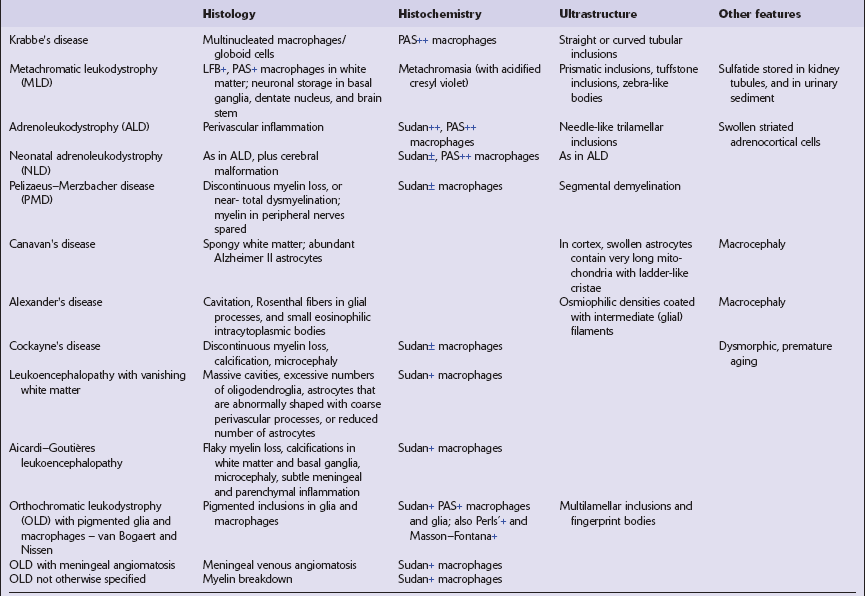
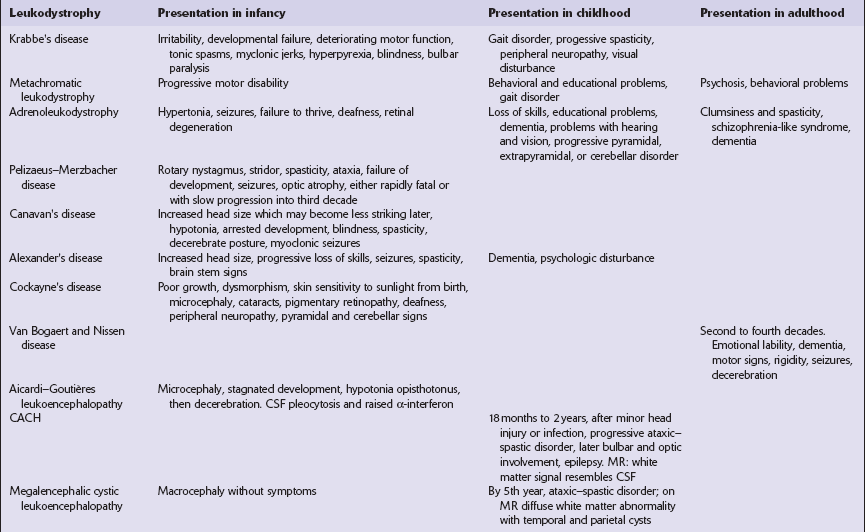
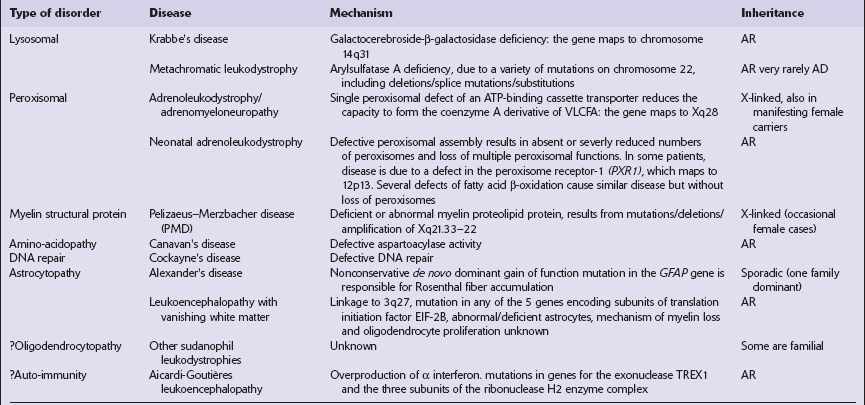
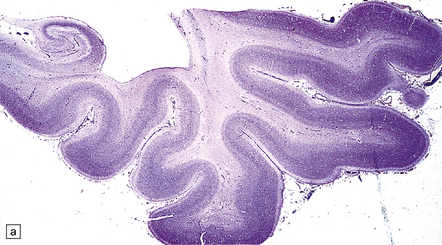
5 The leukodystrophies can be distinguished on the basis of their clinical, etiologic, and neuropathologic characteristics (Fig. 5.1, Tables 5.1–5.3). This chapter covers the leukodystrophies that are not known to be due to lysosomal or peroxisomal disorders. Those that are caused by lysosomal or peroxisomal disorders are described in more detail in Chapter 23. Table 5.1 Clinical features of leukodystrophies CACH, childhood ataxia with central hypomyelination syndrome. Table 5.2 Etiologic classification of leukodystrophies AR, autosomal recessive; AD, autosomal dominant; VLCFA, very long chain fatty acids. 5.1 Descriptive classification of leukodystrophies. unremarkable in the connate cases, but generally appears gray and firm with a blurred gray–white matter interface (see Fig. 5.2a,b). Cerebellar atrophy can be marked. Involvement of brain stem and cord tracts renders them a dull yellow, contrasting with the whiteness of the preserved peripheral myelin in cranial and spinal roots. 5.2 Pelizaeus–Merzbacher disease. Myelin staining may be absent (connate variant) or severely reduced but leaving a flaky or tigroid pattern where residual myelin islets have a tendency to hug blood vessels (Figs 5.2–5.4). Axons are relatively preserved, though oligodendroglia are reduced and astrocytosis is marked. All central myelin is affected, while spinal and cranial nerve roots and peripheral nerves are normal (Fig. 5.5). Sudanophilic lipid is sparse and contained in perivascular macrophages. Cerebellar cortical degeneration is quite common (Fig. 5.6). 5.3 Pelizaeus–Merzbacher disease. 5.4 Myelin and sudanophilic lipid in Pelizaeus–Merzbacher disease. 5.5 Sparing of myelin in peripheral nerves in Pelizaeus–Merzbacher disease.
Disorders that primarily affect white matter
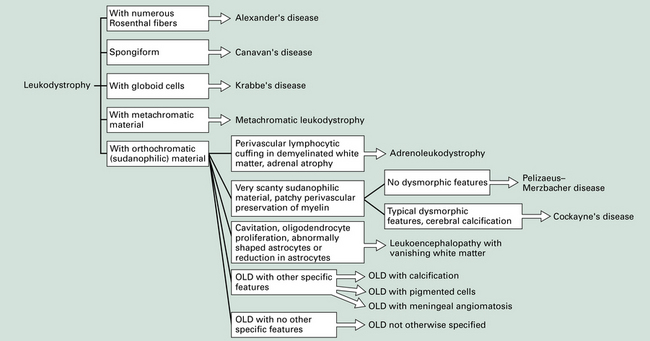
This provides a morphologic approach to the differential diagnosis of the leukodystrophies. OLD, orthochromatic leukodystrophy.
PELIZAEUS–MERZBACHER DISEASE
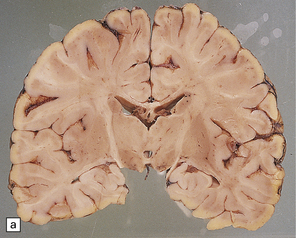
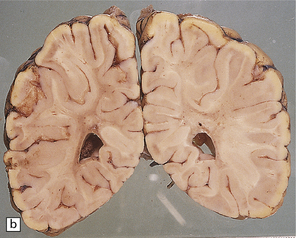
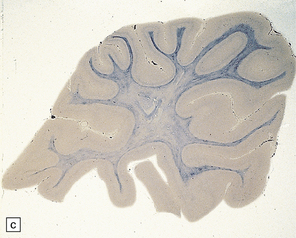
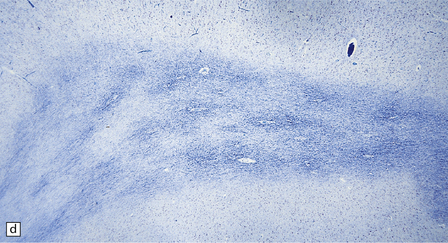
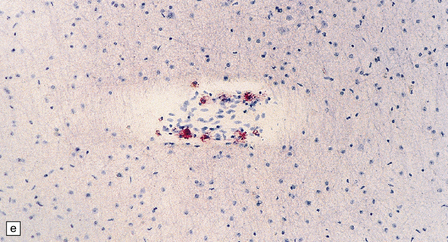
(a,b) Sections of the brain from a 15-year-old male with a typical slowly progressive clinical disorder. Much of the cerebral white matter appears gray and granular, but the U-fibers are relatively spared. The internal capsules and corpus callosum are streaked with gray. (a) Coronal section through the basal ganglia. (b) Coronal section through the parieto-occipital region. (c) In the occipital lobe from this patient there is only scant myelin staining. (d) At higher magnification the white matter takes on a tigroid appearance as islands of residual myelin surround blood vessels. (e) In this frozen section there is only sparse orthochromatic lipid.
MICROSCOPIC APPEARANCES
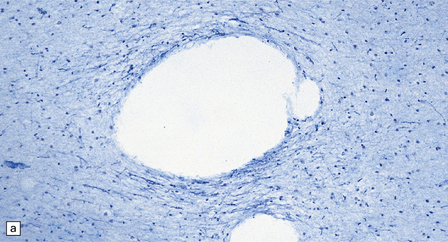
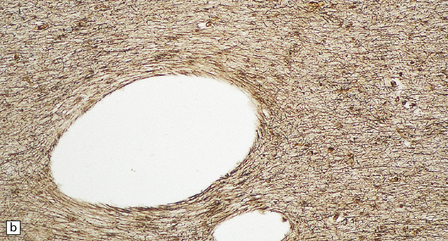
As with other leukodystrophies there is a relatively spared population of axons in demyelinated regions. (a) Occipital white matter stained for myelin. (b) An adjacent serial section stained for axons.
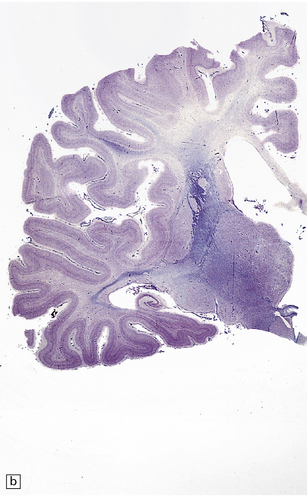
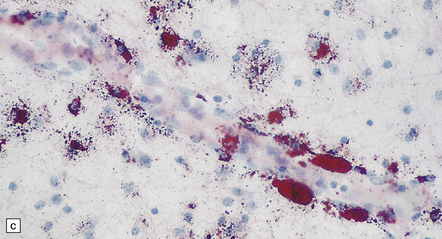
(a,b) Coronal sections from a 6-month-old child with the connate form of Pelizaeus–Merzbacher disease. Myelin is demonstrable in the internal capsule and optic radiation only. (a) Temporal lobe. (b) Coronal section at mid-thalamic level. (c) Moderate amounts of orthochromatic lipid can be demonstrated.

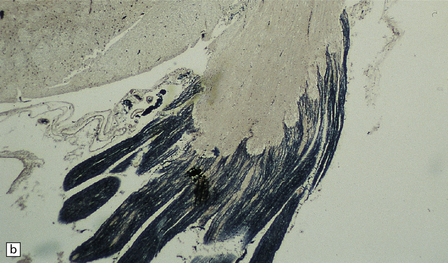
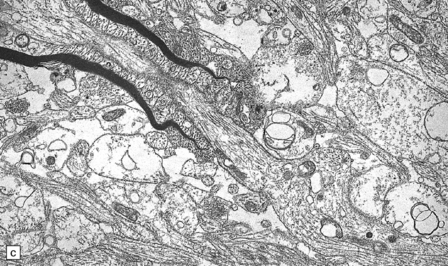
This is a characteristic finding. (a) Anterior aspect of the spinal cord showing the marked contrast between the normal white roots and the gray (demyelinated) cord. (b) Lateral pons showing the fifth cranial nerve root. Compare the normal peripheral myelin with the unmyelinated central structures. (c) Ultrastructural examination of the white matter from a cerebral biopsy showing segmental demyelination. The myelin stops abruptly at a heminode, leaving a naked axon continuing through the neuropil.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Disorders that primarily affect white matter
Only gold members can continue reading. Log In or Register to continue