids abundant in the membranes of nervous tissue. In 1991, exogenous administration of monosialotetrahexosylganglioside, also known as GM1 or Sygen, was examined in the prospective randomized Maryland GM-1 study of 37 patients. This trial demonstrated statistically significant improvement in ASIA motor scores when compared with placebo.84 Efficacy was noted as late as 48 hours after injury, and a predominant effect on lower extremity function suggested effect on axons traversing the injury.75 This led to the largest prospective randomized clinical trial in patients with acute SCI to date, the Sygen Multi-Center Acute Spinal Cord Injury Study, which enrolled more than 750 patients. This study failed to demonstrate a significant difference in its ambitious primary outcome measure—a two-point improvement on the modified Benzel walking scale. It is possible, however, that greater efficacy may have been seen with earlier administration; because the patients were obligated to receive MPSS first, GM1 was not administered, on average, until 55 hours after injury in this study. We are unaware of any plans for future trials with this agent.85
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree