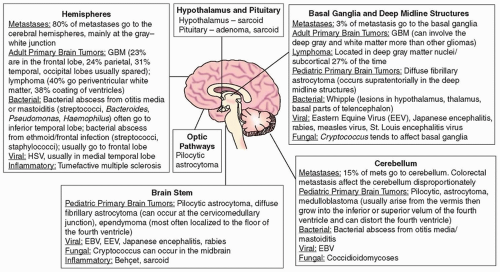
|
Clinical Pearls |
Imaging Features |
CSF Studies and Systemic Workup |
Metastatic tumors (in order of decreasing frequency) |
Lung
Breast
Melanoma
Renal
Colorectal
|
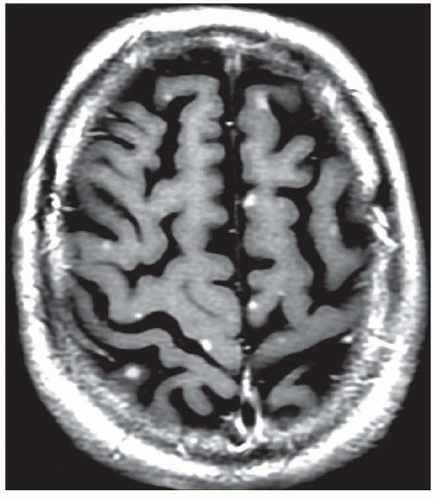
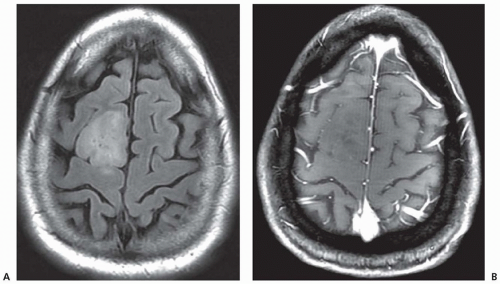
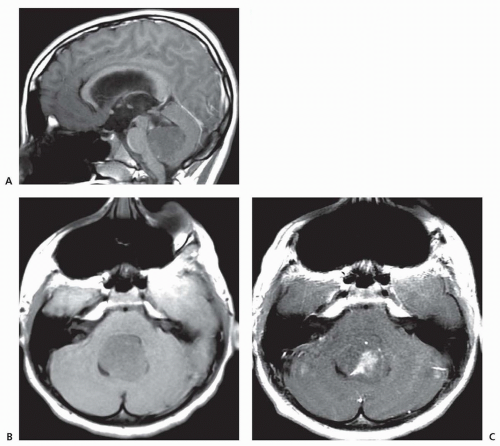
80% of brain metastases occur in the cerebral hemispheres, 15% in the cerebellum, and 5% in the basal ganglia.
Metastases tend to localize to the gray-white junction location and the border zone between two major arterial distributions.
Brain metastases are multiple, approximately 50% of cases.
FLAIR imaging tends to reveal a large amount of associated vasogenic edema.
MR spectroscopy shows low N-acetylaspartate (NAA) and creatine levels and elevated choline levels reflecting cell membrane and myelin turnover.
Gradient echo or SWI may demonstrate hemosiderin deposits in cancers that tend to hemorrhage (e.g., melanoma, choriocarcinoma, renal cell, and thyroid cancer). Melanoma tends to be hyperdense on CT scan even in the absence of hemorrhage. On MRI, melanoma is hyperintense on T1 and hypointense on T2.
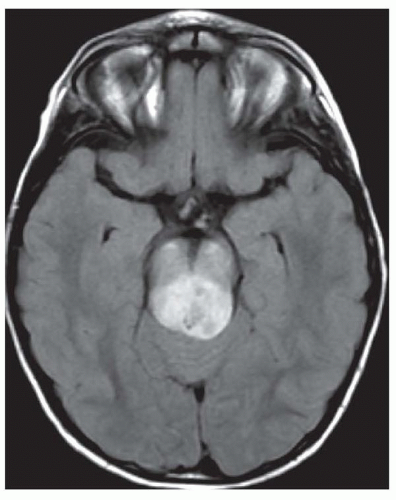
Colorectal metastases involve the cerebellum disproportionately.
|
More than 60% of patients with brain metastases will have a mass demonstrated on chest imaging that is either due to a primary lung cancer or lung metastases from a primary tumor elsewhere.
Tests to consider when brain metastases are suspected:
Mammogram
Skin exam
Whole-body CT
Whole-body FDG-PET
|
Meningoma |
35% of all primary brain tumors
67% of cases occur in women
Peak incidence, age 40-60 yr
|
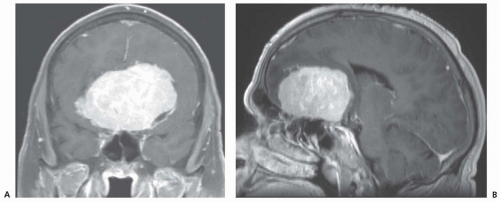
Dural based with dense, homogeneous enhancement
Anatomic predilection in order of frequency
Parasagittal
Convexity
Sphenoid ridge
Cerebellopontine angle
Olfactory groove
Can elicit a bony reaction leading to hyperostosis of the overlying calvarium
Calcification occurs in approximately 20% of cases. |
None |
Gliomas |
|
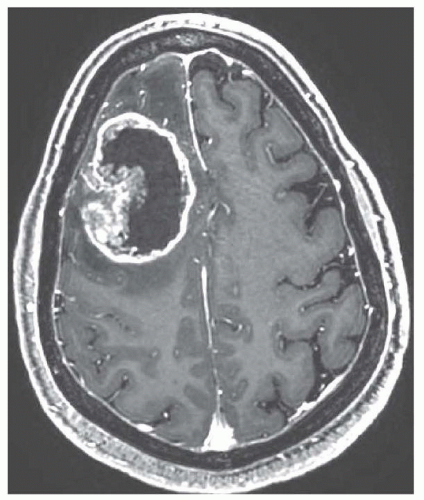
Glioblastoma (GBM)
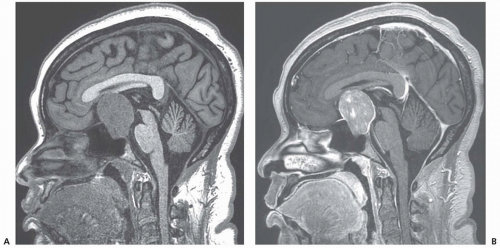
Causes extensive edema in the deep white matter
Enhances with gadolinium
Central areas of necrosis restrict on DWI (bright)
May have satellite lesions
Tumor often crosses the corpus callosum and anterior commissure.
MR spectroscopy: Cho/NAA ratio >2.2 is thought to be high grade.
Anaplastic astrocytoma
Oligodendroglioma
40%-80% rate of calcification
Enhances in 50%-70%
Hemorrhage or cyst formation occurs in 20%.
Usually, there is little edema.
|
Order lower extremity Doppler in patients with GBM. Ultimately, up to 25% of these patients suffer from venous thromboembolism during the first year of diagnosis. |
Pituitary adenoma |
10% of all primary brain tumors
Classified as secretory (75%) and nonsecretory (25%)
Prolactinoma
Growth-hormone-producing tumor:
Adrenocorticotropic hormone (ACTH)-producing tumors
Thyroid-stimulating hormone (TSH)-producing tumors:
|
Tends to be hypodense on CT
Microadenomas are generally hypointense on T1 and variable intensity on T2.
Adenomas do not enhance as much, and enhance later, than normal pituitary tissue. Dynamic contrast-enhanced MRI scans are best of delineate adenomas.
Macroadenoma are adenomas >10 mm. They have a propensity for hemorrhage and infarction (pituitary apoplexy).
Differential diagnosis:
|
Pituitary hormone panel
Serum and 24-h urine cortisol levels
TSH and T3/T4 levels
Growth hormone
Formal visual field testing and ophthalmologic evaluation are critical.
Serum prolactin >200 µg/L with an adenoma >10 mm in size is diagnostic of a prolactinoma. |
Primary central nervous system lymphoma (PCNSL) |
Causes <5% of all primary brain tumors
Immunocompromised state (e.g., HIV, transplant) is a major risk factor.
Among immunocompetent patients, the mean age of onset is 60 yr and there is a slight male predominance.
|
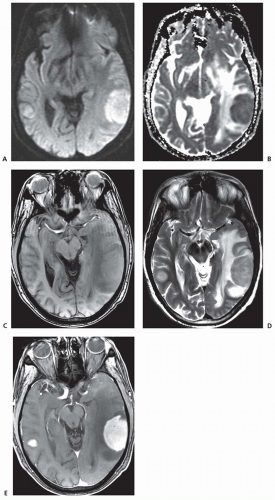
Tends to be hypodense on CT
MRI features
Anatomic predilection
Periventricular white matter in 40%
Coating of ventricles in 40%
Deep gray matter nuclei/subcortical in 30%
Unusual multifocal distribution of tumor can occur.
Diffusely enhancing in the immunocompetent patients; necrotic center can occur in immunocompromised patients.
Spread across corpus callosum is suggestive of PCNSL.
Masses tend to be <2 cm in patients with AIDS and >2 cm in non-AIDS patients. |
Slit lamp examination reveals intraocular involvement in 15% of patients. |
CSF, cerebrospinal fluid; FLAIR, fluid-attenuated inversion recovery; MR, magnetic resonance; SWI, susceptibility-weighted imaging; CT, computed tomography; MRI, magnetic resonance imaging; FDG-PET, 18F-fluorodeoxyglucose positron emission tomography; DWI, diffusion-weighted imaging; FSH, follicle-stimulating hormone; LH, luteinizing hormone. |