Chapter 85 Endovascular Treatment of Stroke
Stroke is the third leading cause of death in the United States, accounting for more than 143,000 deaths each year. The Centers for Disease Control and Prevention estimates approximately 795,000 strokes occur annually in the United States. Of these, 610,000 are sentinel events, with the remainder occurring in those who have suffered a prior stroke.1 Stroke is a leading cause of long-term disability due to loss of independence, language, motor skills, and cognitive abilities.1 The American Heart Association has estimated the financial burden of stroke to be nearly $70 billion in 2009 due to both direct and indirect costs.2 Although acute stroke is dichotomized into both ischemic and hemorrhagic etiologies, the vast majority of strokes are secondary to ischemia. Roughly 80% to 85% of acute strokes are secondary to thromboembolic vessel occlusion, typically arising from cardiac, carotid, or intracranial artery pathology.3
Timely arterial recanalization and prevention of reocclusion after treatment have become integral foci of the modern management of acute stroke. Current therapeutic modalities include intravenous chemical thrombolysis, intra-arterial mechanical and chemical thrombolysis, and stenting. Rapid diagnosis and treatment of acute stroke have been shown to improve patient outcomes in multiple studies.4–10 However, multiple barriers exist that may prevent patients from receiving timely revascularization, including delay in diagnosis, resource constraints, and lack of physicians trained in stroke management. Regionalization of stroke care has been popularized in recent years in the United States to combat such barriers. Despite these efforts, it is estimated that less than 1% of patients suffering an acute stroke receive intravenous thrombolytic therapy.11 The recent results of the third European Cooperative Acute Stroke Study (ECASS), which showed benefit in patients who received intravenous recombinant tissue plasminogen activator (rtPA) within 4.5 hours of symptom onset,12 may increase the number of patients eligible to receive intravenous thrombolytic therapy.
Occlusion and Recanalization
Arterial recanalization is widely accepted as a surrogate marker of efficacy for stroke therapies. The Thrombolysis in Myocardial Infarction (TIMI) scale is accepted among neurointerventionalists as a semiquantitative measure of vessel recanalization (Table 85-1).13 Transcranial Doppler ultrasonography has also shown promise in evaluating vessel recanalization.14–16 Successful recanalization has been linked to improved clinical outcomes in many series.17 Pretreatment residual flow has been shown to be predictive of both time to achieve recanalization and likelihood of a successful intervention.15 In a meta-analysis of recanalization and outcome, Rha and Saver demonstrated a strong correlation between arterial recanalization and improved functional outcomes with reduced mortality.17 Successful arterial recanalization at the time of intervention does not always correlate with lasting benefit, because some vessels may reocclude. Reocclusion rates as high as 34% have been reported in some studies following intra-arterial administration of rtPA.18–20 In addition, distal propagation of thrombus has been reported in approximately 16% of patients undergoing pharmacologic or mechanical thrombolysis.20 Potential reperfusion injury may occur when the blood–brain barrier becomes destabilized. Secondary cerebral edema and/or intracranial hemorrhage may result, possibly necessitating operative intervention.
TABLE 85-1 TIMI Flow Grading System13
| TIMI Grade | Classification | Criteria |
|---|---|---|
| 0 | No perfusion | No recanalization of the primary occlusive lesion |
| 1 | Penetration without perfusion | Incomplete or partial recanalization with flow past the initial occlusion, but no distal branch filling |
| 2 | Partial perfusion | Partial recanalization with incomplete or slow distal branch filling |
| 3 | Complete perfusion | Full recanalization with filling of all distal branches |
Presentation
Patients suffering an acute ischemic stroke most commonly present with sudden-onset neurologic deficit(s) that localize to the brain territory supplied by the affected vessel(s). It is imperative to perform a thorough but succinct history and neurologic examination to assess the extent of stroke. Physicians must gather information regarding the progression of neurologic deficit over time and any improvements that have occurred since onset, as spontaneous improvement may indicate a transient ischemic attack or point to an alternative diagnosis, such as seizure. The National Institute of Health Stroke Scale (NIHSS) quantitatively rates the severity of the stroke and has demonstrated excellent reliability and clinical utility.21–23 The scale ranges from 0 (no symptoms) to 42 and grades patient deficits in multiple functions, including motor, sensory, language, and alertness. Generally, scores of 1 to 5 represent mild stroke, 5 to 20 moderate to severe stroke, and greater than 20 very severe stroke. The NIHSS and its booklet are accessible online at the National Institute of Neurological Disorders and Stroke (NINDS) Web site (http://www.ninds.nih.gov/).
Imaging
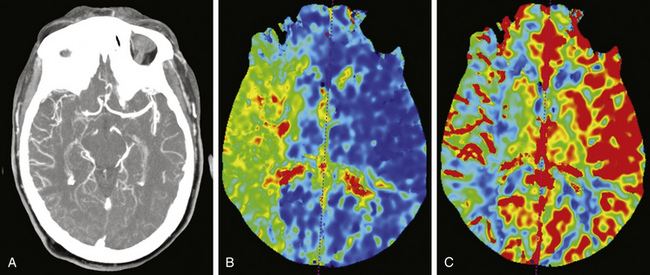
All patients presenting with stroke symptoms should undergo brain imaging. Computed tomography (CT) is the most readily available and efficient imaging modality, although magnetic resonance imaging (MRI) may also be performed. Early noncontrasted CT scanning is critical for evaluation of intracranial hemorrhage and serves as the primary differentiator for standard of care therapies. In addition, noncontrasted CT scanning of the head may reveal hypodensities consistent with evolving territories of infarction, cerebral edema or herniation, loss of gray–white matter differentiation, or arterial occlusion referred to as the “hyperdense sign.” At the University of Florida, computed tomography angiography (CTA) of the head and neck and cerebral CT perfusion are performed on all patients who present with acute stroke symptoms. It is imperative the aortic arch and major arteries of the head and neck be visualized to evaluate for arterial occlusion, flow-limiting stenosis, dissection, or other vessel anomalies. CT perfusion is used to assess the extent of stroke and the amount of potentially salvageable brain parenchyma. Tissue with preserved cerebral blood volume, despite reduced cerebral blood flow and increased mean transit time, represents the stroke penumbra (Fig. 85-1).24,25 CT perfusion may be limited at visualizing the posterior fossa due to significant bone artifact and beam scatter; however, it is hoped that newer imaging technologies and techniques will ameliorate this difficulty. Alternatively, some institutions rely on diffusion-weighted MRI to evaluate the brain’s physiologic state. Whichever modality is used, timely evaluation of actual brain physiology is rapidly becoming a new standard in the cutting-edge treatment of stroke.
Patient Selection
Indications and contraindications for intravenous thrombolysis are listed in Table 85-2. Intracranial hemorrhage is a direct contraindication for revascularization therapy. The therapeutic window for intravenous rtPA has been extended to 4.5 hours from the onset of symptoms based on results of the recent ECASS III trial.12,26 Patients eligible for intravenous rtPA should undergo this treatment prior to attempts at endovascular therapy. If patients fail to improve neurologically with intravenous rtPA, present outside of the therapeutic window, or have a contraindication to intravenous rtPA, endovascular therapy may be considered, including the use of intra-arterial rtPA, mechanical disruption using the microwire, the use of mechanical thrombectomy/aspiration devices, angioplasty, stenting, or a combination of procedures in those with persistent occlusive thrombi.
TABLE 85-2 Indications and Contraindications to rtPA Administration
| Indications | Contraindications |
|---|---|
• Minor or rapidly improving symptoms • Stroke or serious head trauma within the past 3 months • Major surgery within the last 2 weeks • Known history of intracranial hemorrhage • Sustained systolic blood pressure >185 mm Hg • Sustained diastolic blood pressure >110 mm Hg • Aggressive treatment needed to lower the patient’s blood pressure • Symptoms suggestive of subarachnoid hemorrhage • Gastrointestinal or urinary tract hemorrhage within the last 3 weeks • Arterial puncture at noncompressible site within the last 7 days • Heparin received within the last 48 hours and elevated partial thromboplastin time • Prothrombin time >15 seconds | |
| Administration | |
| 0.9 mg/kg infused intravenously over 60 minutes, with 10% of the initial dose given as a bolus over 1 minute |
The relative amount of ischemic parenchyma should be considered strongly when deciding to pursue endovascular treatment. Specifically, unsalvageable tissue (defined by regions with decreased cerebral blood volume in the setting of increased mean transit time and decreased cerebral blood flow on perfusion imaging) comprising greater than one third of the overall brain territory at risk of ischemia is a relative contraindication to endovascular therapy. In our experience, these patients are at high risk of hemorrhagic transformation following intra-arterial pharmacologic and/or mechanical thrombolysis or stenting, particularly if the nonsalvageable region involves the basal ganglia. Other factors linked to poor clinical outcomes in patients undergoing endovascular therapy include advanced age (greater than 75 years), presentation NIHSS score greater than 18, and admission glucose greater than 150 mg/dl.9 While the conventional ideal therapeutic window for endovascular therapy is within 6 to 8 hours of symptom onset,10,26,27 patients are increasingly being successfully treated outside of this time frame guided by physiologic imaging (CT perfusion or MRI perfusion).28,29
Intracerebral Hemorrhage
The major complication of endovascular therapies for stroke is intracranial hemorrhage, which is estimated to occur in roughly 5% to 10% of patients undergoing intravenous tissue plasminogen activator therapy.7,30,31 Clinically significant intracerebral hematomas, so-called symptomatic intracerebral hemorrhage (SICH), develops in around 3% of patients. The frequency of SICH increases with the concomitant presence of early signs of infarction on CT scan prior to administration.31,32 Furthermore, symptom severity, diabetes mellitus, and elevated blood glucose are well-demonstrated independent risk factors for SICH.32,33 Other possible risk factors include high systolic blood pressure, low platelets, advanced age, and delay in treatment. Intra-arterial tissue plasminogen activator, in contrast to venous, has a slightly higher risk of SICH. Estimates of SICH in those receiving intra-arterial thrombolysis are approximately 6% to 12%, while those receiving both intravenous and intra-arterial administration are estimated to be roughly 9% to 20%.10,31
The pathophysiology of post-treatment SICH appears to be primarily the result of reperfusion injury with hemorrhagic transformation at ischemic sites.34 Ischemia results in disruption of the blood–brain barrier, causing leakage from vessels, tissue edema, and loss of autoregulation secondary to increased free radical and matrix metalloproteinase activity.35,36 Reperfusion of damaged vessels results in small ruptures with microhemorrhages that may ultimately enlarge into a hematoma due to disruption of the normal clotting cascade by the presence of thrombolytic agents.
Intravenous Thrombolytic Therapy
Intravenous thrombolytic therapy with rtPA was the first FDA-approved intervention for acute stroke. The NINDS trial, published in 1995, was a large, randomized, placebo-controlled study consisting of more than 600 patients randomized to rtPA versus placebo within 3 hours of stroke onset.4 At 24 hours, no difference was seen in NIHSS improvement between those receiving rtPA and those receiving placebo. At 3 months, patients receiving rtPA had 1.7 times greater odds of a favorable outcome than did those receiving placebo. SICH occurred in 34 of the 312 patients receiving rtPA (20 were symptomatic, of which 9 were fatalities), compared to 11 of the 312 patients receiving placebo (2 symptomatic, 1 fatality). Two additional trials, ECASS I and II, demonstrated comparable results with improved functional outcomes but increased risk of hemorrhage.7,8 These findings led to approval by the FDA of rtPA, at a dose of 0.9 mg/kg, in acute stroke patients presenting within 3 hours of symptom onset.
Recently, trials have focused on the benefits of rtPA beyond the 3-hour window. The Alteplase Thrombolysis for Acute Noninterventional Therapy in Ischemic Stroke (ATLANTIS) trial, published in 1999, evaluated the benefits of rtPA administration between 3 and 5 hours after symptom onset.5 This trial demonstrated no benefit to the administration of rtPA beyond 3 hours. In 2004, published pooled data from the ATLANTIS, ECASS, and NINDS trials suggested a potential benefit in administration beyond the 3-hour window.37 In 2008, Hacke et al. demonstrated significant benefit in clinical outcome at 90 days in patients receiving rtPA within 180 to 270 minutes after symptom onset.12 In 2009, the FDA approved the use of rtPA in acute ischemic stroke in patients 3 to 4.5 hours after symptom onset.
Despite the recent temporal expansion, intravenous rtPA faces several important limitations. Research has demonstrated ineffectiveness in lysing thromboembolic obstruction of large proximal vessels as compared to more distal, smaller vessels.16 One study of 349 patients undergoing intravenous rtPA for stroke revealed nearly one third with no recanalization, one third with partial recanalization, and only one third with complete recanalization.38 In addition, early reocclusion has been demonstrated in up to 34% of patients receiving intravenous rtPA.14,19 To combat these limitations, new endovascular therapies have been developed to provide better targeting of thrombolytic agents with improved recanalization and prevention of reocclusion. These therapies are described in the remaining sections of this chapter.