39 Endoscopic-Assisted Transnasal Craniectomy Approach to Esthesioneuroblastoma
Aldo Cassol Stamm, Larry H. Kalish, Fernando Oto Balieiro, Iulo Barauna, and David W. Kennedy
 Introduction
Introduction
Esthesioneuroblastoma (ENB) is a rare, malignant tumor of neural crest origin arising from neurosensory receptor cells of the olfactory epithelium, lying in the nasal cavity and paranasal sinuses. It is also referred to as an olfactory neuroblastoma, which better describes the origin and nature of the tumor. It accounts for 3 to 5% of cancers of the nasal cavity1 and has a wide age range (3–90 years) with a bimodal age distribution with peaks in the second and fifth decades.2–4 Both sexes are equally affected, and there is no apparent racial predilection.
 Etiology
Etiology
The basal cells of the olfactory neuroepithelium are presumably the progenitors of the esthesioneuroblastoma. No known causal factor exists for this tumor, and no hereditary patterns have been described for this neoplasm.1
 Pathology
Pathology
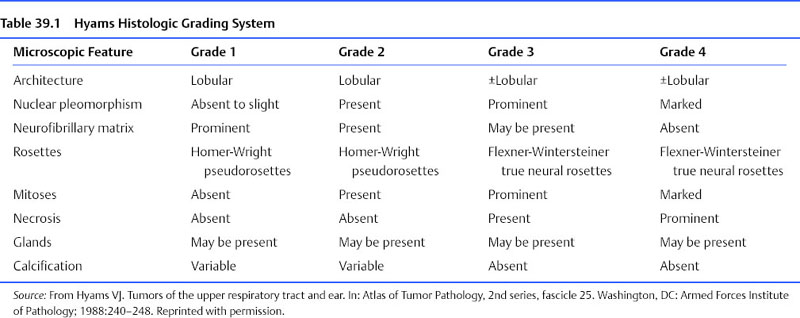
Hyams5 developed a pathology grading system with four grades to classify esthesioneuroblastomas based on their histologic features (Table 39.1). The utility of this grading system has been questioned. Some studies have correlated it with survival and prognosis,1,6–8 whereas others have failed to show any useful correlation.9,10 Many studies have combined grades 1 and 2 into low grade and grades 3 and 4 into high grade.6
These tumors have a tendency to spread locally through the submucosal plane of the paranasal sinuses and invade the anterior cranial base. Extension to the brain and subarachnoid space may follow.11 Hematogenous spread and lymphatic spread have also been well described with locoregional metastases to cervical lymph nodes seen in 10% to 30% of patients with esthesioneuroblastoma,2,12 and distant metastases to the lung, bone, and other atypical sites have been reported less frequently.11,13–17
 Clinical
Clinical
The most common presenting symptoms include unilateral nasal obstruction, recurrent epistaxis, and anosmia.18,19 The presenting symptoms are related to the site and local invasion of the tumor, so that occasionally these tumors may present with eustachian tube obstruction and a unilateral middle ear effusion, or diplopia with a rapid proptosis and visual loss.18 They may also be associated with hormone excess syndromes such as Cushing syndrome20,21 or the syndrome of inappropriate antidiuretic hormone secretion (SIADH).22
 Treatment
Treatment
Although there is no consensus about the treatment of these tumors, many clinicians believe that control is best achieved by combining surgery with adjuvant therapy, such as radiotherapy and chemotherapy.23–27
Craniofacial resection with or without bifrontal craniotomy has been considered the standard surgical approach to ENB, and must be considered the gold standard with which all other treatments are compared.28 Craniofacial resection has the advantage of providing excellent intradural and extradural exposure of the structures of the anterior cranial fossa, and facilitates a multilayered reconstruction. The associated surgical morbidity includes postoperative cerebrospinal fluid (CSF) leak, meningitis, bone flap infection, wound infection, hemorrhage, and symptomatic pneumocephalus. Many series have reported a relatively low incidence of complications (22–30%), with some complications resulting from postoperative radiotherapy. Many studies, however, do not address the effects related to retraction of the frontal lobes and the high incidence of anosmia seen even in unilateral tumors.23,24,26,28,29 Complications have improved over time with the advances in perioperative care, but are higher in older patients and in centers performing fewer procedures30,31
Endoscopic technology, techniques, and instrumentation have all evolved significantly, and the visualization provided by the use of endoscopes during tumor resection is unsurpassed, resulting in more frequent utilization of an endoscopic approach in the resection of these tumors.24,26,32,33 This approach may be limited to assisting in the nasal component of the craniofacial resection (endoscopic-assisted craniofacial resection) to complete the tumor resection using a solely endoscopic access. Whichever technique is employed, it is critical that the important precepts of oncologic resection be maintained.
The debate as to the best technique continues; however, a recent meta-analysis supports endoscopic approaches.34 Surgery was clearly shown to be superior to nonsurgical treatment modalities. Endoscopic surgery produced better survival rates than open surgery, but this is confounded by the larger number of patients with more advanced tumors undergoing open surgery compared with endoscopic. There is also considerable interinstitution and intersurgeon discrepancy and potential publication bias.34
 Staging
Staging
When deciding on the approach, the stage of the tumor must be carefully considered. Kadish et al35 in 1976 designed the most widely used pretreatment staging system for ENB This system divides patients into three groups: group A, tumor strictly confined to the nasal cavity; group B, tumor involving the nasal cavity and the paranasal sinuses; and group C, tumor extending beyond the nasal cavity and the paranasal sinuses into the intracranial compartment. The more advanced the Kadish staging, the worse the outcome; however, this staging system does not address the issue of tumor metastasis or extension to extracranial sites.6,8 A fourth group, group D, tumor with cervical nodes or distant metastasis, is frequently added to this staging system.36 Biller et al37 devised a tumor-node-metastasis classification for esthesioneuroblastoma, whereby tumor extension was more clearly defined. Although more detailed than the Kadish system, it requires a craniotomy for staging and assumes universal cribriform plate involvement. Dulguerov and Calcaterra23 modified this tumor-node-metastasis classification system, but the Kadish system is still more widely used due to its simplicity and prognostic value.
We believe that an additional shortcoming of the Kadish system is its inability to provide significant guidance with regard to surgical expectations and appropriate treatment modality, and that the stages are not fully applicable to the concepts of endoscopic transnasal resections.
Whereas the Kadish system differentiates between tumors confined to the nose and those involving the sinuses, with endoscopic-assisted transnasal craniectomy (EATNC), this differentiation is of limited importance in terms of surgical approach, and probably also is of limited prognostic importance. But for tumors that extend beyond the nose and paranasal sinuses, it becomes critically important to differentiate whether the tumor involves the dura or the orbit, because the appropriate surgical approach would differ markedly, and this differentiation is not achieved by the Kadish staging.32,38,39 Similarly, it appears reasonable that, over time and given a sufficiently large series, differences in survival rates may also become evident between these two involvement sites. In terms of dural involvement, we believe, as do many surgical oncologic centers, that it is also important to determine whether the tumor involves just the dura or extends intracranially, and, if it does extend intradurally, whether it is still a tumor that can be resected with EATNC or will require a craniofacial approach.
We use the following staging system: stage 1, tumor confined to the nose and paranasal sinuses; stage 2, dural involvement; stage 3, orbital involvement; stage 4, intracranial involvement; stage 5, regional or distant metastases (Fig. 39.1).
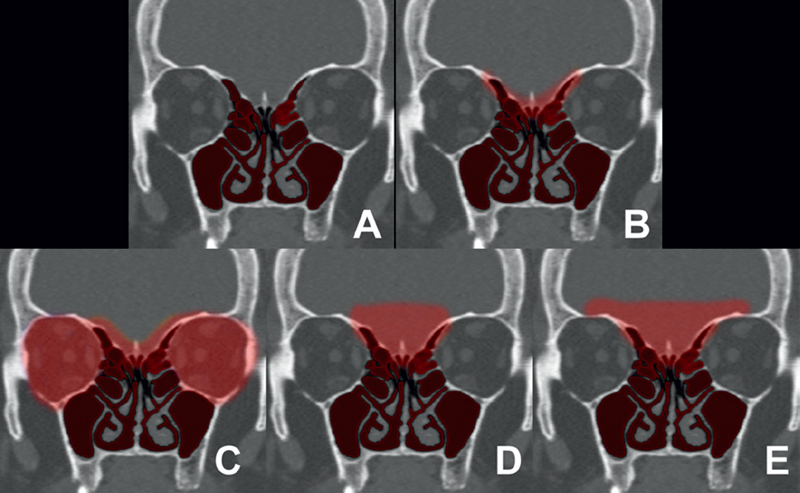
Fig. 39.1 Normal coronal computed tomography (CT) painted with the novel Stamm-Kennedy esthesioneuroblastoma staging system. (A) Stage 1. (B) Stage 2. (C) Stage 3. (D) Stage 4A. (E) Stage 4B.