Fig. 27.1
(a) Example of a group 1 tumor. A 58-year-old female with a left-sided cerebellopontine angle (CPA) meningioma located anterior to the inner auditory canal (IAC). (b) Illustration of a group 1 tumor displacing the facial (VII) and cochlear (VIII) nerves posteriorly (45.2 %) and compressing the trigeminal nerve (V) superiorly (59.5 %). An inferior displacement of the facial and cochlear nerves was observed in 42.9 % (not shown in illustration). Ch. Pl. choroid plexus, IX glossopharyngeal nerve, X vagus nerve, XI accessory nerve
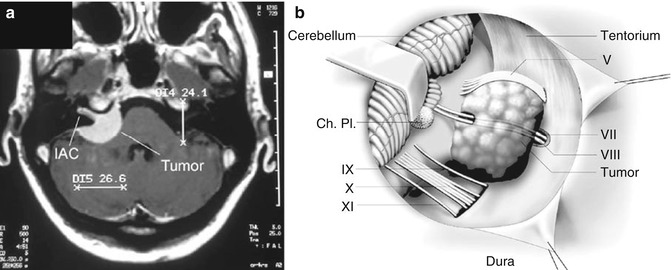
Fig. 27.2
(a) Example of a group 2 tumor. A 44-year-old female with a right-sided CPA meningioma involving the IAC. (b) Illustration of a group 2 tumor involving the IAC. The posterior wall of the IAC is removed. The tumor may either originate in the IAC or involve the IAC secondarily. The facial and cochlear nerves lie within the tumor in 29.2 % of cases. Superior or inferior displacement was observed each in 25 % (not shown). The majority of tumors (70.8 %) did not displace the trigeminal nerve, but in larger tumors, the displacement was observed mainly to the superior (16.7 %) and anterior (8.3 %) direction
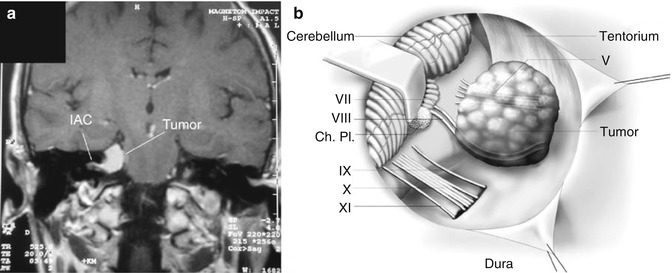
Fig. 27.3
(a) Example of a group 3 tumor. A 58-year-old female with a right-sided CPA meningioma located superior to the IAC. (b) Illustration of a group 3 tumor displacing the facial and cochlear nerves inferiorly and compressing the trigeminal nerve inferiorly. Inferior displacement of the facial and cochlear nerves was observed in 77.8 %; the trigeminal nerve was most commonly displaced inferiorly in large tumors (33.3 %)
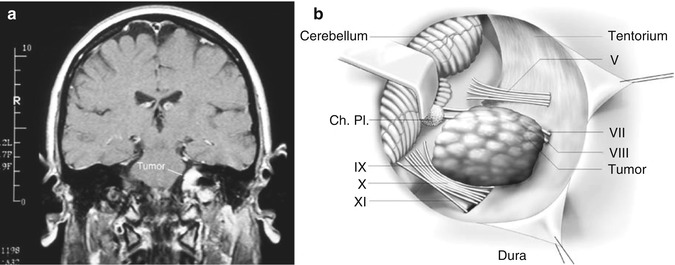
Fig. 27.4
(a) Example of a group 4 tumor. A 45-year-old female with a left-sided CPA meningioma located inferior to the IAC. (b) Illustration of a group 4 tumor displacing the facial and cochlear nerves anterosuperiorly (68.75 %) and compressing the glossopharyngeal and vagus nerves inferiorly (56.25 %)
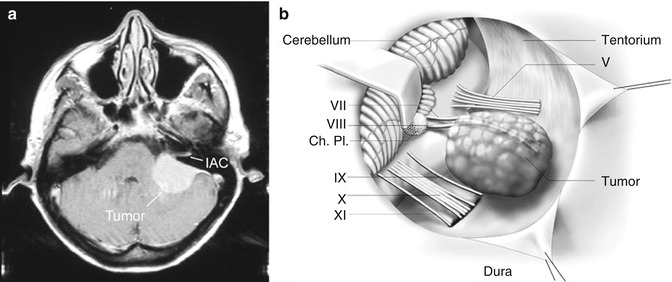
Fig. 27.5
(a) Example of a group 5 tumor. A 46-year-old female with a left-sided CPA meningioma located posterior to the IAC. (b) Illustration of a group 5 tumor displacing the facial and cochlear nerves anteriorly (62.5 %). Inferior displacement of these nerves was observed in 25 % (not shown). The glossopharyngeal and vagus nerves were displaced inferiorly in 50 % (not shown)
27.3.2 Nerve-Tumour Relationship
In any case of CPA meningiomas, the facial and cochlear nerve is displaced in distinguished directions, due to their intimate anatomic relation in the CPA. The direction of nerve displacement was depending on the site of tumour origin at the CPA.
CPA meningiomas with their origin anterior to the IAC (group 1), the facial and cochlear nerve was most commonly displaced posteriorly (45.2 %, Fig. 27.1b). Inferior displacement was observed in 42.9 % and superior displacement in 9.5 %.
The trigeminal nerve was mostly displaced superiorly (59.5 %); anterior displacement was observed in 26.2 % and inferior displacement in 14.3 %. The cranial nerves IX–XI were inferiorly displaced in only 16.7 % of cases.
The nerve-tumour relationship in CPA meningiomas involving the IAC is much less predictable. Most commonly, the facial and cochlear nerve was surrounded by the tumours (29.2 %, Fig. 27.2b). Displacement to the superior and inferior direction was observed in 25 % each. Posterior (12.5 %) and anterior (8.3 %) displacement was less common. In large tumours, the trigeminal nerve was displaced superiorly in 16.7 % of cases. Cranial nerves IX–XI were inferiorly displaced in 29.2 % of cases.
As it may be anticipated, tumours originating superior to the IAC (group 3) most commonly displaced the facial and cochlear nerve inferiorly (77.8 %, Fig. 27.3b).
An anterior displacement was observed in only 16.7 %. The trigeminal nerve was displaced inferiorly in large tumours in 33.3 % of cases (Fig. 27.3b).
Similarly, in group 4 tumours, in 68.75 %, the facial and cochlear nerve was displaced superiorly in 68.75 % (Fig. 27.4b), and anterior displacement was observed in 18.75 %. In 68.75 % of cases, the trigeminal nerve was not involved, but in large tumours, displacement was observed to the superior direction in 25 %. The cranial nerves IX–XI were inferiorly displaced in 56.25 % of cases (Fig. 27.4b).
Finally, group 5 tumours showed displacement of the facial and cochlear nerve to the anterior direction in 62.5 % (Fig. 27.5b). An inferior displacement was observed in 25 %. There was no relation to the trigeminal nerve in 87.5 % of cases, and anterior displacement was only observed in large tumours in 12.5 % of cases. The cranial nerves IX–XI were most commonly displaced to the inferior direction (50 %), and they were equally displaced anteriorly or have been surrounded by the tumours in 12.5 %.
27.3.3 Tumour Resection
Patients were most commonly operated through a lateral suboccipital retrosigmoid approach (330 patients) in the semisitting position. In tumours with significant extension to the petroclival region, a combined supra-infratentorial presigmoidal approach has been performed (17 patients). In all procedures, the intracranial part of surgery was carried out under the operating microscope.
Intraoperative neuromonitoring of the facial and the cochlear nerve was applied since 1986, and standardized protocols were routinely used since 1990 (Medelec limited, Surrey, England).
Total tumour resection, including Simpson grades 1 and 2 [36], could be achieved in 95 tumours (83.3 %) in group 1, 68 tumours (88.3 %) in group 2, 63 tumours (90 %) in group 3, 32 tumours (78 %) in group 4 and 40 tumours (88.9 %) in group 5. Altogether, 85.9 % of patients underwent complete tumour resection and 14.1 % a subtotal removal of the tumours.
The rate of total tumour resection in the subgroup of patients, who underwent surgery through the combined supra-infratentorial presigmoidal approach, was lower (70.58 %) due to tumour involvement of the cavernous sinus in five patients.
27.3.4 Complications
The most common complications, encountered after surgery of CPA meningiomas, were cerebrospinal fluid (CSF) fistula and postoperative hydrocephalus each in 4.6 % of cases. Few patients with CSF fistula required a temporary lumbar drainage (2.8 %) or a surgical revision (0.8 %). Patients with hydrocephalus were treated with temporary external ventricular drainage (3.2 %) or a ventriculo-peritoneal shunt (1.4 %).
Postoperative haemorrhage occurred in 3.5 % of patients requiring surgical evacuation in 2.6 %.
The rate of postoperative sigmoid sinus thrombosis was rare following a lateral suboccipital approach (0.3 %) but had a higher incidence after the combined supra-infratentorial presigmoid approach (5.8 %).
In this clinical series, two patients (0.6 %) died perioperatively, one due to aspiration on the third postoperative day (following a combined supra-infratentorial presigmoid approach) and the other due to a haematoma on the second day after surgery following tumour removal through the lateral suboccipital approach.
27.3.5 Facial Nerve Function
The pre- and postoperative facial nerve function was evaluated on the basis of clinical data of 334 patients.
In group 1 tumours (n = 109), most of the patients (n = 93, 85.3 %) presented initially with no facial paresis (House & Brackmann grade 1). Preoperative H&B grades 2, 3, 4 and 5/6 paresis were observed in 8.3, 2.8, 1.8 and 1.8% of patients accordingly. Both patients with preoperative complete facial palsy were already operated in an outside hospital and presented with a recurrent tumour.
In group 2 tumours involving the IAC (n = 76), 81.6 % of the patients presented with no facial nerve paresis preoperatively; 6.6 % presented with a facial nerve paresis of H&B grade 2 score, 3.9 % with H&B grade 3 score, 3.9 % with H&B grade 4 score, 2.6 % with H&B grade 5 score and 1.3 % with complete facial nerve paresis.
In group 3 tumours (n = 66), 87.9 % of patients had no preoperative facial nerve deficit; 10.6 % of patients presented with a facial nerve paresis of H&B grade 2 score and 1.5 % with a complete facial nerve palsy (after previous surgery).
In group 4 tumours (n = 39), 79.5 % of patients presented without any facial nerve deficit. 12.8 % had a mild facial nerve paresis of H&B grade 2, 5.1 % presented with H&B grade 3 score and 2.6 % with H&B grade 4 score.
In group 5 tumours (n = 44), 90.9 % of patients presented without facial nerve deficit. 9.1 % had a mild facial nerve paresis before surgery (H&B grade 2).
Comparison among groups showed that preoperative facial nerve paresis was less common in group 5 tumours (9.1 %) compared to group 4 (20.5 %) and group 2 (18.4 %), although the difference was not statistically significant (group 5 vs 4, p = 0.1397; group 5 vs group 2, p = 0.1678). The immediate postoperative result of facial nerve function in patients with preoperative good function was best in group 5 (preservation of H&B grade 1 score in 90 %) followed by group 4 (preservation of H&B grade 1 score in 87 %) and group 3 (preservation of H&B grade 1 score in 84.5 %). Preservation of preoperative good facial nerve function was less common in group 1 (76.3 % H&B grade 1 score) and in group 2 tumours (79 % H&B grade 1 score) although it was still achieved in the majority of cases (Table 27.1). The difference between group 5 and group 1 was statistically significant with p = 0.0414, and the difference between group 5 and group 2 did not reach statistical significance (p = 0.1467).
Table 27.1
Rate of functional facial nerve preservation at the same preoperative level after surgery (including improvements)
Grade | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 |
|---|---|---|---|---|---|
H&B 1 | 71/93 (76.3 %) | 49/62 (79 %) | 49/58 (84.5 %) | 27/31 (87 %) | 36/40 (90 %) |
H&B 2 | 6/9 (66.6 %) | 2/5 (40 %) | 7/7 (100 %) | 5/5 (100 %) | 4/4 (100 %) |
H&B 3 | 2/3 (66.6 %) | 0/3 (0 %) | 1/2 (50 %) |
Improvement of facial nerve function in the immediate postoperative period was observed in all four patients with group 5 tumours presenting with a mild paresis (H&B grade 2). Recovery from mild facial paresis was also observed in other groups. There was no improvement of facial nerve function in the immediate postoperative period in patients with tumours involving the IAC (group 2).
The outcome of facial nerve function depending on the surgical approach did not reveal any significant difference.
The influence of tumour size as a possible relevant factor for facial nerve outcome was examined separately. There were 149 tumours (44.6 %) with a diameter ≤3 cm and 129 patients among them had a normal preoperative facial nerve function (H&B grade 1, 86.6 %). In 82.9 % of these patients, normal facial nerve function was preserved postoperatively. A total of 185 patients had tumours >3 cm (55.4 %). Among them 155 patients had normal preoperative facial nerve function (H&B grade 1, 83.8 %). Normal facial nerve function after surgery could be achieved in 80.6 %.
Statistical comparison did not reveal any significant difference concerning facial nerve outcome between both groups (p = 0.6177).
Also the relationship between the extent of tumour resection and facial nerve function was investigated but did not show any significant difference between the patient groups with total compared to subtotal tumour resection.
27.3.6 Auditory Function
Results of pre- and postoperative auditory function based on PTA and speech discrimination tests were obtained in 333 patients.
Among 109 patients with group 1 tumours, 45 % had normal preoperative hearing (Class 1), 15.6 % presented with Class H2, 17.4 % with Class H3, 11.9 % with Class H4 hearing and 10.1 % were already deaf (Class H5).
Due to intrameatal tumour infiltration, normal preoperative hearing (Class H1) was less frequently encountered in patients harbouring group 2 tumours with only 28.9 % (22 of 76 patients). 22.4 % patients had Class H2, 18.4 % had Class H3, 7.9 % had Class 4 and 22.4 % of patients were already functionally deaf at time of surgery (Class H5).
In group 3 tumours (n = 65), 49.2 % had normal hearing (Class H1) before surgery. 18.5 % had Class H2, 15.4 % had Class 3, 4.6 % presented with Class 4 hearing and 12.3 % were already deaf before surgery.
In group 4 tumours (n = 39), 28.2 % of patients presented with normal hearing (Class H1) before surgery. 25.6 % had Class H2, 10.3 % presented each with Class H3 and H4 hearing, 25.6 % were already deaf on the affected side before surgery.
In group 5 tumours (n = 44), 47.7 % of patients presented with normal hearing (Class H1) before surgery. 22.7 % had Class H2 hearing and 15.9 % presented with Class H3 and 6.8 % with Class H4 hearing; 6.8 % patients were already deaf on the affected side before surgery.
The comparison among groups showed that normal preoperative hearing was more common in group 3 (49.2 %) and group 5 (47.7 %) compared to group 2 (28.9 %) and group 4 (28.2 %) tumours. The immediate postoperative results of auditory function in patients with preoperative normal hearing is best in groups 3 and 5 (preservation of normal hearing in 81.3 % and 81 %) followed by group 1 (preservation of normal hearing in 63.3 %) and group 4 (preservation of normal hearing in 54.5 %). Preservation of preoperative normal hearing was less common in group 2 (22.7 %) (Table 27.2). The difference between group 2 versus group 3, 5 and 1 was highly significant (p < 0.0001, p = 0.0001 and p = 0.0016).
Table 27.2




Preservation rate of auditory function on the same level after surgery (including improvements)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








