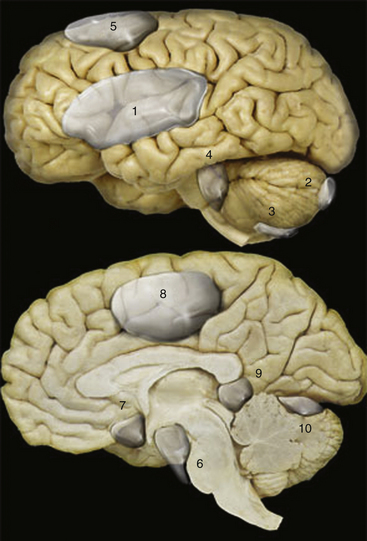
Chapter 26 Arachnoid, Suprasellar, and Rathke’s Cleft Cysts
Most of the intracranial cystic lesions are related to neoplasms, bacterial or parasitic infections, or loss of tissue due to malformation, infarction, or injury, including that resulting from surgical resection of brain tissue. These topics are discussed in other chapters of this book; however, an additional group of cystic intracranial lesions is encountered in neurosurgical practice, and three of these lesions are discussed in this chapter: the arachnoid, suprasellar, and Rathke’s cleft cysts. Of particular interest is that the management of these lesions continues to evolve with the development of endoscopic neurosurgical techniques.1–12
Intracranial Arachnoid Cysts
Arachnoid cysts are intra-arachnoid benign cystic lesions filled with cerebrospinal fluid (CSF).13 According to Cohen and Perneczky,2 in 1831 Bright was the first to describe the intra-arachnoid location of intracranial arachnoid cysts. These lesions are probably developmental in origin and become symptomatic either because of their progressive enlargement or because of hemorrhage into the cyst. The enlargement of arachnoid cysts has been discussed controversially and is at this point in time a matter for discussion. There are various hypotheses to explain the growth of arachnoid cysts:
1. Active fluid secretion from the cyst wall14,15
2. Fluid accumulation caused by an osmotic pressure gradient16
3. Pumping of CSF through a persistent communication between the cyst and the arachnoid space due to vascular pulsation17
4. The so-called slit-valve mechanism, which is described later1,18,19
Arachnoid cysts occur throughout the neuraxis, and generally, no communication is demonstrable between the cyst and the subarachnoid space, although occasionally during surgery an arachnoid cyst is observed being filled through an apparent one-way valve.20,21 Arachnoid cysts may be asymptomatic throughout life, and rarely, they may spontaneously regress;22–24 however, if they do become symptomatic, the progression results from compression on the underlying brain, overlying bone, or both. There is an ongoing discussion whether space-occupying asymptomatic cysts should be operated on to prevent a hindrance to normal brain development and function.25–27 Recently, Di Rocco28 commented on this. He discussed whether past failures in the management of this lesion have allowed to individuate reliable criteria to distinguish those subjects who may benefit of the surgical management from those who should be only observed. He emphasized that there are no clear-cut indications for operative treatment of Sylvian fissure arachnoid cysts, and the absence of defined criteria for postoperative success. In his conclusion, he argued that in many instances, surgical indications are offered based on preferences rather than objective evaluation of individual patients.
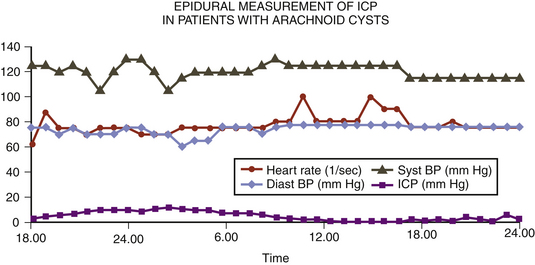
If the indication for surgery is questionable, intracranial pressure (ICP) monitoring should be performed to prove ICP elevation or pathologic pressure waves.4,29 The clinical symptoms resulting from these arachnoid cysts depend greatly on their location—whether over the sylvian fissure; over the cerebral convexity; in the interhemispheric region; in the sella and suprasellar region; around the optic nerve, the quadrigeminal plate, or the cerebellopontine angle; in the region of the clivus; over the cerebellar vermis or cerebellar hemisphere; or within the lateral or fourth ventricle.30–36 Arachnoid cysts have also been described extending across the region of the foramen magnum from the posterior cranial fossa into the upper cervical spine posterolateral to the spinal cord.37–39 The midline lesions often lead to an obstruction of the CSF flow and result in focal symptoms and raised ICP.40–43 There is a continuing discussion about whether intracranial arachnoid cysts are related to a specific seizure type and electroencephalographic focus.44
The arachnoid cyst wall is histologically indistinguishable from normal arachnoidal membrane. Moderate thickening of the arachnoid and an increase in connective tissue are common (Fig. 26-1).45 Ultrastructural studies confirm the similarity of the cyst membrane with the normal meningeal counterpart, including the cell-cell connections and the occurrence of basal laminal structures. Quantitative differences in the contribution of the single components have been found both between different cysts and between cysts and normal arachnoid.
In a recently published microsurgical and endoscopic anatomical study, Inoue and colleagues46 claimed that there are two types of arachnoid membranes: outer and inner. The outer arachnoidal membrane surrounds the whole brain, and the inner membranes divide the subarachnoid space into cisterns. Twelve inner arachnoid membranes and 9 cisterns were identified in this study. A special kind of arachnoid cyst formation consists of a luminal epithelial layer connected with a glial sheet, followed peripherally by a thin connective tissue covering (Fig. 26-2.).
The glial nature of parts of the cyst lining can be shown by glial fibrillary acidic protein staining. Some authors have called these cysts “glioependymal.”47
In many cases, arachnoidal cysts are incidental findings noted on CT scanning or MRI of the head performed for a reason unrelated to the cyst. Such patients are informed about the radiographic finding; provided with a copy of the study so they can present it to a physician at a later date, if necessary; and followed up annually. In approximately 15% of middle fossa arachnoid cysts, an asymptomatic lesion may become symptomatic as a result of bleeding in association with the cyst and raised ICP. This event may occur after minor head trauma.48–50
In a report of 6 cases of subdural hematoma occurring in 18 patients with previously asymptomatic middle cranial fossa arachnoid cysts, Rogers and colleagues51 recommended a cystoperitoneal shunt to treat the cyst after evacuation of the hematoma. Auer and co-workers52 also recommended evacuation of the hematoma and the cyst’s wall in one procedure. Handa and associates53 reported on the two-stage removal of bilateral cysts and hematomas. They recommend that the hematomas be drained initially through burr holes and that 3 months later the cyst wall be resected and a cystoperitoneal shunt inserted. Mori and colleagues as well propose a two-step procedure. Hematoma evacuation is adequate at first operation. If the preoperative symptoms persist, additional arachnoid cyst surgery should be considered.54 Markakis and colleagues55 also recommend a two-stage approach to the management of large arachnoidal cysts, beginning with a shunt procedure, which is followed several weeks later by the resection of the cyst wall and a ventriculostomy. Another treatment option is to evacuate the hematoma through an endoscopic burr hole approach and perform a cystostomy to the CSF space in one procedure.56 Interestingly, successful treatment of middle fossa arachnoid, cysts, which means reduction of cyst size, may not reduce the risk of posttraumatic injury hemorrhage as demonstrated by Spacca and co-workers in a series of 40 patients operated with endoscopic fenestration. Four of these patients experienced a post-traumatic intracystic bleeding after surgery.57
Cerebral convexity cysts occurring in adults present as seizures, headache, raised ICP, and, sometimes, marked reactive thickening of the overlying skull with erosion of the inner table. These cases can be managed by the wide excision of the membranes and the establishment of communication between the cyst interior and the CSF of the subarachnoid space. The same approach has been used in the treatment of symptomatic interhemispheric arachnoid cysts and cysts in the region of the quadrigeminal plate that produce aqueductal obstruction that leads to hydrocephalus. Before the advent of MRI, arachnoid cysts of the cerebellopontine angle often presented a diagnostic dilemma that required differentiation from other mass lesions located in the cerebellopontine angle.31 Cysts of the cerebellopontine angle may mimic other lesions in this location and may cause hearing loss and cerebellar signs. These cysts may present as intermittent downbeat nystagmus with an associated hydrocephalus or as vague symptoms, including hearing loss and disequilibrium, contralateral trigeminal neuralgia, or hemifacial spasm.58–61
Surgical options for the management of symptomatic arachnoid cysts include the endoscopic resection of the cyst wall with opening of the membranes, which establishes communication with the hemispheric or ventricular CSF pathways. Levy and co-workers described their results using the microsurgical keyhole approach for middle fossa arachnoid cysts.62 This procedure can be performed with minimal morbidity via minicraniotomy. Compared with an endoscopic approach, better control of hemostasis can be obtained. The operative time and length of hospital stay were not excessively increased. Other options are stereotactic cyst aspiration,63–65 shunt drainage or drainage of the lesion through a burr hole,66 craniotomy with resection or marsupialization of the cyst walls,67 and craniectomy and ventriculostomy of the cyst.24,68 In a cooperative European study of the management of arachnoid cysts in children, total excision or marsupialization emerged as the first-choice surgical procedure, and shunting procedures were often applied to cysts located in deeper locations. Among the 285 patients, from birth to 15 years of age, there was a resultant reduction of the size of the cyst in approximately two thirds of the cases, and in 18%, the cyst had disappeared completely on follow-up CT scanning.69 Another study of the relative merits of different approaches to the management of arachnoid cysts in children is based on an analysis of 40 children treated between 1978 and 1989 at the University of California, San Francisco. Of 15 patients with cysts that were treated initially by fenestration alone, 67% showed no clinical or radiographic improvement and subsequently required cyst-peritoneal or ventriculoperitoneal shunting. All of these patients improved postoperatively, although shunt revision was required in approximately one third of cases as a result of the recurrence of a cyst. These authors concluded that, irrespective of the location of the lesion, cyst-peritoneal or cyst-ventriculoperitoneal shunting is the treatment of choice.25 However, there is considerable risk of overdrainage with posterior fossa overcrowding and acquired Chiari I malformation, or hindbrain herniation.70
Several groups reported about their results in neuroendoscopic treatment of arachnoid cysts. In a prospective study, Schroeder and coworkers10 treated seven consecutive patients with symptomatic arachnoid cysts in different locations endoscopically. The authors performed cystocisternostomies and ventriculocystostomies via burr holes with the aid of a universal neuroendoscopic system. Symptoms were relieved in five patients and improved in one patient, whereas the size of the cyst decreased in six patients. Although the follow-up period was short (15 to 30 months), the authors recommend neuroendoscopic treatment of arachnoid cyst as the first therapy of choice. The second study was conducted by Hopf and co-workers.6 They evaluated 24 patients with intracranial arachnoid cysts that were treated endoscopically. Their surgical strategy was to create broad communication between the cyst and the subarachnoid space. Various techniques were used: endoscopic fenestration (10 cases), endoscopic controlled microsurgery (5 cases), and endoscopy-assisted microsurgery (9 cases). In all patients sufficient fenestration of the cysts could be achieved, with a favorable outcome in 17 patients. Operative complications included infection (3 patients), bleeding into the cyst (1 patient), and subdural fluid collections (4 patients). The authors conclude that different endoscopic techniques do provide sufficient treatment of selected arachnoid cysts. Recent advances in neurosurgical techniques and neuroendoscopy continue to favor cyst fenestration over shunt insertion as the method of choice for initial cyst decompression.71
Case Report 1: Arachnoid Cyst
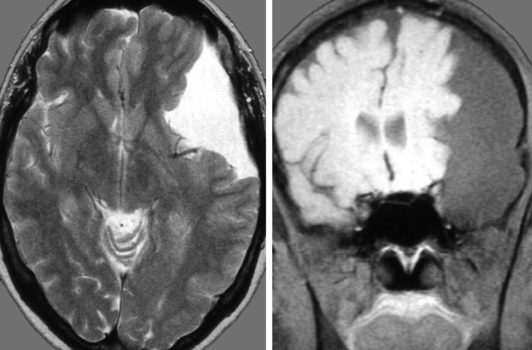
A 14-year-old boy was admitted with aggressive attitude, loss of motivation, headache, and nausea. The neurologic examination was normal. An electroencephalogram showed a left-sided reduction of activity in the frontotemporal region. Magnetic resonance imaging (MRI) demonstrated a large left, frontotemporal arachnoid cyst with a slight mass effect (Fig. 26-3). Epidural ICP measurement during a period of 24 hours revealed normal values (Fig. 26-4). We concluded that the cyst was not related to the patient’s symptoms, and no further intervention was performed. Long-term follow-up examinations showed that the patient was in good neurologic condition with normal age-related capacity.
Case Report 2: Arachnoid Cyst
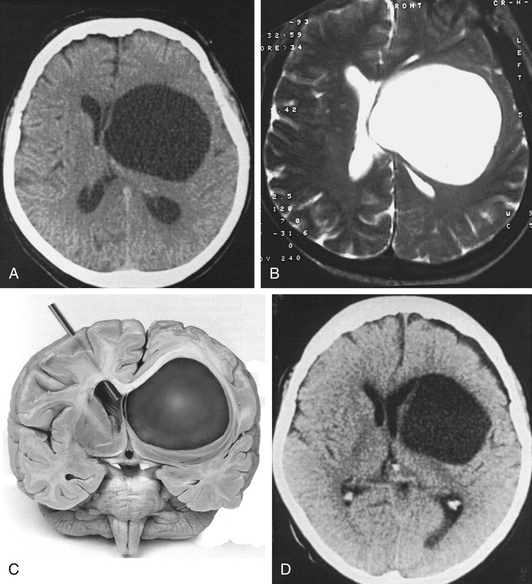
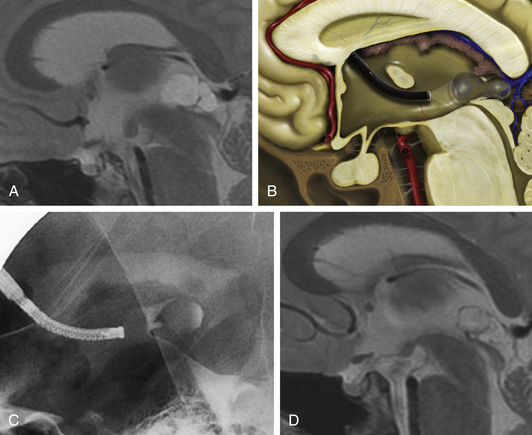
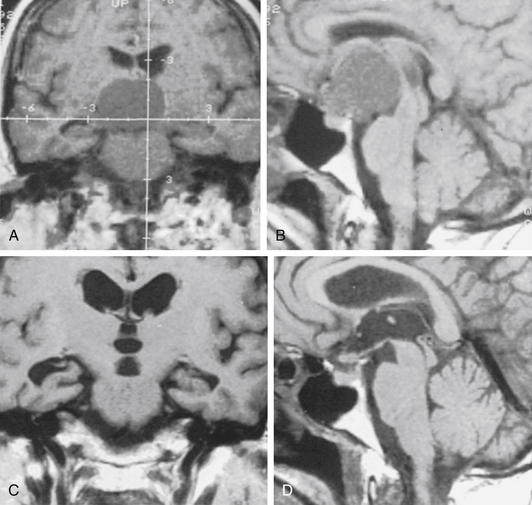
A 72-year-old woman suffered from headache, stupor, and right hemiparesis. A large left hemispheric cystic process with a midline shift was diagnosed by computed tomography (CT) and MRI examination (Fig. 26-5A and B). Using three-dimensional (3D) stereotactic trajectory and target-point calculation, the cyst membrane was approached endoscopically through a right frontal burr hole. The gray membrane was opened by radiofrequency coagulation, and biopsies were taken (Fig. 26-5C). The cyst contained CSF-like fluid. There was no evidence of tumor or other pathology. The histopathologic diagnosis was that of an epithelial cyst. The cyst was opened endoscopically to the left lateral ventricle. After surgery, the CT scan showed that the midline shift was greatly reduced. The left frontal horn was enlarged again (Fig. 26-5D). A few days after the intervention, the patient was alert and she was discharged with only a slight hemiparesis.
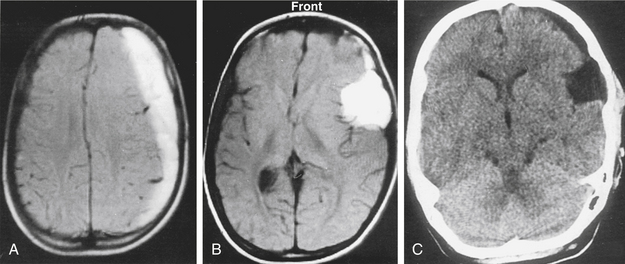
Case Report 3: Arachnoid Cyst and Chronic Subdural Hematoma
A 12-year-old boy had been hit on the head by a hockey stick. He suffered from headaches, and 2 weeks later his consciousness was impaired. MRI examination showed a left chronic subdural hematoma (Fig. 26-6A) related to a temporal arachnoid cyst (Fig. 26-6B). The subdural hematoma was drained through a silicone catheter. On CT examination, the subdural hematoma was greatly reduced with no signs of raised ICP or mass effect (Fig. 26-6C). We decided to leave the arachnoid cyst without further operative intervention. The patient did not develop complications during the postoperative course. Over a follow-up period of 9 years, the arachnoid cyst has remained.
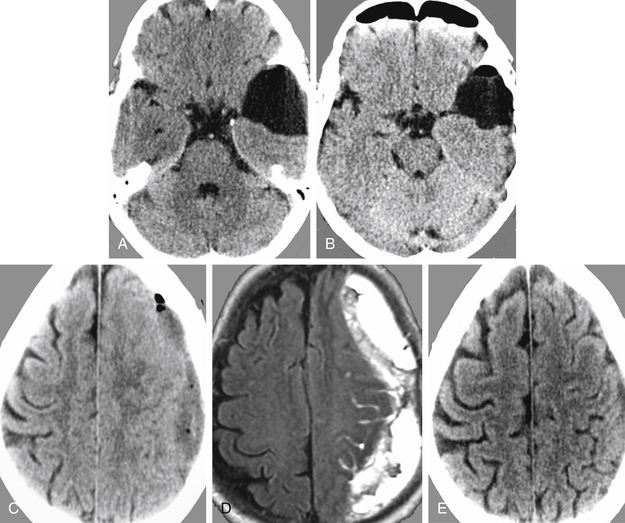
Case Report 4: Arachnoid Cyst and Postoperative Chronic Subdural Hematoma
This female patient suffered from headache, vertigo, and partial oculomotor palsy. CT demonstrated a left-sided temporal arachnoid cyst (Fig. 26-7A). Endoscopic cystocisternostomy was performed. Postoperative CT examination showed reduction of the cyst size (Fig. 26-7B), and symptoms improved. However, in the follow-up a subdural fluid collection with mass effect developed (Fig. 26-7C and D). This subdural hematoma was evacuated successfully via burr hole drainage as seen in control CT examination (Fig. 26-7E).
Neuroendoscopic Instrumentation and Operative Technique in Treatment of Arachnoid Cysts
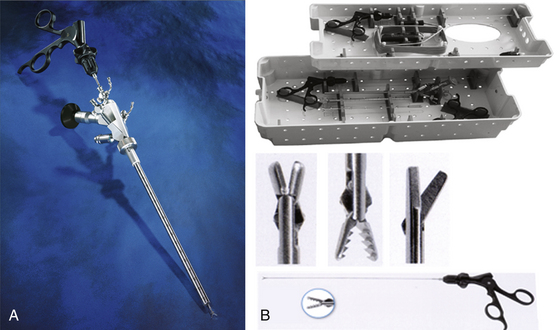
Endoscopes
Various rigid and flexible endoscopes are available to perform cystostomy, cystoventriculostomy, or cystocisternoventriculostomy (Fig. 26-8A and B). The advantages of rigid-lens scopes are the brilliant and bright pictorial quality and the guidance via a predetermined direct trajectory. Angled rigid scopes are used together with microscopes and neuronavigational devices in endoscopy-assisted microsurgery.72 They offer the possibility of looking around corners. Flexible neuroscopes have the advantages of steerability and maneuverability, which make inspection and interventions on multifocal and multiseptated cystic lesions easier.73
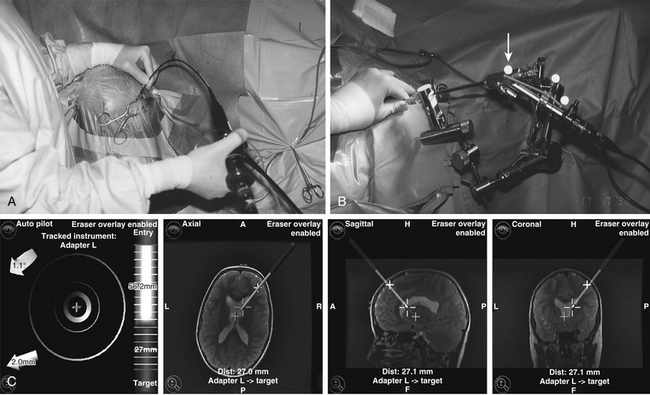
Guidance
Frame-based stereotactic guidance provides high accuracy and ensures orientation but could be time consuming and restricts endoscope movements. Standard neuronavigation systems provide image guidance, which is interactive and precise.74 These systems can be applied in a freehand mode or in combination with holding and guiding devices (Fig. 26-9A to C).
Instruments
Various instruments are available for endoscopic interventions on arachnoid cysts. Microforceps and scissors are helpful to open and resect cyst membranes (Fig. 26-10A and B). Newly developed bipolar microforceps make it possible to dissect membranes and perform hemostasis using a single instrument (Fig. 26-11).75
In many cases, it is advisable to open the arachnoid cysts using electrosurgical devices. In cooperation with Erbe Company, we have developed a bipolar cutting and coagulation microprobe, which is controlled automatically by an electrosurgical unit. The regulated energy release avoids thermal damage to vulnerable structures. Safe hemostasis is ensured by pinpoint accuracy and effective coagulation of small vessels. The cutting depth is freely adjustable up to 3 mm. The cutting needle can be retracted into the endoscope’s working channel. The probes are available for both rigid and flexible endoscopes with diameters of between 0.9 and 1.5 mm (Fig. 26-12).76 Balloon catheters (Fogarty, double balloon) are very useful to enlarge the stomas in a nontraumatic fashion.
Imaging
Intraoperative digital dynamic subtraction cystography (cystoventriculography) is performed routinely to show the communication of the arachnoid cyst to the adjoining CSF compartments and the restoration of normal CSF flow. After the endoscopic intervention postoperative electrocardiogram-gated dynamic MRI examination demonstrates the normalized CSF flow under real-time conditions. In a recently published study Hoffmann and colleagues77 could show 90% accuracy in diagnosis of communication between arachnoid cysts and neighboring CSF spaces using cine-mode MR imaging. Algin and coworkers78 compared phase-contrast (PC) cine MRI versus MR cisternography to evaluate the communication between intraventricular arachnoid cysts and neighboring cerebrospinal fluid spaces. They found that PCMRI is an effective method for evaluating noncommunicating arachnoid cysts. The results should be confirmed with MR cisternography as suspected jet flow is depicted.
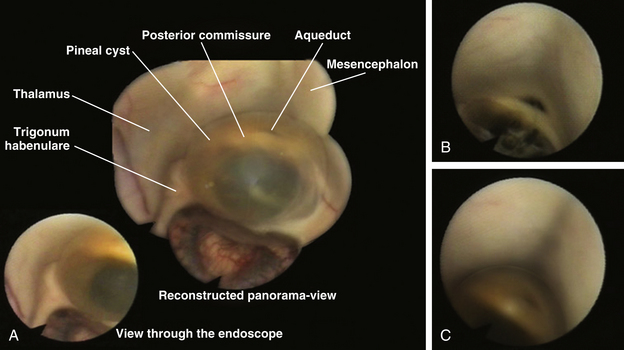
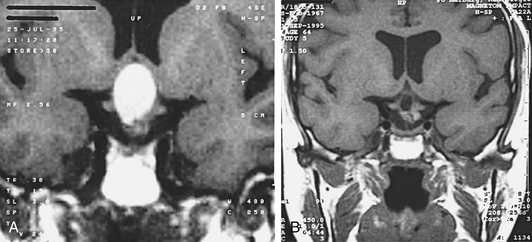
Case Report 5: Pineal Cyst
A 38-year-old female suffered from vertigo, headache, and intermittent loss of consciousness. MRI revealed an obstructive hydrocephalus due to a sylvian aqueduct obstruction caused by a cystic lesion in the posterior part of the third ventricle (Fig. 26-13A). Cystoventriculostomy was performed using the flexible, steerable endoscope (Fig. 26-13B). Fluoroscopy was used for intraoperative control (Fig. 26-13C). Postoperative MRI shows a cyst-collapse and re-establishment of CSF flow through the aqueduct (Fig. 26-13D). Fig. 26-14 shows the intraoperative findings during the operative procedure. By moving the flexible endoscope nearly the whole dorsal part of the third ventricle can be explored, as shown in Fig. 26-14A.
Suprasellar Cysts
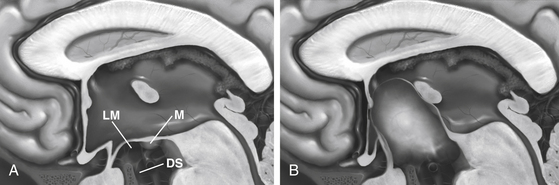
Suprasellar cysts are arachnoid cysts that occur in the sella region and become symptomatic as locally expanding lesions. Arachnoid cysts in relation to the sella turcica represent 10% of all cases.79 The term suprasellar cyst, formerly a synonym for craniopharyngioma, designates a small group of lesions, usually congenital, with a thin, even transparent wall that is filled with clear, colorless, or light-yellow fluid. The congenital effect from these cysts, which constitute fewer than 1% of all intracranial mass lesions, was severe enough to cause symptoms in the first 2 decades in 46 of the 54 reports collected by Hoffman and co-workers.80 The lesion evolves as a consequence of prevention of CSF circulation into the chiasmatic cistern or laterally from the interpeduncular cistern beneath the hypothalamus and behind the pituitary stalk and optic chiasm. The presence of CSF from below the pontine cistern then pushes the hypothalamic floor upward and thins it greatly, so that above the arachnoid dome are only at most a few glial and ependymal cells, as described by Harrison81 in three of four cases. In many of the cases, thin, even transparent, connective tissue is the only lining to the cyst. As do arachnoid cysts in other locations, suprasellar arachnoid cysts may enlarge over time. This change could be effected by active secretion of the membrane82 or from ectopic choroid-like structures14 or osmotic pressure gradients.16 Another theory for the enlargement of suprasellar arachnoid cysts is based on endoscopic and cine-mode evidence of a slit valve,1,19,20 formed by an arachnoid membrane around the basilar artery. This valve is supposed to open and close with arterial pulsations and lead to an inflow of CSF into the cyst forced by a pressure gradient.
By the time that the diagnosis is made, much or all of the third ventricle is usually filled by the cyst, causing an obstruction of one or both foramina of Monro, lateral ventricular dilatation, and a huge head. Indeed, the dome of the cyst is usually much higher than that shown in Fig. 26-15, lying just beneath the corpus callosum.
One possible mechanism for this block is excessive development of an arachnoidal curtain that extends from the posterior hypothalamus to the dorsum sellae below, originally described by Key and Retzius.83 Its presence, confirmed by Lillequist84 and by Fox and Al-Mefty,85 becomes a menace when such curtain and the arachnoid lateral to it become imperforate. Another mechanism of pathogenesis, proposed by Starkman and coworkers,86 is that intra-arachnoidal spaces in the embryo persist and expand exclusively within the arachnoid. This event was demonstrated incidentally at autopsy in a careful dissection of an intact suprasellar cyst by Krawchenko and Collins.13 Most suprasellar arachnoid cysts occur in children, with a male prevalence.2 The clinical picture often includes, in addition to hydrocephalus with a big head and ataxia, disturbed visual acuity and fields due to forward and upward displacement of the chiasm, and hypopituitarism due to pressure in the hypothalamus and pituitary stalk. These symptoms caused by a suprasellar cystic lesion had been first described by Pieter Pauw, a Dutch anatomist, in the 16th century.87
A constant forward and backward nodding of the head and neck, the bobble-head doll syndrome, is an inconstant sign.88–90 Hagebeuck and coworkers91 describe this syndrome in a 4-year-old boy, which resolved completely 3 years after endoscopic cystoventriculostomy. An unusual symptom is precocious puberty.92 Headache may occur in older patients. On CT scans, the cyst has the density of CSF; its wall shows neither enhancement nor calcification and is often mistaken for a dilated third ventricle. According to Cohen and Perneczky,2 suprasellar arachnoid cysts appear as midline round or oval hypodense lesions adjacent to the dilated frontal horns. They have a typical “Mickey Mouse” configuration on axial CT scans or MRI. Prenatal diagnosis is possible using antenatal ultrasound combined with antenatal MRI.93 Effective surgical treatment, which would seem to require simply making a big opening between the cyst and a normal CSF compartment, proves to be surprisingly difficult. Various combinations have been tried, including the transfrontal removal of the lower anterior wall of the cyst beneath the chiasm, a transcorticoventricular or transcallosal approach to remove much of the dome, the insertion of catheters between the cyst and ventricle or chiasmatic cistern, and the insertion of shunts from the lateral ventricles. Any one of these operations alone has a poor chance of sustained success. Agreement seems to be converging on the insertion of a combination of shunts from the lateral ventricles to the peritoneal cavity, with either a transcallosal route to remove the cystic dome, which was used with sustained success by Hoffman and coworkers in five cases,71 or subfrontal removal of the anterior cyst wall. This latter tactic was successful in two cases from Gonzalez and colleagues,94 three cases from Raimondi and colleagues,95 and two cases from Murali and Epstein.96 However, the lower opening closed, and symptoms recurred in one case of each of the last two groups and in one of Hoffman and co-workers’ cases. That shunts from the ventricles alone may not suffice was demonstrated in a case from Murali and Epstein, in a child in whom a neonatal shunt kept the ventricles small but who also required opening of a suprasellar cyst to control bilateral visual loss 9 years later. Ventriculoperitoneal shunting alone was satisfactory in Raimondi’s fourth case. Each of the traditional approaches has been associated with a high rate of recurrence of cysts.2
Upcoming neuroendoscopic techniques seem to solve some of the major surgical problems in treatment of suprasellar arachnoid cysts. Pierre-Khan and associates89 were the first to publish their results after performing endoscopic ventriculocystostomy of suprasellar arachnoid cysts. They used a monopolar electroprobe to create the wide stoma between the cyst and the ventricular cistern (ventriculocystostomy). In contrast to them, Caemaert and associates1 prefer to use the neodymium:yttrium aluminum garnet (Nd:YAG) laser to open the cyst to the ventricular system and the basal cisterns (ventriculocystcisternostomy). None of the patients had postoperative complications or need for a secondary shunting procedure. Additional authors have published similar successful results.2,19,97–100 Gangemi and associates11 did an extensive literature review and described the postoperative follow-up of five patients with suprasellar arachnoid cysts at their own institution after endoscopic fenestration. They found among the reviewed cases, a rate of cure or improvement of 90% (92 of 102 patients including their own cases) after endoscopy and 81% (60 among 74 cases) after other surgical procedures. The results of this study suggest that endoscopic ventricle-cyst-cisternostomy is the best treatment for suprasellar arachnoid cysts, because it is less invasive, provides the best results, and avoids shunt dependency in most cases.
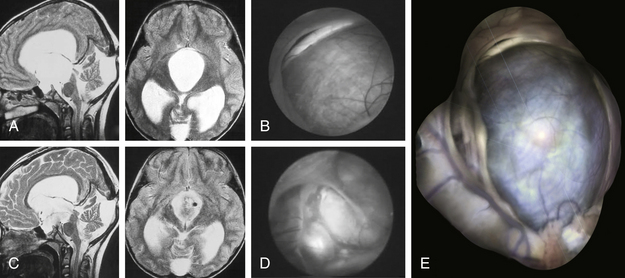
Case Report 6: Suprasellar Arachnoid Cyst
An 8-year-old girl presented with signs of raised ICP, ataxia, and a cognitive disorder. MRI showed a hydrocephalus caused by a large suprasellar cyst with brain stem compression (Fig. 26-16A). The girl was operated on with the neuroendoscopic technique using the frontal transventricular burr-hole approach. The cyst bulged into the foramen of Monro (Fig. 26-16B). After cystocisternostomy the pituitary stalk was clearly seen (Fig. 26-16D). Six days after the intervention, the girl’s clinical condition was good and she was discharged. A control MRI, taken 1 year after the intervention, shows that the cystic lesion has reduced greatly in volume, and free CSF communication existed between the ventricular system and the basal cisterns, which is documented by a postoperative MRI scan with typical flow-void signal in T2-weighted sequences (Fig. 26-16C). The girl still has no neurologic signs.
Figure 26-16E was reconstructed from different endoscopic photographs to show the entire range of the endoscopic views while moving the endoscope during the procedure.
Neuroendoscopic Technique in Treatment of Suprasellar Arachnoid Cysts
Preoperatively, it is advisable to plan the operative approach whether stereotactically or by neuronavigation. Through a frontal precoronal burr-hole approach, the surgeon enters the frontal horn of the lateral ventricle with the endoscope.74 The cyst dome is typically bulging through the foramen of Monro. Ventriculocystostomy is performed using microscissors and microforceps as well as the bipolar coagulation and cutting device. It is advisable to create a large stoma (10–15 mm in diameter). After inspection of the parasellar region, it is absolutely necessary to open the membrane of Lillequist (cystocisternostomy), which forms the inferior wall of the cyst toward the prepontine cistern, using the basilar artery as a landmark. Our bipolar coagulation and cutting electrodes prove to be the safe instruments to make bloodless openings and avoid thermal effects to the surrounding nerve tissue.75,76
Because many patients are severely impaired by the time of initial diagnosis, prompt aggressive effort and close follow-ups are required. In rare cases prepontine arachnoid cysts can disappear spontaneously as described by Dodd101 and Thomas.102
Case Report 7: Low-Grade Astrocytoma
A 62-year-old woman was admitted with a progressive bitemporal hemianopia and agitated psychosis (Karnofsky score of 30%). On MRI, a large cystic suprasellar space-occupying lesion with a blockage of foramen of Monro (Fig. 26-17A and B) was noted. Endoscopic stereotactic cyst evacuation was performed as an emergency procedure. The cystic lesion was reached through a right frontal burr hole. The gray membrane that bulged into the foramen of Monro was coagulated and was opened by microscissors. The sticky yellow contents of the cyst were aspirated. The remaining cyst membrane was vaporized using a laser. The histopathologic diagnosis was of a low-grade astrocytoma. Visual loss and the psychological disturbances of the patient normalized immediately after the procedure. A postoperative MRI showed that the cystic process was totally evacuated (Figs. 26-17C and D). The patient was discharged 12 days after the procedure (Karnofsky score of 90%).
Rathke’s Cleft Cysts
Rathke’s pouch, the superiorly directed evagination from the stomodeum of the 4-week-old human embryo, becomes obliterated at all but its cranial portion by the seventh week of gestation. The anterior wall of the remaining small cavity, “the pituitary pouch,” develops into the anterior lobe of the pituitary gland, and its posterior wall proliferates much less to become the pars intermedia of the gland. At autopsy, Shanklin103 found that a residual lumen between a portion of these two structures persisted in 22 of 100 normal pituitary glands. Small asymptomatic, fluid-containing cysts were found in 13 of these 22 specimens. Such cysts of Rathke’s cleft were recorded in 26% of routine autopsy series in five publications.104–107 Infrequently, these cysts enlarge enough to produce symptoms. These residual clefts of Rathke’s pouch are usually lined with cuboidal or columnar epithelial cells, which are often ciliated and include mucin-secreting goblet cells that stain positively by the periodic acid-Schiff method. Stratified or pseudostratified squamous epithelium may also be present and may rest on a collagenous connective tissue stroma.
By November 1989, Voelker and co-workers108 had collected a total of 155 histologically confirmed symptomatic cases from the world literature, including their own 8 cases. The increased recognition of the disorder is evident from the total of only 35 cases found in the literature in 1977 by Yoshida and associates.109 The Rathke’s cleft cyst was both intrasellar and suprasellar in 90 patients, intrasellar in 22, suprasellar in 15, and intrasphenoidal in 1. The cyst capsule varies in thickness and can be any color. Common colors of the more watery fluids are yellow, blue, or green, at times with cholesterol crystals. The content of the cyst may vary from watery or serous (in 15 cases) to mucoid, gelatinous, caseous, or motor-oil-like consistency, to white and creamy. This last appearance may be suggestive of pus. The content of one of the cysts was so tough as to require a rongeur for removal. Although in these series reported with only a few patients and a limited range of abnormal appearances may be described in CT scans and MRI,110 the extreme differences in the cystic content of protein and other chemicals are matched by similar variation in the scans, as pointed out by many authors.111–117 However, the size and location of the lesion were delineated in approximately 100% of the MRI studies and 90% of the CT scans. Image features such as a sellar epicenter, smooth contour, absence of calcification, absence of internal enhancement, and homogeneous attenuation or signal intensity within the lesion suggest the diagnosis of a Rathke’s cleft cyst.118–120 Choi et al.121 determined the differential magnetic resonance image (MRI) features of pituitary adenoma, craniopharyngioma and Rathke’s cleft cyst involving both intrasellar and suprasellar regions in 64 patients. A snowman shape and solid characteristics, and homogeneous enhancement of the solid portion were more common in pituitary adenomas. A superior lobulated shape and third ventricle compression by superior tumor extension were more common in carniopharyngiomas. Finally, an ovoid shape, a small tumor volume, cystic characteristics, and no or thin cyst wall enhancement were typical in Rathke cleft cyst. The statistically accuracies of diagnosis were as follows: 92.1% in pituitary adenoma, 92.3% in craniopharyngioma, and 92.2% overall. Kunii et al.122 described the value of single-shot, fast spin–echo, diffusion-weighted MR imaging to differentiate Rathke’s cleft cysts from other cystic lesions. Several regions of interest (ROIs) for apparent diffusion coefficient (ADC) measurements were identified in the fluid component of the lesions.
Kleinschmidt and associates123 proposed a new pathognomonic MR feature—the posterior ledge sign—of Rathke’s cleft cysts. Ross and colleagues111 stated that the diagnosis can be made at operation after the cystic cavity is irrigated. The lining of Rathke’s cleft cyst is smooth and transparent; that of a craniopharyngiomatous or a pituitary adenomatous cyst is lined at least at some point by tumor.
Case Report 8: Rathke’s Cleft Cyst
A 28-year-old patient suffering from a secondary amenorrhea was admitted to our department. An MRI scan showed a cystic lesion growing up from the sellar region and bulging into the third ventricle (Fig. 26-18A). We decided to perform primarily an endoscopic cyst evacuation using the frontal transventricular burr hole approach. The cyst was totally evacuated, and the cyst membrane was partly resected (Fig. 26-18B). The histopathologic diagnosis of the cyst membrane and its contents was ambiguous; some cells showed characteristics of craniopharyngioma cells, whereas others seemed to be of epithelial origin. Crystalloid and amorphic material was found in the contents of the cyst. The established histopathologic diagnosis was that of Rathke’s cleft cyst; the differential diagnosis was a craniopharyngioma.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree