Chapter 92 Epilepsy, Sleep, and Sleep Disorders
Abstract
Epilepsy is the third most common neurologic disorder after stroke and Alzheimer’s disease in the United States. Sleep, sleep disorders, and epilepsy are commonly associated. It is well known that sleep and sleep deprivation increase the incidence of parasomnias and seizure activity. Conversely, seizure disorders can affect the wake–sleep cycle. Sleep disorders—including parasomnias—can mimic, cause, or even be triggered by epileptic phenomena, and vice versa. A high index of suspicion and a full awareness of the broad spectrum of sleep and epileptic phenomena is instrumental to an accurate diagnosis.1
Epilepsy refers to a host of seizure disorders characterized by uncontrolled abnormal brain electrical discharges associated with undesirable motor, verbal, or experiential phenomena.2,3 These phenomena often occur during sleep.4 Electroclinical events include interictal discharges (IIDs), which are electrographically but not clinically evident, and ictal events, which are usually electrographically and clinically evident.
There are many ways of classifying seizure disorders.2 In spite of considerable diversity in etiologies and in specific ictal or IID characteristics, epileptic seizure manifestations tend to be highly state dependent. Non–rapid eye movement (NREM) sleep is associated with increased incidence and spread of IIDs; clinical accompaniment is most often associated with localization-related epilepsies originating in temporal and frontal lobes.4–6 Rapid eye movement (REM) sleep is a relatively antiepileptic state in that spread of IID is anatomically localized, and clinically evident seizures are usually suppressed.5,7,8 Arousal from NREM or REM sleep can also provoke or mimic seizures or parasomnias.9
The facilitation of sleep upon partial seizures depends in part on the location of the epileptic focus.10 The likelihood that the same basic brain circuitry generates both NREM sleep oscillations and electrical seizures with spike–wave complexes explains the close relationship between seizures and sleep.11
With the advent of neurophysiologic monitoring techniques, it has become obvious that state determination is a very complex and dynamic phenomenon involving multiple neural networks, neurotransmitters, neuropeptides, and neurohormones, as well as a myriad of sleep-promoting substances. Given these complexities, it has become clear that determining state may be inexact, with components of two or all three states occurring simultaneously or oscillating rapidly. This concept of state dissociation in animals and humans has been extensively reviewed.12
These mixed or rapidly oscillating states result in fascinating and perplexing clinical phenomena that can easily be confused with epileptic events; conversely, these sleep disorders may be perfectly imitated by epileptic events. Furthermore, other primary sleep disorders can trigger seizures, and conversely, seizures can trigger abnormal sleep phenomena. Clinically there is substantial overlap among epileptic, sleep, and psychiatric phenomena (Box 92-1).
Box 92-1
Modified from Mahowald MW, Schenck CH: Sleep disorders. In: Engel J Jr, Pedley TA, editors: Epilepsy: a comprehensive textbook. Philadelphia: Lippincott-Raven; 1997. p. 2705-2715 (with permission).
Overlap between Sleep and Epileptic Phenomena
There are five primary determinants of the quality of nighttime sleep and of daytime alertness: homeostatic (duration of prior wakefulness), circadian (biological clock influence), age, drugs, and central nervous system (CNS) pathology.13 These factors determine the overall sleep–wake pattern and also play an integral role in epileptic events.
Historical Aspects
In 1965, Gastaut and Broughton14 reported the clinical and polygraphic characteristics of sleep-related episodic phenomena in human patients. They outlined major symptoms of two major parasomnias, sleepwalking and sleep terrors. Both occur during NREM sleep, usually when the patient emerges from stage 4 NREM sleep. Prior to this study,14 these parasomnias were associated with seizure disorders. In 1968, Broughton15 questioned the pathophysiologic mechanisms underlying these paroxysmal (sudden) nocturnal events. Although parasomnias and seizure disorders exhibit common features such as abrupt onset, confusion, disorientation, and retrograde amnesia, Broughton proposed that most if not all of these episodes could be related to a disorder of arousal rather than to epilepsy.
After Broughton’s pioneering work, the concept of an arousal disorder generating parasomnias was accepted, but subsequent studies also suggest that arousal disorders can provoke, represent, or be caused by seizure disorders. Certain predisposing factors in NREM sleep seem to increase IID and ictal epileptic events.4,5 The incidence of arousal-related paroxysms, such as sleep spindles, K-complexes, bursts of slow waves, and ponto-geniculo-occipital (PGO) spikes, is closely associated with the occurrence of generalized or focal spikes, epileptiform spike-and-wave, and polyspike-and-wave in human and animal epilepsy.16,17 There is also a statistical relationship between the cyclic alternating pattern (CAP) of fluctuating cortical excitability with both epilepsy and sleep disorders.18,19
Epidemiology
There are no definitive epidemiologic studies on the coincidence of parasomnias and seizure disorders, although available studies suggest that nocturnal seizures rarely represent parasomnias.14,15,20 Symptoms of parasomnias—such as nightmares, sleep terrors, violent behavior during sleep, sleepwalking, and REM sleep behavior disorder (RBD)—resemble seizure disorders (notably partial complex seizures), thus warranting comments on reports of incidence, etiology, and clinical course.
The incidence of epilepsy has been studied most often in industrialized countries where overall population percentages are similar; available studies conducted in developing countries indicate a higher prevalence than in industrialized countries. The following statistics reflect well-conducted epidemiologic studies in the United States.21 The number of patients in the United States with a diagnosis of epilepsy is about 2.5 million, and the cumulative lifetime incidence ranges from 1.3% to 3.1% of the population by the age of 80 years. Epilepsy is the third most common neurologic disorder after stroke and Alzheimer’s disease in the United States.
Epilepsies may be categorized as generalized (40%), localization related (57%), or unclassified (3%). Localization-related epilepsies may be further subclassified as partial complex (36%), simple partial (14%), and partial unknown (7%). Localization-related epilepsies, particularly partial complex seizure disorders with tonic-clonic convulsions, are the prototypical pure sleep epilepsies; nearly 60% of these patients exhibit convulsions only during sleep.22,23 Most of these nocturnal seizure disorders are attributed to temporal or frontal lobe foci.6 Onset can occur at any time, although the average peak age at onset is in adolescence.22 Electroclinical symptoms tend to persist, and over time ictal events or IID events, or both, are likely to disperse across the sleep–wake cycle.21–23
Age at onset of parasomnias such as sleepwalking and sleep terrors is believed to be in childhood. The earlier age at onset of some parasomnias can provide one criterion for differential diagnosis from some nocturnal seizure disorders; however, many epilepsies—such as partial complex seizure disorders—do not remit spontaneously.21–24 Hereditary factors can be more prevalent in some parasomnias than in partial complex seizure disorders. Still, the most definitive criterion for differential diagnosis is polygraphic evidence of epileptic seizure discharge, and this may be difficult to obtain from surface recordings of patients with deep temporal or frontal lobe foci.25 It is likely that the rarity of nocturnal seizures manifesting as other parasomnias is more apparent than real, the correct diagnosis having been overlooked for lack of consideration.
Pathogenesis
The hypothalamic and brainstem generators of sleep and arousal have diffuse ascending and descending projections26 that give rise to a number of distinguishing physiologic characteristics called components. Components can be tonic or phasic. Tonic components are sustained background activity, such as degree of electroencephalographic (EEG) synchronization and muscle tone. Phasic components include periodic transients, such as sleep spindles, K-complexes, and muscle twitches. The association of these tonic and phasic events is important to the integrity of sleep states. Dissociation or abnormality of these components likely contributes to a variety of sleep, arousal, and seizure disorders as well as their interaction.
Direct experimental evidence using dissociative manipulations is best documented with respect to spread of EEG and clinically evident seizures that can coexist with or masquerade as parasomnias.27 Two state-specific components affecting epilepsy are the degree to which cellular discharge patterns are synchronized and alterations in antigravity muscle tone.5 NREM sleep and drowsiness differ from alert waking and REM sleep in that EEG activity is synchronized and postural muscle tone is diminished. REM sleep differs from NREM sleep in that EEG activity is desynchronized, and it differs from waking and NREM sleep in that postural muscle tone is absent. REM sleep has sometimes been called “paradoxical sleep”28 because it is characterized by a “highly active brain in a paralyzed body.”29
During NREM sleep, virtually every cell in the brain discharges synchronously, and the discharge can even reach paroxysmal levels similar to those in epileptic states.30 This occurs to a lesser extent in drowsiness. Lasting oscillations of rhythmic burst–pause firing patterns result in concerted synaptic actions. Synchronous synaptic effects, whether excitatory or inhibitory, are likely to augment the magnitude and propagation of postsynaptic responses, including epileptic discharges. During REM sleep and alert waking, cells discharge asynchronously.31 The divergent synaptic signals associated with asynchronous discharge patterns are less likely to augment the magnitude or propagation of epileptic EEG discharges.
Skeletal muscle tone also varies by sleep or waking state. Antigravity muscle tone is preserved in NREM sleep and waking,29,32 thus permitting seizure-associated and conceivably parasomnia-associated movement. Profound lower motor neuron inhibition occurs in REM sleep,29,33 creating virtual paralysis (but sparing the diaphragm to permit continued respiration). Disruption of this important component of REM sleep might underlie RBD and can influence clinically evident motor seizures.
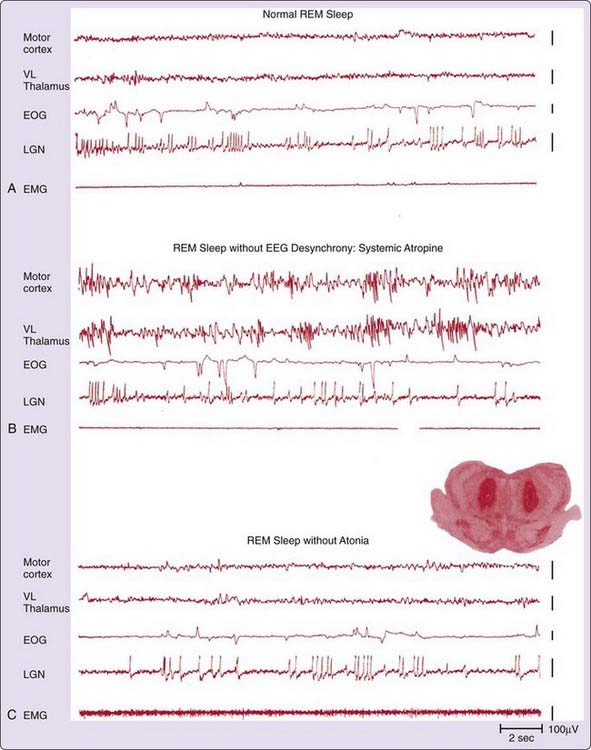
These different EEG and skeletal motor components can be experimentally dissociated, as depicted in Figure 92-1.7 Figure 92-1A shows normal feline REM sleep. Figure 92-1B shows that NREM sleeplike EEG synchrony during REM sleep can be induced by systemic administration of atropine. Although it is not shown in the figure, atropine also synchronizes the waking EEG. EEG-synchronizing effects are presumably achieved by blocking acetylcholine (ACh) release from cells in the nucleus basalis of the forebrain and pedunculopontine-peribrachial nuclei of the brainstem, because these are the critical generators of the asynchronous EEG discharges that occur in waking and to a greater extent in REM sleep.26,34 Figure 92-1C shows selective loss of postural muscle tone induced by a lesion in the pontine generators of REM sleep atonia.31 Neural generators are thought to be cholinoceptive and glutaminergic cells in the brainstem atonia regions,31,35 which hyperpolarize lower motor neurons.33
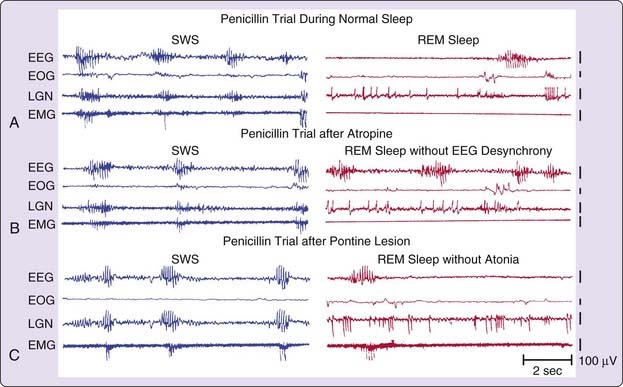
Dissociating these EEG and motor components significantly and differentially influences electrographic and clinical seizure manifestations, as illustrated in Figure 92-2. Figure 92-2A shows the distribution of penicillin-induced spike–wave complexes during intact NREM and REM sleep states. Figure 92-2B shows the effects of atropine administration. The REM sleep EEG is synchronized, and the spike–wave discharge rate is comparable with that in NREM sleep. Although it is not shown in the figure, atropine similarly synchronizes the waking EEG in conjunction with an increase in spike–wave discharge rate. Unlike waking and NREM sleep, there is no clinical manifestation during REM sleep, presumably because of the skeletal motor paralysis unique to that state. Figure 92-2C shows that a pontine lesion eliminates REM sleep atonia so that a clinically evident myoclonic seizure occurs in REM sleep.
These results are supported by other experimental and clinical findings indicating that substrates of state-specific components rather than integrity of the state per se can be salient determinants of seizure propagation. Agents that synchronize the EEG, such as cholinergic or noradrenergic antagonists, have proconvulsant effects.36–38 Conversely, agents that desynchronize the EEG discourage epileptic EEG discharge propagation. Examples are cholinergic and noradrenergic agonists39–42 as well as beta-carbolines such as abecarnil,43 which act on central benzodiazepine receptors. Finally, pharmacologic manipulations that induce atonia, such as carbachol infusion into the brainstem, also block clinical motor accompaniment.41 Consistent observations have been reported in experimental models of primary generalized epilepsy, such as electroconvulsive shock, penicillin epilepsy, and photosensitive epilepsy7,37,39; in animal models of localization-related epilepsies, such as limbic system kindling and the cortical alumina cream preparation41,44; and in the clinical literature on symptomatic generalized epilepsies such as West’s syndrome.40 Collectively, the findings confirm that cellular discharge patterns and alterations in tone affect electrographic and clinically evident seizure manifestations in diverse epileptic syndromes, including those that mimic parasomnias. There is growing evidence that glial cells play a role in epilepsy.45,46
Clinical Features
This section discusses various areas of overlap and confusion between sleep disorders and seizures. These areas include normal events, hypersomnia, insomnia, and parasomnias (see Box 92-1).
Normal Sleep Phenomena
Sleep Starts
Many healthy people experience sleep starts (hypnic jerks) during the transition from waking to sleep. The most common is the motor sleep start, a sudden jerk of all or part of the body, occasionally awakening the victim or bed partner.47,48 Variations include the visual (flashes of light, fragmentary visual hallucinations), auditory (loud bangs, snapping noises), and somesthetic (pain, floating, something flowing through the body) sleep starts, which occur without the body jerk.49–51 Sleep starts represent a normal (although not understood) physiologic event, and they should not be confused with seizures or other neurologic conditions. It is likely that the exploding head syndrome, characterized by a sensation of a loud sound like an explosion or a sensation of bursting of the head,52 is a variant of a sensory sleep start. Similar phenomena might represent the sole manifestation of a seizure.53 There is a single case report of a brainstem lesion associated with auditory sleep starts.54
Nightmares
Nightmares are frightening dreams that usually awaken the sleeper from REM sleep (see Chapter 97). Unlike disorders of arousal such as sleep terrors (see later), nightmares are not usually associated with prominent motor or vocal behavior or autonomic excitation, and the arousal results in immediate full wakefulness, with memory for the dream sequence of events that caused the awakening.55 Seizures can manifest as recurrent dreams, nightmares, or disorders of arousal such as sleepwalking and sleep terrors. The diagnosis of seizure-related dreams and nightmares may be overlooked, because the symptom is misinterpreted as a primary sleep phenomenon.56–59 Autosomal dominant frontal epilepsy can also manifest as recurrent nightmares.60
Hypersomnia
Epilepsy
The sole manifestation of nocturnal seizures may be simple arousals that may or may not be perceived by the patient. If enough arousals occur, the resulting sleep fragmentation will be apparent, with symptoms of severe excessive daytime sleepiness (Fig. 92-3). These seizure-induced arousals may be associated with very minor motor phenomena.61
Some patients with seizures are hypersomnolent during the day, even after discontinuing antiepileptic medication. Seizure-free preadolescent children with epilepsy are sleepier than healthy controls. In one study, there was no difference in objective sleepiness in children with epilepsy on or off medication, suggesting that antiepileptic drugs do not necessarily cause the daytime sleepiness.62 Excessive daytime sleepiness in a patient on antiepileptic medications must not summarily be attributed to antiepileptic medication.63–65
Narcolepsy
Narcolepsy is a genetically determined disorder characterized by excessive daytime sleepiness, cataplexy (the sudden loss of muscle tone triggered by emotionally laden events), sleep paralysis, hypnagogic hallucinations, and automatic behavior during which prolonged, complex activities may be performed without conscious awareness or recall.66,67 The spell-like nature of some sleep attacks, cataplexy, and sleep paralysis may be mistaken for seizures. Conversely, atonic (epileptic negative myoclonus) or inhibitory seizures may mimic cataplexy,68–74 and the periods of automatic behavior are often misdiagnosed as partial complex seizures, postictal confusion, or priomania.75,76 The incomplete and waxing and waning nature of cataplexy can imitate tonic–clonic seizure activity.
Periodic Hypersomnia (Kleine-Levin Syndrome)
The Kleine-Levin syndrome is a poorly understood condition characterized by recurrent periods of hypersomnia. The often-cited association with adolescent males and unusual behavior such as hypersexuality and megaphagia have been overrated.77,78 Menstruation-related periodic hypersomnia might represent a variant of the Kleine-Levin syndrome.79 Similar recurrent episodes of hypersomnia may be caused by “ictal sleep” lasting 13 days at 10- to 60-day intervals.80,81
Sleep-Disordered Breathing
There is an interesting and important relationship between sleep-disordered breathing and seizures (Video 92-1![]() ). Nocturnal seizures, probably triggered by periods of hypoxemia, may be the presenting symptom in some persons with obstructive sleep apnea or sleep-related hypoventilation.82,83 Furthermore, sleep apnea can exacerbate seizures in patients who have epilepsy that is caused by sleep disruption, sleep deprivation, hypoxemia, or decreased cerebral blood flow.84 Obstructive sleep apnea may be associated with seizure occurrence in older adults with epilepsy.85 Identification and treatment of sleep-disordered breathing in persons with seizures can improve seizure control.86,87 Some seizure-like spells associated with sleep apnea are actually caused by episodes of cerebral anoxia.88
). Nocturnal seizures, probably triggered by periods of hypoxemia, may be the presenting symptom in some persons with obstructive sleep apnea or sleep-related hypoventilation.82,83 Furthermore, sleep apnea can exacerbate seizures in patients who have epilepsy that is caused by sleep disruption, sleep deprivation, hypoxemia, or decreased cerebral blood flow.84 Obstructive sleep apnea may be associated with seizure occurrence in older adults with epilepsy.85 Identification and treatment of sleep-disordered breathing in persons with seizures can improve seizure control.86,87 Some seizure-like spells associated with sleep apnea are actually caused by episodes of cerebral anoxia.88
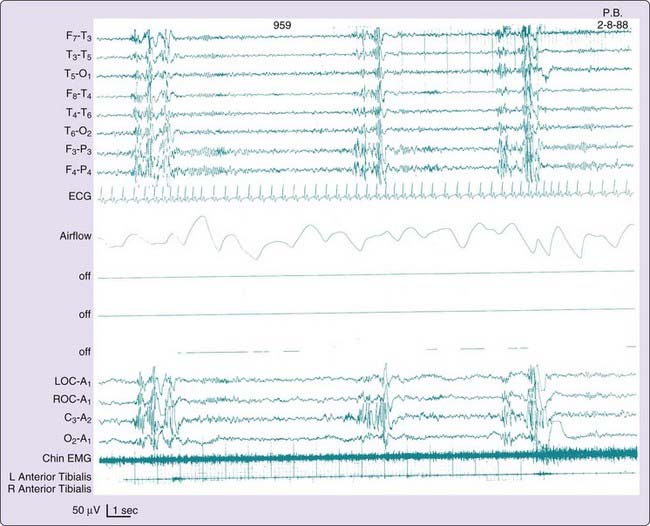
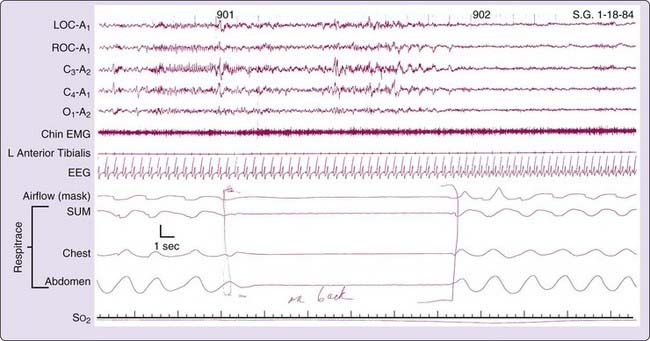
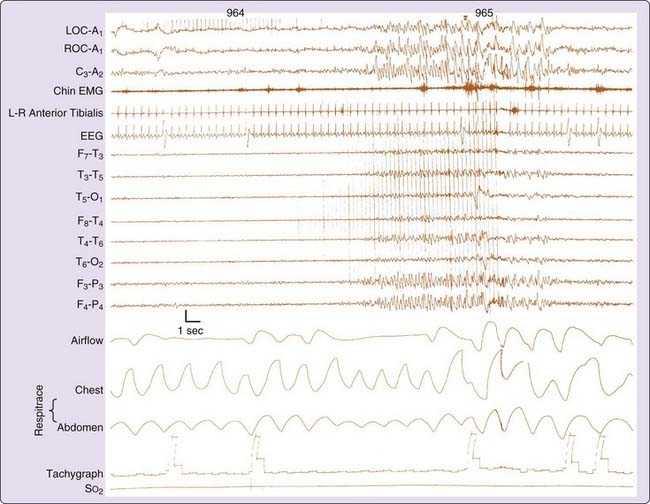
Seizures can also cause periods of apnea, often repetitive, and can closely mimic the conditions of obstructive or central sleep apnea.89–92 Figure 92-4 shows repetitive apneas as the sole manifestation of seizures, and Figure 92-5 shows obstructive sleep apnea inducing electrical seizure activity.
Insomnia
Paroxysmal, otherwise unexplained awakenings may be the sole manifestation of nocturnal seizures and result in the complaint of insomnia.93–98 Some patients with occasional paroxysmal periodic motor attacks during sleep have very frequent (every 20 to 60 seconds) subclinical arousals causing severe sleep fragmentation.99 These paroxysmal arousals may be due to deep epileptic foci.100 The arousal preceding nocturnal seizures may be the initial manifestation of the seizure.101 Animal studies support the concept of frequent arousals as the manifestation of seizures.102 This might explain why many patients with epilepsy report frequent, otherwise unexplained nocturnal awakenings.103
Parasomnias
Disorders of Arousal
Disorders of arousal are the most common and impressive of the NREM sleep parasomnias, and they may readily be confused with epileptic phenomena (see Chapter 94). These occur on a continuum ranging from confusional arousals to sleepwalking to sleep terrors.
Disorders of arousal may be difficult to differentiate from nocturnal seizures, and vice versa.104,105 Preservation of consciousness during seizures can lead to their being confused with disorders of arousal or psychogenic conditions.106 Crying (dacrystic) or laughing (gelastic) seizures may be misinterpreted as confusional arousals or sleep terrors.107,108 Both disorders of arousal and seizures may be related to the menstrual cycle.109–111
Arousals of any sort may serve to trigger a disorder of arousal. Therefore, any underlying condition resulting in arousal can cause a disorder of arousal, including sleep apnea, gastroesophageal reflux, or seizures. Thus the clinical event of a sleepwalking or sleep terror episode may, in fact, represent an epiphenomenon of a completely different underlying sleep disorder.20 It is common clinical experience to see an improvement in disorders of arousal following effective treatment of obstructive sleep apnea. Conversely, effective treatment of obstructive sleep apnea with nasal continuous positive airway pressure (CPAP) can result in disorders of arousal, presumably associated with deep NREM-sleep rebound.112,113 It must be remembered that sleep terrors and seizures can coexist in the same person.27
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree