Fig. 42.1
Anatomical preparation of the posterior facet complex, disc, and exiting nerve root
The proper position of the working cannulas on the posterolateral or posterior annulus is essential for adequate access and successful performance of full-endoscopic discectomy, and the skin entry point can be measured in the preop MRI [5]. For the posterolateral approach a line drawn from the skin to the center of the disc is transferred to the mediolateral distance and is between 8 and 12 cm. For the lateral approach the skin entry corresponds, in the lateral fluoroscopic view, to the posterior margin of the facet complex, between 15 and 18 cm lateral the midline (Fig. 42.2).
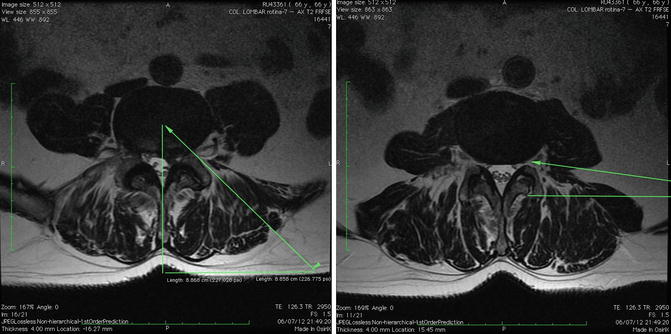
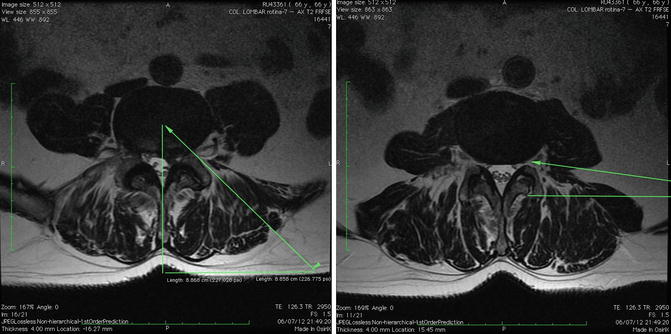
Fig. 42.2
Measured in the preop MRI of the skin entry point for posterolateral and lateral approaches
Although for the interlaminar approach we use the same anatomical corridor as for conventional microdiscectomy, we do not need to detach the multifidus muscle from the midline, and when the ligamentum flavum is incised, the opening can be limited to a maximum of 5 mm to insert the endoscope with minimization of operation-induced traumatization and its consecutive sequelae.
To treat surgically cervical compression pathologies, since the spinal cord may not be manipulated, full-endoscopic posterior decompression can only be performed in lateral localized pathologies and can be applied to foraminal radicular compression due to disc herniation and/or osteophyte compression.
The removal of extruded disc material and/or dilation of the foramen corresponds to direct decompression.
42.2 The Posterolateral and Extreme-Lateral Approach
This technique can be done with conscious sedation and local anesthesia which allows continuous feedback from the patient during the entire procedure to avoid causing damage to neural structures with the patient in the prone position on a radiolucent table and guidance of c-arm fluoroscope (Fig. 42.3).


Fig. 42.3
Patient with conscious sedation and prone position on a radiolucent table
In using this technique we can approach from inside the disc at the base of the herniation and perform a fragmentectomy without manipulation of the nerve root or using an extraforaminal approach, decompressing the nerve root directly without removing the yellow ligament. The anatomical basis of the approach is the safe triangle of Kambin [2] and the posterolateral and extreme-lateral approach and with identification of the anatomical structures, the transverse root, the exiting root, and the disc.
The skin entry point is between 8 and 16 cm lateral from the midline, targeting the safe triangle in the auxiliary area between exiting and transversing roots in the medial pedicular line in the AP view and the posterior vertebral line in the lateral view (Fig. 42.4).
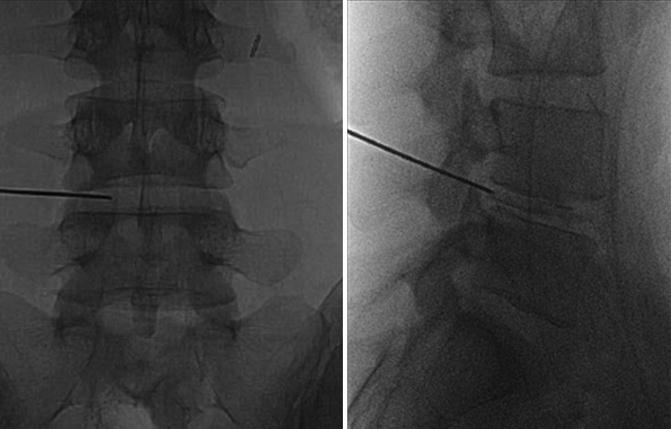
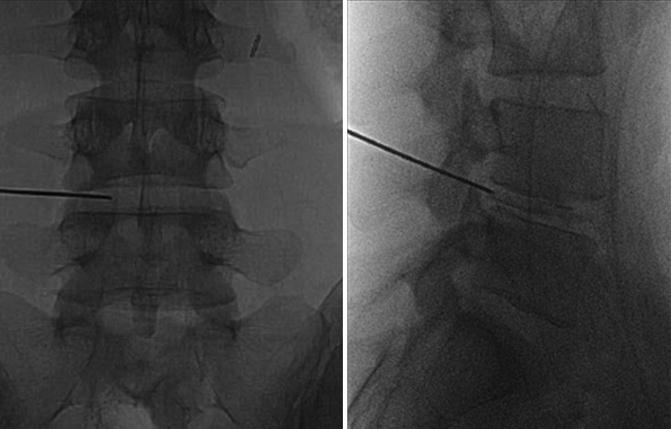
Fig. 42.4
The percutaneous lumbar disc entry point with the spinal needle for L4/L5
After entering the disc with the needle, it is replaced with the guide wire and the dilating obturator. The next step is annular fenestration and sliding a beveled working cannula in a twisting motion until it reaches the deepest part of the annulus (Fig. 42.5).
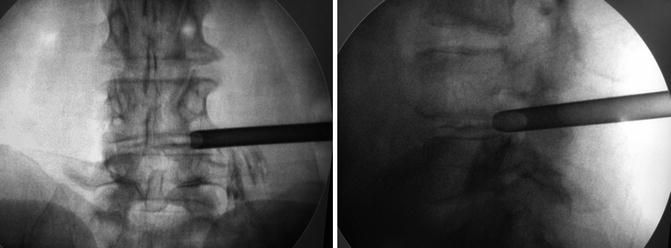
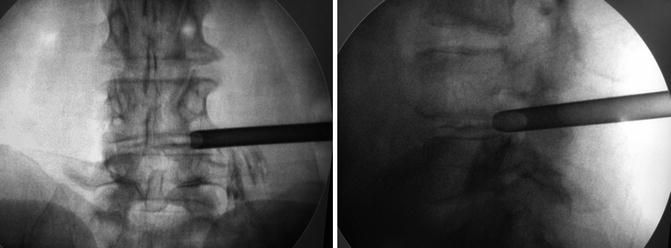
Fig. 42.5
Beveled working cannula in place for L4/L5
Now, we can insert the endoscope with the view of the disc and the epidural space and the herniation and the epidural space (Fig. 42.6).










