Global Burden of Neurologic Disease
Jennifer Sevush-Garcy
Mitchell S. V. Elkind
INTRODUCTION
Neurologic disorders are globally among the most important causes of human illness and mortality. Quantifying the burden of neurologic disease and its impact on populations throughout the world is challenging for several reasons, however. First, neurologic disease includes disorders that primarily affect the brain as well as diseases that affect other body systems but have prominent neurologic manifestations. Second, neurologic diseases are notable for more frequently causing disability than death. Commonly used measures of disease impact, such as hospitalization or mortality rates, may not capture the impact of nonfatal neurologic problems such as migraine or epilepsy. Third, there are often disparities in neurologic disorders caused by socioeconomic and geographic factors. Assessment and diagnosis of neurologic disease may also depend on resources available for their measurement that are not available in all environments. Despite these limitations, present estimates of the burden of neurologic disorders suggest that they have an enormous impact on human health.
THE CLASSIFICATION OF DISEASE: WHAT IS A NEUROLOGIC DISORDER?
The classification of neurologic disorders can be broken down into two general categories: primary neurologic disorders affecting the nervous system only and secondary neurologic disorders, in which injury or dysfunction of the nervous system occurs as a result of a disease that primarily affects another organ system or in which dysfunction of the nervous system occurs along with dysfunction of several other organ systems. Examples of primary neurologic disorders include Alzheimer disease, migraine, and multiple sclerosis. Examples of secondary neurologic disorders include seizures secondary to infection with malaria, paraneoplastic syndromes associated with primary systemic cancer, and peripheral neuropathy occurring in the setting of nutritional deficiencies.
The distinction between primary and secondary neurologic disorders complicates the task of estimating global disease burden. For instance, do we classify diabetic neuropathy as a neurologic disorder or as a complication of an endocrinologic disorder? Should stroke be considered a neurologic disorder or a cardiovascular disease? Should head injury in the context of a motor vehicle accident be counted toward the burden of disease of neurologic disorders or of accidents? Various approaches have been taken to answer these questions, and in some instances, the definitions may shift depending on the purpose of the analysis. Although these distinctions may seem academic at first glance, they could have implications for public health campaigns and approaches to measuring, reporting, and acting on the relative burden of illness caused by different diseases.
ESTIMATING DISEASE BURDEN
There are several measures used to evaluate disease burden, including incidence, prevalence, morbidity, case fatality, mortality, disability, quality of life, pain, and cost. Incidence and prevalence are used to determine how common a disease is. The number of first cases of a disease over a defined time interval in a defined population determines its incidence. Prevalence measures the total number of cases, new and old, at a particular time in a defined population. Both indices depend on the accurate and complete enumeration of cases and adequate knowledge of the underlying population at risk. Case fatality refers to the proportion of patients with a disease who die from it. Mortality refers to the overall number of deaths due to the disease in a given time period.
Traditional approaches to estimating the impact of illness have focused on mortality because it is relatively easy to measure. The impact of some neurologic disorders may be reasonably captured by reference to their case fatality or mortality. For example, malignant brain tumors, strokes, and head injuries are often severe and may lead to death. A metric focused exclusively on mortality, however, will fail to capture the impact of many neurologic disorders that are chronic and slowly progressive, or intermittent and disabling, but that do not cause their sufferers to die. For example, multiple sclerosis is a disease process that has low mortality but inflicts a rather high level of disability on its patients; however, it is relatively rare. Alternatively, migraine is a neurologic disorder that also has low mortality but has moderate disability and is extremely common. Clearly, attempts to measure this type of disease burden require a more versatile metric than mortality alone.
More recent attempts to measure disease burden have therefore aimed at capturing not only mortality but also morbidity, which captures the disability, handicap, and other physical costs associated with the disease. One common approach to measuring burden of disease is to consider a time-based metric that incorporates premature mortality (the number of years of life lost due to premature death, based on an expected life span) and disability (years of healthy life lost as a result of disability weighted by the severity of the disability). The combination of both of these measures yields disability-adjusted life years (DALYs). DALYs are a well-established metric of disease burden that measure the number of healthy years of life lost as a result of both death and disability caused by a particular disease. One DALY constitutes 1 year of healthy life lost in an ideal world in which everyone lives into old age free of any disease or disability. One advantage to using the DALY to measure disease burden is that it allows comparisons of impact across very different disease states, in effect serving as a common measure for acute severe illness (stroke, head injury, myocardial infarction) and less severe chronic illnesses (epilepsy, migraine). The DALY metric thus reflects the impact of disease on both early mortality and on
disability, both of which are particularly important for assessing the overall impact of neurologic disease.
disability, both of which are particularly important for assessing the overall impact of neurologic disease.
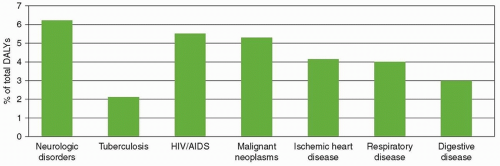
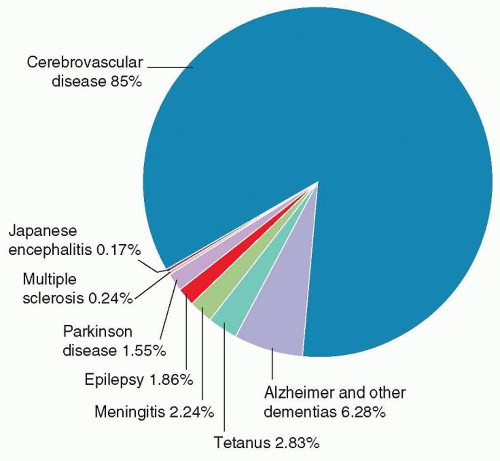
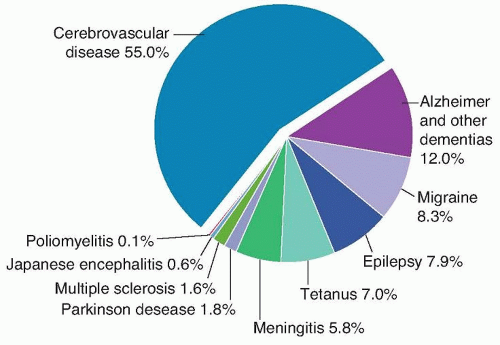
Neurologic disorders account for the largest proportion of DALYs of any category of disease, more so than cancer, heart disease, or pulmonary disease (Fig. 1.1). Within the category of neurologic disorders, the greatest proportion of DALYs is due to cerebrovascular disease, which represents just over half of the DALYs due to all neurologic disorders. Alzheimer disease and other dementias, together with epilepsy and tetanus, comprise another quarter of the DALYs seen with neurologic disease. Perhaps surprisingly, migraine encompasses 8.3% of DALYs among neurologic disorders, which is double that encompassed by Parkinson disease and multiple sclerosis combined, although it contributes little to the occurrence of deaths. Likewise, although epilepsy contributes to almost 8% of DALYs, it is responsible for less than 2% of deaths. Stroke, on the other hand, which is also frequently fatal, is responsible for 85% of deaths when compared to other neurologic disorders (Figs. 1.2 and 1.3).
Among neurologic disorders, stroke carries the largest burden of disease. Estimates from the Global Burden of Diseases, Injuries, and Risk Factors Study, sponsored by the World Health Organization (WHO), ranked stroke as the second most common cause of death and the third most common cause of DALYs worldwide in 2010. These numbers may still underestimate the burden of disease, however, because they are limited to the clinical stroke syndromes that lead patients to seek medical attention. They generally do not include the subclinical disease burden from cerebrovascular disease, such as subclinical infarcts and white matter injury from ischemia, which may lead to cognitive impairment and functional decline.
THE SHIFTING CHARACTER OF NEUROLOGIC DISEASE OVER TIME
The relative importance of different neurologic disorders over time has changed not only as a consequence of changes in population demographics and risk factors but also as a consequence of world events and scientific knowledge. For example, tremendous advances in our understanding of peripheral nerve injuries, including phantom limb pain, occurred during the civil war, through the examination of amputees and injured soldiers by Silas Weir Mitchell and colleagues. Further advances in our understanding of head injuries occurred during the First World War. Early in the 20th century, neurologists also frequently
encountered brain injury as a direct or indirect consequence of infections, including syphilis, tuberculosis, and viral encephalitis. For example, the Spanish flu pandemic of 1918 to 1919 gave rise to many cases of postencephalitic parkinsonism, a disorder made familiar to many through Oliver Sacks’ Awakenings. Later in the century, as life expectancy in developed countries increased, disorders of the elderly, including stroke and neurodegenerative disorders such as Parkinson disease and Alzheimer disease, were commonly encountered. Infectious neurologic disorders resurfaced again, however, in the 1980s in the form of the HIV/AIDS epidemic, with its well-known complications of toxoplasmosis and cerebral lymphoma. Rare and initially mystifying neurologic diseases have also captured the popular imagination and generated interest beyond what would be expected from the numbers of patients affected; the spongiform encephalopathies caused by prions, such as new variant Creutzfeldt-Jakob disease (or mad cow disease) had a tremendous impact in terms of teaching us about how diseases can jump from one species to another.
encountered brain injury as a direct or indirect consequence of infections, including syphilis, tuberculosis, and viral encephalitis. For example, the Spanish flu pandemic of 1918 to 1919 gave rise to many cases of postencephalitic parkinsonism, a disorder made familiar to many through Oliver Sacks’ Awakenings. Later in the century, as life expectancy in developed countries increased, disorders of the elderly, including stroke and neurodegenerative disorders such as Parkinson disease and Alzheimer disease, were commonly encountered. Infectious neurologic disorders resurfaced again, however, in the 1980s in the form of the HIV/AIDS epidemic, with its well-known complications of toxoplasmosis and cerebral lymphoma. Rare and initially mystifying neurologic diseases have also captured the popular imagination and generated interest beyond what would be expected from the numbers of patients affected; the spongiform encephalopathies caused by prions, such as new variant Creutzfeldt-Jakob disease (or mad cow disease) had a tremendous impact in terms of teaching us about how diseases can jump from one species to another.
THE EPIDEMIOLOGIC TRANSITION AND THE DOUBLE BURDEN OF DISEASE
The concept of the “epidemiologic transition” has been used to explain the shift in the types of diseases that often occur in countries as they pass through different stages of development. As nations industrialize and develop, the major causes of death and disability shift from a predominance of nutritional deficiencies and infectious diseases toward degenerative and chronic diseases, such as diabetes and cardiovascular disease. Investigators have described at least five stages of transition. The first stage (pestilence and famine) includes nutritional deficiencies and infection and characterizes regions such as sub-Saharan Africa and rural South Asia. In the second stage (receding pandemics), during which the pandemics of infectious disease and malnutrition recede, diseases related to hypertension, such as hemorrhagic stroke, become more common. China is an example of a region in this stage. During the third stage (degenerative and man-made diseases), life expectancy improves but high-fat diets, sedentary lifestyles, and cigarette smoking are introduced, allowing chronic, degenerative, and “man-made” diseases, including cardiovascular disease and ischemic stroke, to become more prominent. Urban India serves as an example of a country in this stage. As countries become more industrialized, populations are also exposed to new environmental hazards. In a study conducted in Taipei, Taiwan, urban air pollution was associated with increased numbers of emergency admissions for cerebrovascular diseases. In the fourth stage (delayed degenerative disorders), there are increased efforts to prevent, diagnose, and treat these lifestyle-related diseases, which allows for a delay in their age of onset as well as the increase in degenerative diseases affecting the elderly. Western Europe and North America are considered to be in this fourth stage of the epidemiologic transition. Finally, a fifth stage may exist (social upheaval and social regression) in which social upheaval and war break down the existing health structures, leading to a resurgence of conditions seen in the first two stages as well as to the effects of violence and accidents. Post-Soviet Russia has been suggested as an example of this fifth stage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree