Chapter 54 Focal and Multifocal Seizures
Introduction
Focal or partial seizures originate in one region of the brain, where they may stay confined or spread to other areas. Multifocal seizures arise from multiple locations and constitute an important type of seizure in infancy and childhood. Both focal and multifocal types have been under-recognized in children, but modern epidemiologic studies show that focal epilepsies account for about 60 percent of all seizure disorders [Berg et al., 1999a,b; Sillanpaa et al., 1999]. The behavioral manifestations of focal seizures relate not only to the region of the brain involved during the ictal discharge, but also to the maturation of the nervous system and the integrity of the pathways necessary for clinical expression.
Focal seizures in the very young are subtler and less declarative than focal seizures seen later in life [Acharya et al., 1997; Hamer et al., 1999; Nordli et al., 1997]. This is particularly true in infants and children with diffuse encephalopathies, in whom brain immaturity, diffuse cerebral dysfunction, or both make manifestations of focal seizures difficult to recognize. Focal seizures also can be mistaken in older children when the presence of secondary convulsive movements prompts casual observers to label the event a “generalized tonic-clonic” seizure. With this misdiagnosis, critical elements of the seizures are overlooked. As described later, careful consideration of the unique features present in pediatric focal seizures can improve diagnostic accuracy.
In a majority of children with focal seizures, no focal structural lesion is present, and the seizures either are the expression of an idiopathic disorder (benign rolandic epilepsy) or are cryptogenic. This finding is in contrast to adults, in whom a focal seizure strongly implies the presence of a focal structural lesion (e.g., stroke, brain tumor). Instead, only 10 percent of children with focal seizures have brain tumors or strokes. In one large epidemiologic study, only 4 of 613 children with epilepsy had a brain tumor [Berg et al., 2000a].
The prognostic value of seizure classification by itself is limited, and a fuller understanding of the patient is achieved by making an epilepsy syndrome diagnosis. As pointed out in Chapter 50, two children with the same seizure type can have markedly different outcomes. Establishing an epilepsy syndrome diagnosis is the best way to determine on management options for different patients. An epilepsy syndrome diagnosis is preferred for assessing prognosis and treatment. Although it may not be possible to diagnose every child immediately on presentation, prospective population-based studies suggest that most children can ultimately be diagnosed with an epilepsy syndrome. Many factors contribute to the diagnosis of a syndrome, but in practice, three are most important:
Children with multifocal seizures (three or more foci, involving both hemispheres) may have unfavorable forms of epilepsy (e.g., migrating partial seizures, Dravet’s syndrome, symptomatic diffuse epileptogenic encephalopathies not otherwise specified). Although these epilepsies manifest with focal seizures, the children usually have evidence of concomitant diffuse cerebral dysfunction on clinical examination, developmental history, and interictal EEG studies. Correct diagnosis is particularly challenging in the group of children with focal seizures and evidence of widespread, diffuse, or multifocal cerebral dysfunction; too often, these patients end up in broad, poorly descriptive “wastebasket” categories, such as Lennox–Gastaut syndrome or generalized symptomatic epilepsy not otherwise specified. Lennox–Gastaut syndrome has particular diagnostic features and is not synonymous with diffuse symptomatic epilepsy, as discussed in Chapter 53. In summary, the importance of correctly recognizing focal seizures cannot be overstated.
Recognition of Focal Seizures in Children
Clinical features alone cannot always allow one to diagnose a focal seizure correctly. Rather, “focal seizure” is actually an electroclinical diagnosis. It usually is made following consideration of multiple factors related to the patient and the clinical event, but may require EEG confirmation, particularly in the very young. Still, a number of important clues can help point to the presence of focal seizures in children (Box 54-1). Experience using video EEG monitoring suggests that certain clinical features tend to have focal ictal EEG correlates [Nordli et al., 2001] (Figure 54-1).
Box 54-1 Seizure Semiology Indicating a Focal Seizure
 Tonic postures (particularly asymmetric tonic posture, although symmetric tonic postures also are seen in infants with focal seizures)
Tonic postures (particularly asymmetric tonic posture, although symmetric tonic postures also are seen in infants with focal seizures)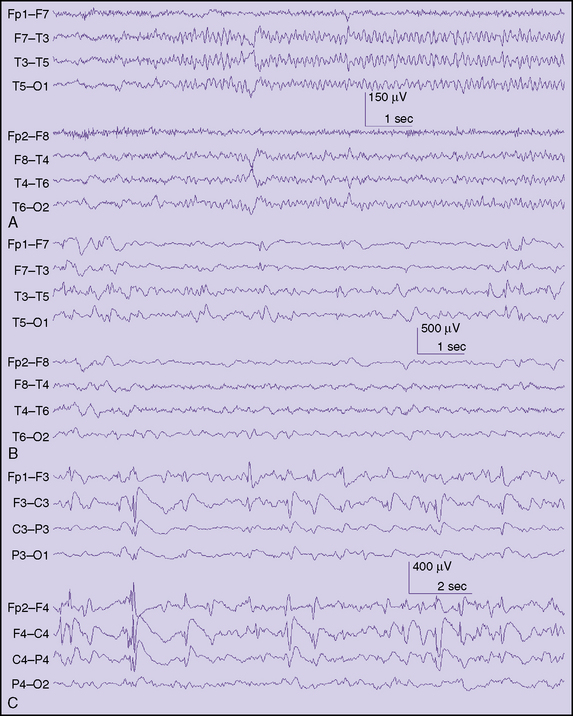
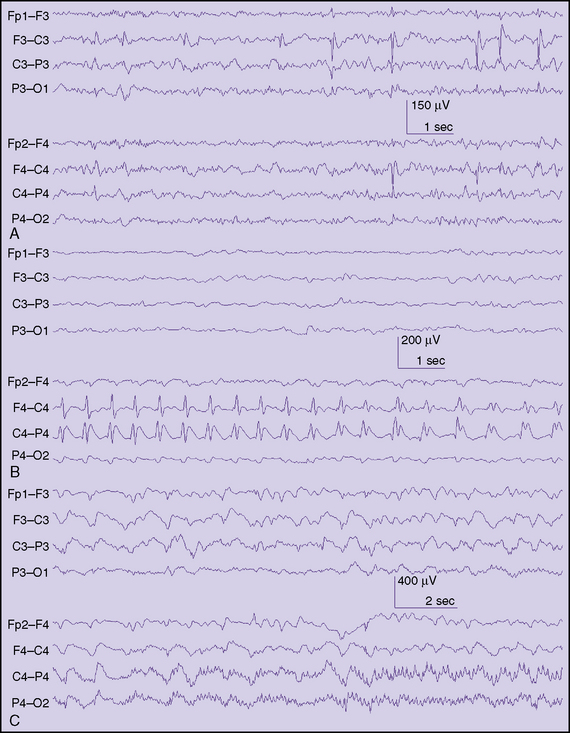
Fig. 54-1 Typical interictal findings on electroencephalogram (EEG) in children with focal seizures.
Behavioral Arrest
In some infants and young children, the most conspicuous feature of a focal seizure may be the sudden, abrupt cessation of on-going activity or a marked change in demeanor, as indicated by subtle but distinct changes in facial expression. Parents easily identify these features because they represent a clear paroxysmal alteration in the child’s behavior. Parents are particularly well attuned to the nature of their child’s habitual behavior, but these behavioral changes may be challenging for a person unacquainted with the child to identify on video tape. In the preverbal child, or in many children with special needs, it is impossible to ascertain alteration of consciousness reliably. Alteration of consciousness cannot be unambiguously inferred from behavior (e.g., daydreaming in school). To assess consciousness accurately, test items must be given and recall tested after the seizure. In children, this often is not possible, so the simple description of a behavioral arrest is more reliably used, rather than trying to infer if a seizure was truly “complex partial.” Behavioral arrest seizures also have been described as hypomotor seizures. This description refers to a sudden reduction in the motor activity of the child. The electrographic ictal accompaniment often emanates from the temporal lobe or posterior quadrant and may be composed of monotonous rhythmic delta, rhythmic theta-alpha patterns with an electrographic “crescendo” appearance, or low-voltage fast discharges that subsequently evolve to other rhythms (Figure 54-2). In children above age 3 years, behavioral arrest may accompany both focal and generalized seizures (absence seizures), so in isolation it is not a reliable indicator of a focal seizure; however, since absence seizures rarely occur in children less than 2.5 years, it is likely to be the correlate of a focal seizure in this age group.
Spasms
Spasms can be recognized by their tendency to recur in clusters, many times in an almost periodic fashion, with a fairly constant interval between some of the individual spasms. Spasms have a quick or myoclonic component at the start, followed by a brief sustained posture (tonic phase), followed in turn by a relaxation. Spasms that are asymmetric, that occur in a child with hemiparesis or other focal pathology, or that are associated with marked interhemispheric asymmetries on EEG are most likely focal seizures. In about 25 percent of patients with spasms, clear electrographic focal seizures can be detected before, during, or after the cluster. The EEG accompaniment of spasms often contains diffuse electrodecrements, even if they are preceded by clear focal seizures [Kubota et al., 1999].
Seizure Classification: International League Against Epilepsy
The International League against Epilepsy (ILAE) Commission on Classification proposed a classification of seizures in 1981. This scheme was widely used for almost three decades. Recently, a new ILAE commission on classification proposed a substantial revision [Berg et al., 2010] (Box 54-2). Now, the term “focal” replaces the previous term “partial,” and the obligatory separation of partial seizures into simple, complex, and secondary generalized has been discarded. Focal seizures still may be described further, if desired. One such way is to identify the degree of impairment. These and other descriptive terms are outlined in a previously published glossary [Blume et al., 2001] (Box 54-3). Examples of descriptors listed in the 2010 report include “without impairment of consciousness or awareness,” “with impairment of consciousness or awareness,” and “evolving to bilateral convulsive seizure.” The reader will note that these terms roughly equate to the older terms of simple, complex, and secondary generalized seizures. The important distinction is that these terms are no longer required but may be used by those who wish to maintain continuity with the 1981 classification. This adjustment appears minor, but is very useful because it is often not possible to determine alteration of consciousness reliably in the very young or in those with difficulties with communication. Lüders and colleagues have a logical and simple system that has been used internationally in major epilepsy centers (Lüders et al., 1999]. Others have proposed a much-simplified semiologic classification system for use in the very young [Nordli et al., 1997]. Neither of these schemes has been endorsed by the ILAE [Nordli et al., 1997]. While seizures may sometimes be broadly classified using the most prominent and early feature of the seizure, the various combinations of features, patterns, and time course of the seizure cannot be adequately summarized in a single word or phrase. Nothing can replace a thorough and meticulous description of the seizure. Indeed, the historic narrative of the seizure, as described or observed by parents, is the single most helpful piece of information allowing proper diagnosis of the seizure disorder and should be recorded, as accurately as possible, with few or no editorial comments.
Box 54-3 Further Descriptions of Focal Seizures
 With observable motor or autonomic components: roughly corresponds to the concept of “simple partial seizure.” “Focal motor” and “autonomic” are terms that may adequately convey this concept, depending on the seizure manifestations
With observable motor or autonomic components: roughly corresponds to the concept of “simple partial seizure.” “Focal motor” and “autonomic” are terms that may adequately convey this concept, depending on the seizure manifestations Involving subjective sensory or psychic phenomena only: corresponds to the concept of an “aura,” a term endorsed in the 2001 Glossary
Involving subjective sensory or psychic phenomena only: corresponds to the concept of an “aura,” a term endorsed in the 2001 Glossary With impairment of consciousness or awareness: roughly corresponds to the concept of “complex partial seizure.” “Dyscognitive” is a term that has been proposed for this concept [Blume et al., 2001]
With impairment of consciousness or awareness: roughly corresponds to the concept of “complex partial seizure.” “Dyscognitive” is a term that has been proposed for this concept [Blume et al., 2001]Epilepsy Syndromes with Focal Seizures
The ILAE classification of epilepsy syndromes is reviewed in Chapter 50. A recent modification of the ILAE classification eliminated the “focal” and “generalized” headings, along with the previous terms “idiopathic” and “symptomatic” (Box 54-4) [Borg et al., 2010]. One way to organize the recognized syndromes is by the specificity of the diagnostic criteria, further organized by age.
Box 54-4 Electroclinical Syndromes Categorized by Age at Onset
Neonatal Period
Benign Familial Neonatal Epilepsy
Of the three recognized epilepsy syndromes in neonates, only one has prominent focal seizures: benign familial neonatal epilepsy (BFNE). The other two syndromes, early myoclonic encephalopathy (EME) and Ohtahara’s syndrome, may have accompanying focal seizures, but the predominant seizures are myoclonic, tonic, or epileptic spasms. BFNE was first described in 1964 by Rett and Teubel [Rett and Teubel, 1964]. Before the advent of newborn video-EEG recordings, it was thought that the seizures in this syndrome might be generalized, but subsequent recordings showed that the predominant seizures are focal clonic or adversive, even though the accompanying EEG may show diffuse flattening at the onset. Ronen et al., reported the incidence as 14.4 per 100,000 live births [Ronen et al., 1999]. The clinical features have been thoroughly reviewed by Plouin [Plouin, 2008]. Most seizures (80 percent) start on the second or third day of life in term, otherwise healthy, newborns. Clinically, they usually begin with a diffuse tonic component, followed by a variety of motor and autonomic phenomena. Motor manifestations may include prominent oculofacial features, limb clonus, or both. Interictal EEG backgrounds are usually normal or may show a théta pointu alternant pattern, which consists of short bursts of rhythmic theta activity with sharply contoured components. Ictal EEGs have shown initial flattening, which may be focal or diffuse, followed by subsequent ictal rhythms. Family history, by definition, is positive and the inheritance is autosomal-dominant. Mutations in the genes encoding KCNQ2 and KCNQ3 account for the majority of cases. There are no official guidelines for treatment of BFNE and it is uncertain whether treatment is beneficial in the long run. There are clear regional preferences but phenobarbital, sodium valproate, and phenytoin have all been used. The long-term outcome is favorable, although 11 percent of patients may have epilepsy later in life [Plouin, 2008].
Infancy
Benign Nonfamilial Infantile Seizures
Fukuyama in 1963 and later Watanabe were among the first to describe infants with the onset of epilepsy in the first 2 years of life with no known cause and excellent outcome [Fukuyama, 1963; Watanabe and Okumura, 2000]. Fukuyama originally described these seizures as generalized convulsions, but this was before the advent of modern video-EEG recordings and it is likely that these were actually focal seizures with secondary spread. Watanabe and colleagues described a case series in 1987 and noted clear focal features, describing these seizures as “complex partial” [Watanabe and Okumura, 2000]. Whether these are two separate conditions or one syndrome is a matter of some debate. In both cases, there is normal development before the onset of seizures. Imaging studies and metabolic tests are unremarkable. Onset is mostly within the first year of life in both cases. The interictal EEG is normal. In both cases, seizures may manifest with blank staring, and may be followed by secondary generalization in the Fukuyama type. Seizures may occur in clusters in both. The ictal focus is most often in the temporal region in the Watanabe form and in the centroparietal region in the Fukuyama type. Both demonstrate an excellent response to treatment and have normal development. Capovilla and colleagues have described another infantile epilepsy with excellent outcome. These infants have focal seizures and a characteristic interictal EEG finding of a “bell-shaped” discharge, which is maximal at the vertex [Capovilla and Vigevano, 2001]. Infants present between 8 and 30 months with relatively bland seizures characterized by motion arrest, some tonic stiffening, and oxygen desaturation. Seizures are infrequent and usually of short duration. The authors did not recommend treatment with antiepileptic drugs (AEDs) in most cases. A family history of epilepsy is present in half the cases and the outcome is very favorable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree