25 Facial and Trigeminal Neuropathy
Anatomy
Facial Nerve
• Motor fibers to all muscles of facial expression, as well as to the posterior belly of the digastric, stapedius, and stylohyoid muscles
• Parasympathetic motor fibers supplying the mucosa of the soft palate and the salivary and lacrimal glands
• Taste fibers to the anterior two thirds of the tongue
• Parasympathetic sensory fibers for visceral sensation from the salivary glands and the nasal and pharyngeal mucosa
• Somatic sensory fibers supplying a small part of the external auditory meatus and skin of the ear
The facial nerve, including the motor root and nervus intermedius, emerges from the brainstem at the cerebellopontine angle and enters the internal auditory meatus, next passing through the geniculate ganglion before traversing the facial canal. Within the bony facial canal, several branches arise from and leave the main facial nerve (Figure 25–1). First, parasympathetic fibers are given off to the greater and lesser petrosal nerves, bound for the pterygopalatine and otic ganglia. A small motor branch arises next, to innervate the stapedius muscle in the inner ear. The chorda tympani then arises to carry taste fibers to the anterior two thirds of the tongue and parasympathetic fibers to the submandibular and sublingual salivary glands.

FIGURE 25–1 Course of the facial motor root and nervus intermedius branches of the facial nerve in the facial canal.
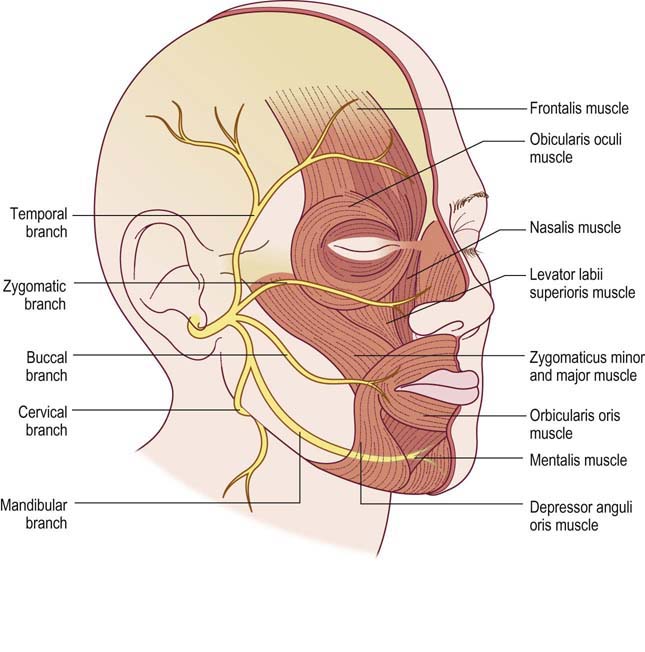
The facial nerve exits the skull at the stylomastoid foramen before coursing through the parotid gland. After the stylomastoid foramen, the nerve supplies the stylohyoid and the posterior belly of the digastric muscles, then gives off a cutaneous posterior auricular branch before dividing into its five major peripheral branches: temporal (a.k.a., frontal), zygomatic, buccal, mandibular, and cervical branches, which innervate the muscles of facial expression (Figure 25–2).
Trigeminal Nerve
The trigeminal nerve, cranial nerve V, carries sensory fibers to the face and motor fibers to the muscles of mastication. It arises from several different nuclei in the brainstem, including one motor nucleus (mid-upper pons) and three separate sensory nuclei. The sensory nuclei include the main sensory nucleus (mid-upper pons), which mediates light touch; the nucleus of the spinal tract of V (pons to upper cervical cord), which mediates pain and temperature; and the mesencephalic nucleus of V (lower midbrain), which mediates proprioception from facial muscles. Exiting from the lateral mid-pons, the nerve is called trigeminal because it branches into three major peripheral nerves that arise from the trigeminal ganglion (also known as the semilunar or gasserian ganglion), located just outside the brainstem on the petrous bone in the middle cranial fossa (Figure 25–3). The cavity formed by the folds of dura that contain the trigeminal ganglion, surrounded by cerebrospinal fluid, is known as Meckel’s Cave. Whereas the trigeminal ganglion contains cell bodies of the sensory fibers from both the main sensory nucleus and the nucleus of the spinal tract of V, the cell bodies of proprioceptive sensory fibers from muscle spindles of trigeminal motor fibers are contained within the mesencephalic nucleus of V in the midbrain.
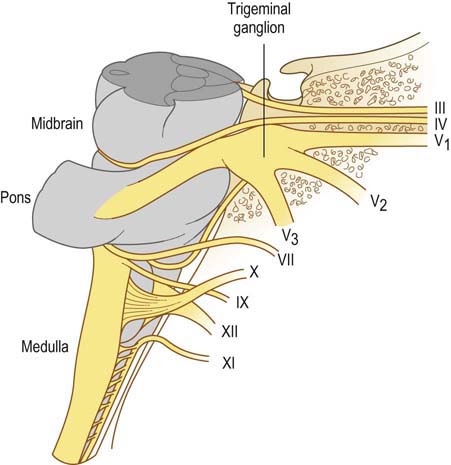
FIGURE 25–3 Trigeminal ganglion and origin of the three major peripheral nerve branches.
(Adapted with permission from Montgomery, E.B., Wall, M., Henderson, V.W., 1986. Principles of neurologic diagnosis. Little, Brown, Boston.)
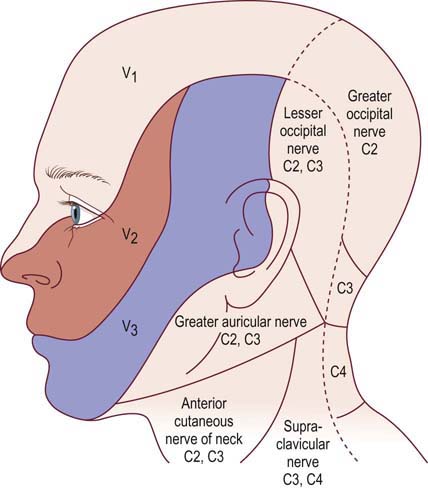
The three major peripheral nerve divisions of the trigeminal nerve are the ophthalmic (V1), maxillary (V2), and mandibular (V3) nerves. Each nerve exits the skull through a distinct opening: (1) the ophthalmic nerve through the superior orbital fissure, (2) the maxillary nerve through the foramen rotundum, and (3) the mandibular nerve through the foramen ovale. Each of the three major nerve branches contains sensory fibers, whereas motor fibers are carried solely in the mandibular nerve branches that supply innervation to the muscles of mastication (masseter, temporalis, medial, and lateral pterygoid muscles) and to the anterior belly of the digastric muscle, the mylohyoid, tensor veli palatini, and tensor tympani muscles. Branches of the trigeminal nerve supply light touch, pain, and temperature sensation to the skin of the face, the anterior half of the scalp, most of the oral and nasal mucosa, the anterior two thirds of the tongue, and the dura mater of the anterior and middle cranial fossae (Figure 25–4).
Clinical
Facial Neuropathy
Unilateral facial nerve dysfunction can also be seen in association with several disorders, most commonly in the setting of diabetes. In addition, facial palsy occurs with herpes zoster involving the geniculate ganglion (Ramsay Hunt syndrome), lymphoma, leprosy, cerebellopontine angle tumors such as acoustic neuroma, multiple sclerosis, stroke, and a host of other disorders (Box 25–1). Bilateral facial weakness is less common; it may be seen in Guillain–Barré syndrome, Lyme disease, sarcoid, Melkersson–Rosenthal syndrome, tuberculous meningitis, and leptomeningeal lymphomatosis/carcinomatosis. Bifacial weakness also is noted in some neuromuscular junction disorders and in various muscular dystrophies.
Box 25–1
Differential Diagnosis of Facial Weakness
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree