Chapter 5
Electromyography of Laryngeal and Pharyngeal Muscles
Although laryngeal EMG (LEMG) can provide valuable diagnostic information in conditions in which there is suspicion of neuromuscular injury, it is also used for other purposes, most commonly therapeutic injection of the intrinsic laryngeal musculature (Table 5.1).
History
Laryngeal electromyography was first described in 1944 by Weddell et al1 even before the technique was standard in the evaluation of truncal and limb neurologic disorders. It was one year later when the first EMG machine designed specifically for clinical use was made by Golseth.2,3 Over the course of the next 30 years, electromyography gradually became accepted as the clinical standard for diagnostic and prognostic evaluation of the neuromuscular system.
|
The field of LEMG was greatly advanced in the late 1950s by Faaborg-Anderson,4 who published a detailed treatise describing the activity of the laryngeal muscles during both phonatory and nonphonatory tasks. Buchthal5 and Hirano6 were also early pioneers in the field, applying newer findings of motor unit morphology to EMG studies of the larynx. The success of EMG-guided botulinum toxin injections for the treatment of laryngeal dystonia, as reported by Blitzer,7 stimulated more widespread incorporation of LEMG into clinical practice. The utility of LEMG in the evaluation of suspected laryngeal neurologic disorders has been described by many investigators, and it is rapidly becoming accepted as the standard of care in the diagnosis and treatment of the injured and neurologically impaired larynx.8–23
Electromyography Recording and Techniques
For the most part, LEMG is performed using a needle recording electrode and surface reference and ground electrodes. The electrical activity at the recording electrode is compared with that of the reference electrode, which has been designated as zero. The difference between these two points is determined and displayed on the oscilloscope or computer screen and via loudspeaker, enabling visual and audio interpretation.
The electrical charges are represented as either positive or negative. By convention electrical positivity is represented by a downward deflection, whereas electrical negativity is represented by an upward deflection of the tracing. It is important to note that the acoustic signal is essential to the proper performance of the EMG exam, and experienced electromyographers can identify the abnormal patterns more efficiently by ear than by visualization.
In brief, a needle electrode (the active or sampling electrode) is inserted through the skin and into the muscle of interest. Reference and ground electrodes are placed over the skin of the neck or upper chest. Proper insertion is verified by asking the patient to perform appropriate verification tasks (such as vocalization for the vocalis muscle or sniffing for the posterior cricoarytenoid muscle). EMG evaluation consists of sampling three types of electrical activity—insertional, spontaneous, and volitional muscle activity.
When a needle is inserted into a relaxed muscle there is a short burst of normal electrical activity that occurs due to disruption of the muscle membrane, which is termed insertional activity. If the test muscle is completely at rest, after the dissipation of the insertional activity, there should be almost complete electrical silence in a normal muscle. Any electrical activity present is termed spontaneous activity and is abnormal. Volitional activity is evaluated by asking the individual to contract the test muscle. During volitional contraction, the morphology of individual motor unit potentials (MUPs) is evaluated. The individual is then asked to perform a sustained contraction and the recruitment pattern of the muscle is sampled.
Although the basic principles are similar, laryngeal and pharyngeal EMG has some differences as compared with the EMG of limb musculature. Because the intrinsic laryngeal musculature is phasically activated to a low degree with respiration, it can be challenging to evaluate insertional and spontaneous activity, which relies on evaluation of electrical activity at rest. In addition, it can be difficult to evaluate interference patterns in selected muscles because individuals may not be able to reliably perform a sustained contraction of the test muscle (sniffing and swallowing are by nature intermittent processes). Finally, correct electrode placement may be difficult due to the fact that each target muscle is small, close to other muscles, and nonpalpable. In cases of paralysis or synkinesis, absent or misleading electrical activity may make electrode placement even more challenging. Thus, extensive familiarity with anatomy is mandatory for accurate electrode placement.
The spectrum of abnormal EMG findings is broad; none are pathognomonic for a specific disease entity, and in themselves cannot provide a definitive diagnosis. The significance of any finding depends on the frequency of its occurrence, pattern of occurrence among various muscles, time course in relation to the original injury, and clinical context; for this reason there are few lists of strict diagnostic criteria for specific diseases in the EMG literature.
Laryngeal Electromyography Techniques
There are six basic components of the technique of laryngeal EMG (Table 5.2), which are discussed in the following subsections.
|
Patient Positioning and Preparation
Consent is obtained. Patients are counseled that the major risks are bleeding and infection, with a diminutive risk of airway compromise. They may have a transient change in their voice due to needle manipulation. Testing is deferred if there is overlying skin infection or an acute laryngitis. We do not routinely request patients to stop anticoagulants, including aspirin, nonsteroidal antiinflammatory drugs (NSAIDs), and Coumadin, and we have not encountered airway complications in over 20 years of testing. Although the pacemaker spike is seen on the oscilloscope, the EMG tracing can be recorded and the pacemaker artifact ignored. Routine diagnostic EMG does not affect electrical cardiac pacing. Deep brain stimulation and vagal nerve stimulation create an extensive artifact that precludes meaningful testing, and must be temporarily turned off to allow for diagnostic LEMG.
We prefer to position the patient reclining in a chair with the neck extended using a modest shoulder roll. Although some examiners prefer to sit at the head of the patient, we prefer to stand at the patient’s side. A local anesthetic can be used at the cutaneous insertion site, although this may affect the signal given by the cricothyroid muscle if the anesthetic diffuses to this area. If the patient reacts strongly with coughing, anesthetic can be dribbled into the airway via the cricothyroid membrane, although this can also blunt the EMG reading.24 For most individuals we do not find it necessary to use an anesthetic.
Electrode Placement and Verification (Fig. 5.1)
- Cricothyroid: The needle is inserted 5 mm lateral to the midline at the level of the lower edge of the cricoid cartilage and directed toward the inferior tuberculum of the thyroid cartilage.
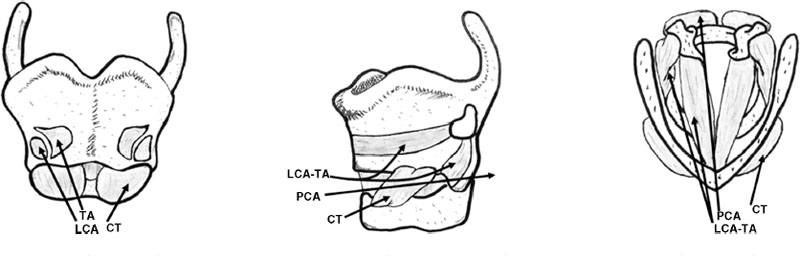
Fig. 5.1 Needle electrode placement for the thyroarytenoid (TA), cricothyroid (CT), lateral cricoarytenoid (LCA), and posterior cricoarytenoid (PCA).
- Verification gesture:
- Activity with glissando (slide pitch of voice from low to high)
- No activity with raising head (straps)
- Activity with glissando (slide pitch of voice from low to high)
- Verification gesture:
- Thyroarytenoid: The needle is inserted at or just lateral to midline at the level of the cricothyroid membrane and directed superolaterally toward the superior tuberculum of the thyroid cartilage.
- Verification gesture:
- Activity with phonation of /e/
- No activity with sniffing (posterior cricoarytenoid, PCA) or with raising head (straps)
- Activity with phonation of /e/
- Lateral cricoarytenoid: The needle is inserted 7 to 8 mm lateral to midline at the level of the cricothyroid membrane and directed superolaterally toward the superior tuberculum of the thyroid cartilage.
- Verification gesture:
- Activity with phonation of /e/
- No activity with sniffing (PCA) or with raising head (straps)
- Activity with phonation of /e/
- Posterior cricoarytenoid: The PCA muscle can be sampled transcutaneously by two methods. If the patient is sufficiently relaxed, the examiner can rotate the larynx by catching the thumb of the noninjecting hand behind the posterior edge of the thyroid lamina. The anterior aspect of the cricoid ring is palpated with the index finger. The needle is inserted just superior and lateral to the index finger, traversing the inferior constrictor until it stops against the rostrum of the cricoid cartilage. Alternatively, the needle may be inserted through the cricothyroid membrane in the midline, traversing the subglottic space (there will be the characteristic airway “buzz” from the amplifier) and piercing the posterior lamina of the cricoid cartilage just to one side of the midline. The needle will often harbor a cartilage plug requiring moderate force to inject the medication. This approach is most successful in younger patients before extensive cartilage ossification has occurred.
- Verification gesture:
- Activity with sniffing
- No activity during phonation
- Activity with sniffing
- Interarytenoideus: With endoscopic guidance, the needle is inserted transglottically, piercing the interarytenoideus muscle in the midline between the arytenoids towers.
- Verification gesture:
- Activity with phonation
- Cricopharyngeus: The cricoid cartilage is palpated, and if possible, the larynx is rotated for injection of the PCA. The insertion site is just at the inferior border of the cricoid cartilage, hugging the trachea. The patient should be asked to sniff, and if there is muscular activity with this gesture the needle should be repositioned more inferiorly. The cricopharyngeus is tonically constricted, but relaxes with swallowing; thus there will be a tonic EMG signal that temporarily abates with each swallow.
- Verification gesture:
- There will be tonic activity that silences during swallow
- No activity with sniffing (PCA) or with raising head (straps)
- There will be tonic activity that silences during swallow
- Many intrinsic laryngeal muscles can also be sampled transorally using curved instruments and hook-wire electrodes, with the exception of the cricothyroideus (Table 5.3).
- Verification gesture:
| Muscle | Nerve | Verification Gesture |
| Levator palatine | X | /s/ |
| Palatoglossus/ palatopharyngeus | X | Swallow |
| Genioglossus/hyoglossus | XII | Protrude tongue |
| Sternocleidomastoid/trapezius | XI | Turn head/raise shoulder |
| Anterior belly digastric | V | Open mouth |
| Masseter/temporalis/internal pterygoid | V | Clench jaw |
| External pterygoid | V | Move jaw from side to side |
| Facial musculature | VII | Facial expression |
Electromyography Patterns
Electromyography activity can be classified into three types: insertional, spontaneous, and volitional. Upon insertion into a relaxed muscle, irritation by the needle itself causes sporadic individual fibers to depolarize. This activity is normal and should not persist 400 milliseconds beyond the time of any needle movement. Prolonged insertional activity is considered a sign of pathologic muscle membrane instability. Alternatively, a needle placed into a muscle in which there is only a very small burst of electrical activity may indicate atrophy, as occurs with long-standing paralysis. There is nothing specifically diagnostic about insertional activity; it is simply an evaluation of the irritability of the muscle membrane. It is difficult to evaluate for insertional activity during LEMG because laryngeal muscles are never truly at rest.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







