Chapter 6 Electroencephalographic Artifacts
STRATEGIES OF ARTIFACT RECOGNITION
“Biological Plausibility” Versus “Biological Implausibility”
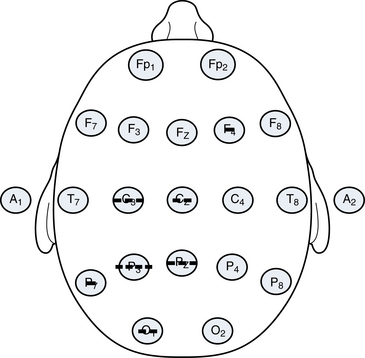
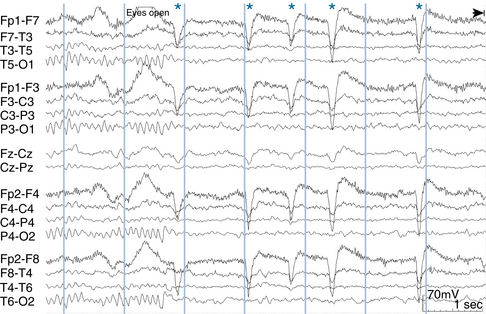
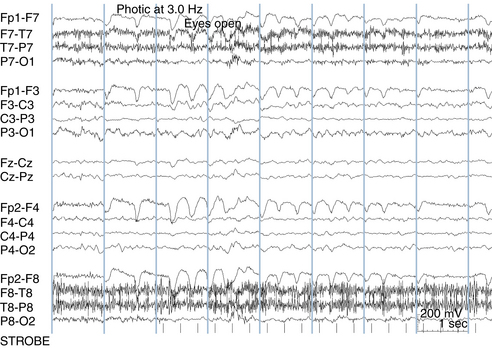
Although some artifacts can be recognized on the basis of the shapes of their waves, the most powerful tool in distinguishing a true brain wave from an artifact is to establish its specific topography. Here, the major operating principle is that biological events recorded on the scalp tend to have a point of maximum voltage with the surrounding measured voltages diminishing with varying steepness from the point of maximum (see Figure 6-1). The voltage gradients seen with electrocerebral events are expected to have some degree of “smoothness.” In contrast, the electric fields of artifacts may have a patchy and unpredictable contour (compare to Figure 6-2).
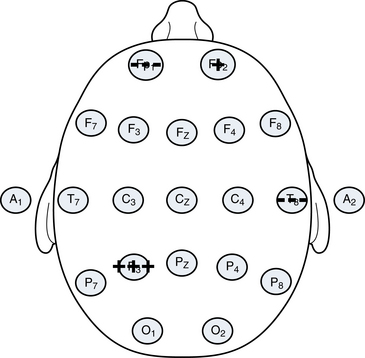
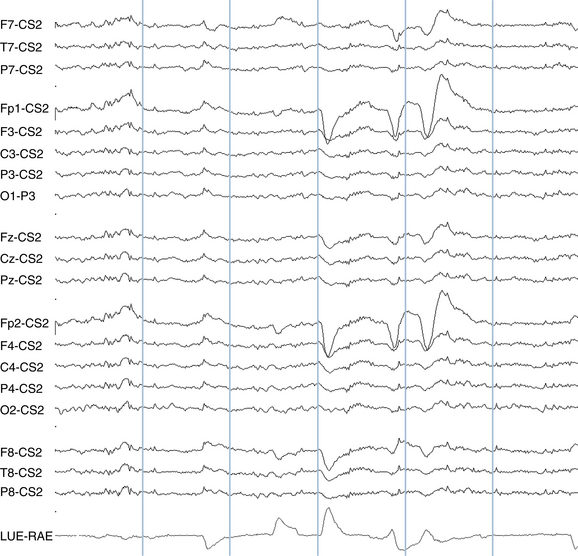
A second principle is that the polarity of most discharges tends to be consistent. Most discharges, if negative at their maximum point, remain negative wherever they are detected on the scalp as shown in Figure 6-1. In general, negative events tend to be negative everywhere, and positive events tend to be positive everywhere. Exceptions to this rule exist, including the occasional examples of discharges that manifest a so-called horizontal dipole (the example of the “horizontal” or tangential dipole is discussed in detail in Chapter 10, “The EEG in Epilepsy”). Even in the small minority of epileptiform events that manifest a simultaneous combined positivity and negativity, those areas of opposite charge are usually segregated in a simple and orderly fashion rather than showing a pattern of several separated regions of positivity and negativity (see Figure 6-3).
