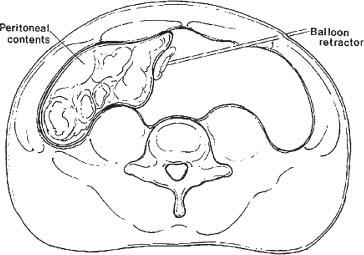
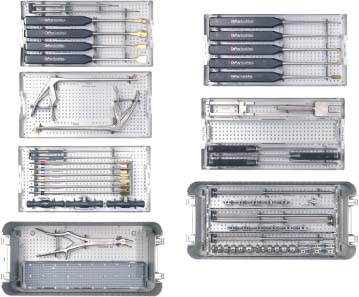
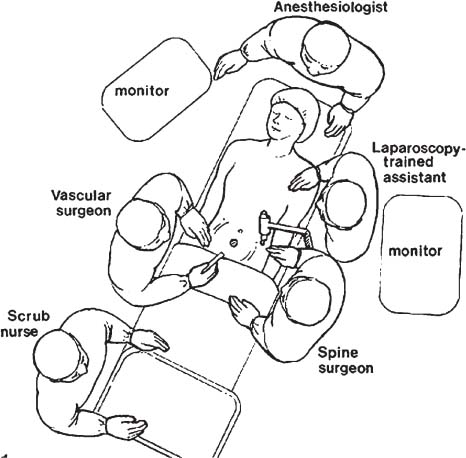
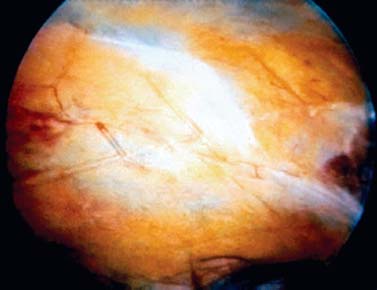
The evolution of endoscopic anterior lumbar interbody fusion (ALIF) began with the first laparoscopic diskectomy performed by Obenchain.1 From that, a combination of vascular surgeons and anterior lumbar spine surgeons developed the gas-mediated laparoscopic approach for ALIF.2–7 For a brief window in time, this approach was the gold standard for minimally invasive access to the anterior lumbar column. This would not have occurred had it not been for the introduction of small cylindrical fusion cages because cylindrical cages were the only interbody fusion implant that could fit through the ports at that point in time. Despite the fact that the gas-mediated approach was well publicized, it is not without its drawbacks. Access above L5–S1 is severely limited. Access to L4–L5 is possible in some cases, but mobilization of the vessels at L4–L5, as well as bowel retraction, is extremely difficult. The approach requires the use of long, thin instruments due to the small size of the valved ports. These endoscopic instruments have fulcrums that are too far from the surgical field, which creates an unnatural operative technique, compared with open anterior lumbar surgery. There are also issues concerning the maintenance of the pneumoperitoneum because suction often eliminates gas from the abdominal cavity faster than the insufflator can supply it. This causes an undesirable loss of exposure. Because of these limiting problems with the gas-mediated approach, a gasless approach, balloon-assisted endoscopic retroperitoneal gasless (BERG), was developed as the next step in minimally invasive anterior lumbar surgery.8–9 The BERG approach utilizes a balloon to perform the initial dissection followed by a combination of a mechanical lifting arm and fan retractor to distend the abdomen without the use of gas insufflation. This is a true retroperitoneal approach to the anterior lumbar column, which allows for access up to L2 and in some cases up to L1. Because there are no pressurized ports with this approach, the surgeon can use standard anterior instruments for lumbar fusion surgery. There is no pneumoperitoneum to maintain, so loss of exposure due to suction is not a problem. Vascular and bowel retraction is similar to an open anterior retroperitoneal approach. Indications By definition, BERG is a retroperitoneal approach to the anterior lumbar spine. Indications for the BERG approach are exactly the same as they are for the open retroperitoneal approach: Non-ALIF Indications Indications for the non-ALIF approach are The BERG approach has no absolute contraindications, although there are some relative contraindications. It is the role of the vascular surgeon to examine the physical health and surgical history of the patient closely prior to surgery. The vascular surgeon should have strong input as to whether or not to attempt a BERG approach with a contraindicated patient. Contraindications include Surgical Equipment The following instruments and equipment are necessary to perform the BERG approach to ALIF properly: FIGURE 28–1 The mechanical lifting arm is used to lift the fan retractor and distend the abdominal wall. FIGURE 28–2 The fan retractor is used to distend the abdominal wall. FIGURE 28–3 The balloon retractor is used to retract the peritoneal contents to the right. FIGURE 28–4 A standard set of instruments for anterior lumbar surgery. Operating Room Setup The spinal surgeon stands on the left side of the patient; the vascular surgeon stands on the right. Video monitors are aligned and angled next to each surgeon, providing cross-table visualization. An endocopically trained technician stands to the right of the spinal surgeon and operates the endoscope following exposure (Fig. 28–5). FIGURE 28–5 The operating room setup for the BERG approach. Patient Positioning The patient is placed in the supine position. Following general anesthesia, the patient is draped and prepped in standard fashion, and preoperative antibiotics are given. Fluoroscopy is used to find the landmarks of the appropriate lumbar level. The skin is marked, identifying the level and angle of the pathologic disk interspace(s). These are drawn on the lateral aspect of the left abdomen, marking the angles of the disk spaces to be addressed (Fig. 28–6). Surgical Technique A transverse, 20 mm left flank incision is made ~1 cm above the left iliac crest in the midaxillary line (Fig. 28–7). The dissection is taken down through the external oblique, internal oblique, and transversus muscles under direct vision to the preperitoneal fat layer using a clearended, endoscopic dissecting port. As the preperitoneal fat layer is penetrated by the clear-ended dissecting port, there is a color change to yellow, which lets the surgical team know that layer has been reached and that they should proceed with caution. FIGURE 28–6 Preoperative markings on the abdomen demonstrating the angle and location of the interdiscal segments. The retroperitoneal space is then gently insufflated with a bulb syringe and digitally dissected into the iliac fossa to allow for balloon insertion. An undeployed elliptical-shaped preperitoneal balloon is advanced through the incision until the entire balloon is within the retroperitoneal space. A 0-degree angled endoscope is placed through the lumen of the dissection cannula, and the balloon is expanded to an approximate volume of 1 L. The endoscope is directed toward the anterior abdominal wall. This allows the identification of the peritoneal reflection on the anterior abdominal wall, at the rectus sheath, above and below the line of Douglas (Fig. 28–8). The peritoneal reflection is used as a landmark for the anterior working port. The anterior working port is located lateral to the peritoneal reflection on the rectus sheath. This port is formed at a level determined by the preoperative markings on the abdomen, which correspond to the interspace angulation. A 2 to 3 cm paramedian incision is made through the anterior abdominal wall and carried down through the fascia. This is done lateral to the peritoneal reflection and with great care to avoid the peritoneal sac. This creates the anterior working/retraction port. The balloon is removed after a 1 cm malleable retractor is placed between the two ports under direct endoscopic vision. Once the retroperitoneal space has been mobilized, the next goal is the retraction of the abdominal wall. FIGURE 28–7 The initial left flank incision. This will become the area of abdominal distention as well as the port for the endoscope and the balloon retractor used to retract the peritoneal contents. FIGURE 28–8 Direct endoscopic view through the balloon at the peritoneal reflection, used as a landmark to create the anterior working port. There are three levels of retraction necessary to access the anterior lumbar spine. The first of these is distraction of the anterior abdominal wall. This is accomplished by the insertion of a fan retractor into the initial flank port. The fan retractor is expanded under direct endoscopic vision. Once expanded, the fan retractor is attached to a mechanical lifting arm. The abdominal wall is elevated by this combination, creating the retroperitoneal space and replacing the need for gas. A flexible nonvalved port, utilized for lateral visualization and retraction, is placed directly below the legs of the fan retractor to provide a clear path for the endoscope. The second level of retraction is necessary to displace the peritoneal contents past the midline to provide access to the lumbar spine and vascular anatomy. A long retractor with an inflatable end is inserted through the newly created lateral working port in the initial left flank incision to push the peritoneal sac and intra-abdominal contents aside, creating the working space (Fig. 28–9). Once the retractor is in place, the technician stands with his or her abdomen against the retractor handle, leaving two hands free for endoscope operation, cleaning, and so on. FIGURE 28–9 The entire setup for the approach with fan retractor and lifting arm to the right, endoscope and balloon retractor in place within the left flank incision, and anterior working port to the left. The third level of retraction is vascular. Following establishment of the operative cavity, the psoas muscle and vascular anatomy are used as reference landmarks. The psoas muscle is bluntly dissected to expose the pathologic disk space(s). The L5–S1 vascular retraction begins by identifying the right iliac vein and utilizing a vascular retractor to retract the fascia and presacral veins, thereby exposing the anterior aspect of the L5–S1 interspace. Through the visualization/retraction port, a standard vein retractor is passed and is used to retract the iliac vein laterally. Once this is done, the presacral veins are ligated or cauterized with bipolar cautery if necessary. Great care must be used in dissecting the anterior soft tissues to maintain the integrity of the presacral plexus. The L4–L5 exposure is more complex. It begins by using an anterior vessel retractor and displacing the vena cava or left iliac vein. This is placed on tension, and the iliolumbar vein is identified. If necessary, the iliolumbar vein is ligated using corporeal knot tying. This is generally reinforced with two specific ligatures. Once the iliolumbar vein is ligated, gentle dissection is used to retract the left iliac vein, exposing the L4–L5 interspace past the midline. The vascular retraction for L3–L4 is performed in a similar way, but it does not require ligation of the iliolumbar vein. Following psoas dissection and vessel retraction, a spinal needle is placed into the pathologic disk(s), and fluoroscopy is used to confirm the operative level. The anterior working port allows for both vascular retraction and the introduction of such standard spinal instruments as dissectors, rongeurs, curettes, and end-plate elevators. Our experience with the BERG approach has been primarily with ALIF. The technique for ALIF is essentially the same as it is with an open anterior retroperitoneal approach. Diskectomy begins by incising the anterior anulus with a long-handled scalpel, both cranially and caudally, as well as left and right. End-plate elevators, rongeurs, and curettes are introduced and utilized through the anterior working port. Once the disk is removed, the surgical team has several options for fusion (e.g., anatomical cages, screw-in cages, allograft, and autograft). After the allograft, disk prosthesis, or cage is placed, the option of buttress plate fixation is possible. Following this, the implant position is confirmed through fluoroscopy. Upon satisfactory imaging, the retroperitoneum is inspected, and the three levels of retraction are removed. The incision is closed in layers in standard fashion. Postoperative Care Patients undergoing stand-alone ALIF or circumferential minimally invasive instrumented fusion are discharged from the hospital at 1 to 3 days postoperatively. Patients are placed in a neoprene lumbar corset for at least 4 weeks postoperatively. They begin aquatic physical therapy at 10 to 14 days postoperatively and advance to weight training, treadmill, and range-of-motion therapy as tolerated. Return to work depends largely on the patient’s motivation and occupational circumstances (Fig. 28–10). FIGURE 28–10 Lateral radiograph at 2 years postoperatively of a 30-year-old male presenting with failed laminectomy syndrome and mild degenerative disk disease at L4–L5. He had an ALIF with femoral ring allograft via BERG and minimally invasive posterolateral instrumented fusion. The patient was discharged within the following day and returned to work at 2 months postoperatively. He has a solid fusion radiographically. (A) AP x-ray. (B) Lateral x-ray. All of these postoperative complications are known to occur with anterior lumbar surgery, and the BERG approach is no exception. Balloon-assisted endoscopic retroperitoneal gasless is a true retroperitoneal approach to the anterior lumbar column. Indications for the BERG approach are exactly the same as they are for an open retroperitoneal approach. Because there are no pressurized ports with this approach and no pneumoperitoneum to maintain, the surgeon can use standard anterior instruments for lumbar fusion surgery. To minimize complications, the BERG approach should be performed in conjunction with a vascular surgeon. REFERENCES
28

Gasless Endoscopic ALIF: The BERG Approach






< div class='tao-gold-member'>
Gasless Endoscopic ALIF: The BERG Approach
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








