38 Endonasal Surgery of Malignancies of the Sinus and Skull Base
Paolo Castelnuovo, Maurizio Bignami, Paolo Battaglia, Andrea Bolzoni Villaret, and Piero Nicolai
 Introduction
Introduction
The application of endoscopic surgery for the management of sinonasal malignancies emerged in the last 10 years as a valid and safe alternative to the gold standard represented by anterior craniofacial resection (ACFR).1–6 This application was made by four factors: the creation of a multidisciplinary skull base team of an otolaryngologist and a neurosurgeons, the experience acquired with endoscopic procedures in the treatment of benign lesions and skull base defects, technical improvements in surgery and radiology, and the acceptance of piecemeal resection.
 Indication and Advantages
Indication and Advantages
Indications for an endoscopic endonasal approach (EEA) have been modified by our group over a 10-year period.6 Up to 2003, only patients with limited nasoethmoidal lesions that did not infiltrate the external bony boundaries of the ethmoid (i.e., lamina papyracea, cribriform plate, ethmoid roof), with minimal extension into the maxillary or frontal sinus, were considered eligible for EEA. From 2004, the indications have been extended to include advanced lesions in contact with or minimally infiltrating the dura. In the last 2 years, selected intradural lesions without brain infiltration also have been treated.7
The advantages of endoscopic techniques include avoidance of facial incisions and osteotomies, short hospitalization, a very limited morbidity, and the possibility of avoiding any brain retraction. The major advantage lies in the outstanding magnified visualization of the site of origin as well as of the areas involved by the tumor. The use of angled telescopes permits viewing behind the corner, providing better visualization of the structures involved by the tumor.
 Contraindications
Contraindications
An EEA is contraindicated if there is a lateral extension over the orbital roof, or extensive involvement of the brain; in these situations, a cranioendoscopic or a standard ACFR is performed. Other contraindications for EEA are extensive lacrimal pathway infiltration, involvement of the anterior wall and lateral portion of the frontal sinus, infiltration of the bony walls of the maxillary sinus with the exception of the medial one, infiltration of the hard palate, and erosion of the nasal bones.
 Diagnostic Workup
Diagnostic Workup
The preoperative diagnostic workup includes endoscopic examination of the nasal cavity to evaluate the borders and the features of the lesion as well as the sinonasal and septal anatomical variations, and magnetic resonance imaging (MRI) with gadolinium enhancement, except with uncooperative patients, in which case computed tomography (CT) with contrast medium is performed instead. MRI with gadolinium enhancement is preferable to CT because it provides better delineation of the interface between the tumor and the surrounding soft tissues (periorbita, orbital content, dura).
In very aggressive histologies (e.g., malignant melanoma, malignant schwannoma, neuroendocrine carcinoma, undifferentiated carcinoma) a positron emission tomography (PET)-CT is included in the preoperative assessment to evaluate the presence of systemic dissemination of the disease. All patients should be informed that it might be necessary to switch intraoperatively to a transfacial or transcranial approach in case any unexpected contraindication is found during the surgery.
 Surgery
Surgery
Instrumentation
The following instrumentation is required for the endoscopic approach to sinonasal malignancies of the sinonasal tract and the anterior skull base: high-quality 0- and 45-degree endoscopes; video equipment (camera and monitors); a recording system; long-handle endoscopic bipolar forceps; curved and double-curved cutting instruments; diode laser supports; long stem and curved drills; long dissection instruments and dural reconstruction instruments; and intranasal vascular Doppler. The use of a microdebrider is strongly recommended. Cavitron and ENT navigation systems can be helpful.
Operative Setup
The patient is placed in a supine, 10- to 20-degree reverse-Trendelenburg position, with the head slightly hyperextended. The surgeon stands on the right side of the patient and the assistant stands on the left side. The nurse stands on the right of the operating surgeon. The anesthesiologist stands on the patient’s left side with the anesthesiology equipment, next to the assistant. Hypotensive general anesthesia is required.4 The nasal cavity is decongested with topical application of oxymetazoline chlorohydrate (10 mL), mixed with oxybuprocaine (10 mL) and adrenaline (1 mL).
Approach
The approach consists of six main steps (Fig. 38.1):
1. The tumor is debulked through cutting instruments, powered instruments (microdebrider or ultrasonic aspiration, high-speed burrs), or angled and malleable instruments, to clearly identify the possible site of origin of the lesion. En-bloc resection can be achieved only in small tumors.
2. The nasal branch of the sphenopalatine artery is cauterized by bipolar instrumentation. The vomer is detached from the sphenoidal rostrum using an intranasal drill, and a large sphenoidotomy is performed. A diode laser is used to remove the posterior two thirds of the septum. These first two steps widen the surgical field and enable both surgeons to work together through both nostrils. Using aspirators and grasping instruments, the second operating surgeon can help in controlling bleeding as well.
3. A Draf III frontal sinusotomy is performed, a subperiosteal dissection of the nasoethmoidosphenoidal complex (mono- or bilateral) is performed, and the surgical specimen is removed either transnasally or transorally. If necessary, this step can include medial maxillectomy and resection of the nasolacrimal duct. Multiple biopsies from the surgical margins are routinely sent to the laboratory for frozen sections.
4. The lamina papyracea and the ethmoid roof, including the cribriform plate, need to be removed only when the lesions involve their mucosal covering.
5. Radiologic or intraoperative findings of any suspicious contact or infiltration of the dura or periorbita require their resection and frozen sections at this site to evaluate margins. A diagnosis of olfactory neuroblastoma (ONB) also requires dura and olfactory bulb resection due to its high propensity to spread along the olfactory phyla. It is better to dissect the dura from the underlying ethmoidal roof with dedicated instrumentation before opening the dura. The dissection of the epidural space is a key point in EEA.
6. Duraplasty with a “three-layer” technique is preferably performed using autologous material: fascia lata or an iliotibial tract both for the intradural and intracranial extradural layers (underlay) and for the extracranial layer (overlay), stabilized with fat tissue and fibrin glue. No bone or cartilage graft is used to repair the skull base to avoid radionecrosis and infection after postoperative radiotherapy. If possible, a vascularized septal flap pedicled on the nasal branch of the sphenopalatine artery8,9 can be used as a third layer. Our group usually does not utilize this flap because of the frequent involvement by the tumor of the septum.
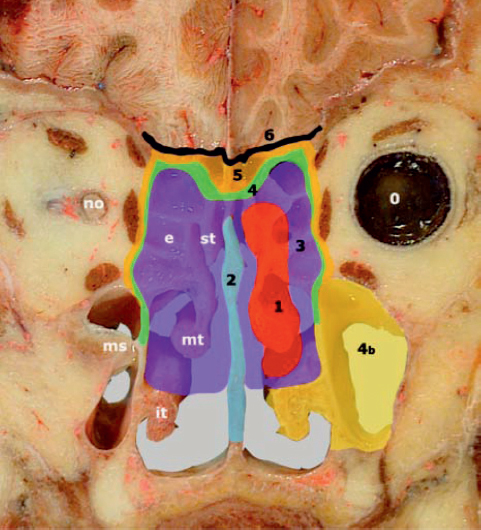
Fig. 38.1 The six main steps of the endoscopic endonasal approach (EEA) are presented schematically on a cadaveric specimen: 1, tumor debulking; 2, removal of the septum; 3, Draf III, with centripetal removal of the ethmoidosphenoidal “box”; 4, removal of bone/cartilage in contact with the tumor; 5, removal of connective tissue around the tumor; 6, skull base duraplasty. E: ethmoid; it.:inferior turbinate; ms.: maxillary sinus; mt.: middle turbinate; no.: optic nerve; o: orbit; st.: superior turbinate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