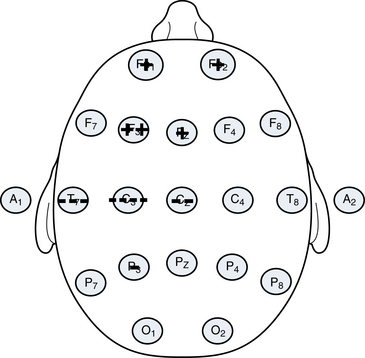
Figure 6-3 A schematic of a “horizontal dipole” is shown, a relatively uncommon finding outside of benign rolandic epilepsy and related syndromes. In contrast to most discharges that show a single polarity on the scalp at any one time (usually negative), in this example, a negative charge and a positive charge are recorded on the scalp simultaneously. Even though both polarities are present, the transition between the two is smooth. The configuration shown here of a negativity in the centrotemporal area and a positivity in the anterior head regions is characteristic of the so-called rolandic spike, discussed in more detail in Chapter 10, “The EEG in Epilepsy.”
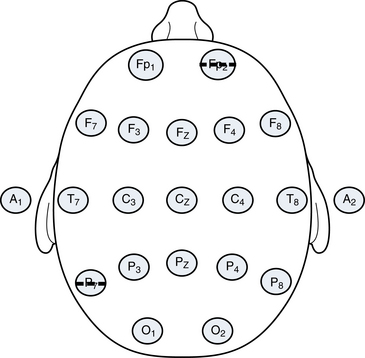
Patterns with significant charge inconsistencies are also not expected from biological systems. The example of an apparent discharge with strong negativities in the left posterior quadrant and the right anterior quadrant but no measured voltage change in the intervening areas as depicted in Figure 6-4 is not likely of cerebral origin. Because this is not a “biological” pattern, there would be a strong suspicion of motion or some other type of artifact having affected two distant electrodes. This pattern and the pattern that was seen in Figure 6-2 may be produced by the haphazard jostling of electrodes during patient movement.
Whenever analyzing any wave on the EEG page, the reader should visualize the voltage topography of the discharge to confirm a distribution of charge that is potentially consistent with cerebral activity. Usually with a bit of practice this can be done quickly. Discharges with bizarre or unpredictable electrical fields likely represent artifact. The importance of localization skills cannot be overemphasized and it is for this reason that the techniques of localization discussed in Chapter 4, “Electroencephalographic Localization,” should be mastered before moving on.
Some significant EEG diagnostic challenges occur when patients are referred for the question of whether sudden movements are epileptic. The diagnostic problem is made more difficult in that each movement may generate a motion artifact causing the appearance that each is correlated with an EEG burst. There would be no difficulty if the movement in question were, for instance, a nonepileptic twitching of the hand because a hand movement would not cause motion artifact in distant scalp electrodes. The hand movement would occur during the study, and there would be no EEG change, strongly suggesting that the hand movements were nonepileptic. If the movement involves the head, however, there may be a simultaneous burst in the EEG, creating some confusion as to whether the movement caused the wave (and is an artifact) or the wave caused the movement (and is an epileptiform discharge). The approach to this problem takes into account that when the head moves, is turned on the pillow, or is subject to some other type of external movement, the pattern of electrodes that are disturbed tends to be more random. Artifacts caused by electrode motion or head motion tend to show a nonregular distribution of inconsistent voltages like those shown in Figures 6-2 and 6-4. In comparison, the patterns associated with electrocerebral activity are expected to show more consistent polarities and a voltage gradient that tapers with distance from the point of maximum.
SPECIFIC TYPES OF EEG ARTIFACT
Artifacts Associated With Eye Movements
Eyeblink Artifact
Electroencephalographers know that when individuals close their eyes, the globes of the eyes deviate upward. This comes as a surprise to some because when we watch a person casually blink or close the eyes, this upward movement of the globes is hidden from view by the closed eyelids. It is only in special situations that this reflex upward eye deviation with eye closure, termed Bell’s phenomenon, is readily observable. Bell’s phenomenon becomes strikingly evident in the case of individuals who suffer from Bell’s palsy. In Bell’s palsy, there is a paralysis of the facial nerve (cranial nerve VII), one of whose functions is to close the eyes. The nerves that move the globe of the eye (cranial nerves III, IV, and VI) are unaffected in patients with Bell’s palsy. Therefore, Bell’s palsy patients have normal eye movement but cannot close the affected eyelid. Thus, the facial nerve paralysis caused by Bell’s palsy literally uncovers Bell’s phenomenon—we can see what the globe of the eye is doing during intended eyelid closure. Bell’s palsy patients have normal eye closure on the unaffected side, but when blinking or closing the eye on the paralyzed side, the globe of the eye can be seen to deviate upward, unhidden by the eyelid. Upward deviation of the globes may also be seen when a person’s eyelids are forcibly pried open during attempted voluntary eye closure. Finally, in some individuals who are in the process of falling asleep, especially babies, the eyelids may lower to a “half-mast” position but do not completely close. Because of a partial Bell’s phenomenon associated with the partial eye closure, only the whites of the eyes can be seen in the half-open palpebral fissures.
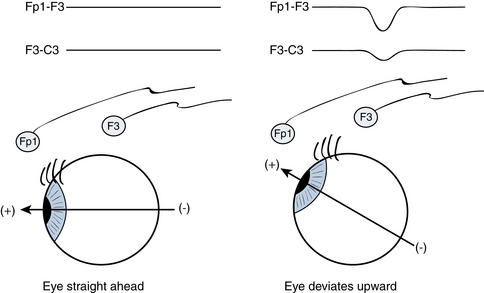
The type of artifact that an upward movement of the globes might cause during eye blinking or eye closure is not intuitively obvious without knowing that the globe of the eye has a particular distribution of charge. As it happens, the cornea (the front of the globe of the eye) carries a net positive charge and the posterior pole of the globe carries a net negative charge, forming a dipole. Because of the presence of this positive charge on the cornea, the bobbing upward of the eye with eye closure is easily detected by EEG electrodes. Figure 6-5 illustrates how the EEG electrodes closest to the eye “perceive” an eyeblink. With upward eye deviation, the electrodes closest to the globes, Fp1 and Fp2, perceive the strong positivity of the corneal surfaces. The F3 and F4 electrodes, which are immediately posterior to the Fp1 and Fp2 electrodes, also pick up some of this positivity, but to a much lesser degree than the Fp1 and Fp2 electrodes. With Fp1 being more positive than F3 and Fp2 being more positive than F4, the Fp1-F3 and Fp2-F4 channels show the characteristic sharp, downward-sweeping waveforms of eyeblink artifact (see Figure 6-6). A similar type of artifact is seen with eye fluttering (see Figure 6-7).
A useful general rule regarding eyeblink artifact is that it should not be detectable in the electrodes of the posterior half of the head; movements of the globes of the eye should not be perceived by the parietal or occipital electrodes because they are too distant. Eyeblink artifact is only occasionally picked up by the central electrodes, C3 and C4, and when it is it should be of low voltage (see Figure 6-8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree