Chapter 5 Head and Neck Blocks
 SPG block and RFA are very useful in the management of patients with intractable cluster headaches, migraine, trigeminal autonomic cephalalgias, and persistent idiopathic facial pain (“atypical facial pain”).
SPG block and RFA are very useful in the management of patients with intractable cluster headaches, migraine, trigeminal autonomic cephalalgias, and persistent idiopathic facial pain (“atypical facial pain”). Temporary diplopia is very common after SPG block because of spread of the injectate to the abducent nerve in the inferior orbital fissure. Diplopia may be used as a surrogate for a successful needle placement inside the pterygopalatine fossa (PPF).
Temporary diplopia is very common after SPG block because of spread of the injectate to the abducent nerve in the inferior orbital fissure. Diplopia may be used as a surrogate for a successful needle placement inside the pterygopalatine fossa (PPF). Practitioners should be familiar with the possible stimulation scenarios during SPG RFA to avoid lesioning the nearby maxillary nerve or branches. The optimal stimulation paresthesias should be behind the root of the nose.
Practitioners should be familiar with the possible stimulation scenarios during SPG RFA to avoid lesioning the nearby maxillary nerve or branches. The optimal stimulation paresthesias should be behind the root of the nose. Percutaneous radiofrequency thermocoagulation of the Gasserian ganglion is very successful in the management of patients with intractable trigeminal neuralgia when the pharmacological treatment is either ineffective or intolerable.
Percutaneous radiofrequency thermocoagulation of the Gasserian ganglion is very successful in the management of patients with intractable trigeminal neuralgia when the pharmacological treatment is either ineffective or intolerable. Percutaneous radiofrequency thermocoagulation of the Gasserian ganglion is usually considered for elderly patients at high risk for surgical microvascular decompression (MVD). The outcome may be less favorable than MVD, but it is less invasive with lower morbidity and mortality rates.
Percutaneous radiofrequency thermocoagulation of the Gasserian ganglion is usually considered for elderly patients at high risk for surgical microvascular decompression (MVD). The outcome may be less favorable than MVD, but it is less invasive with lower morbidity and mortality rates. The maxillary nerve exits through the foramen rotundum, which is located at the roof of the PPF. Hence, its block is essentially a modified SPG block.
The maxillary nerve exits through the foramen rotundum, which is located at the roof of the PPF. Hence, its block is essentially a modified SPG block. The mandibular nerve exits through the foramen ovale. The mandibular division (V3) is the most caudad and lateral part of the Gasserian ganglion.
The mandibular nerve exits through the foramen ovale. The mandibular division (V3) is the most caudad and lateral part of the Gasserian ganglion. The mandibular nerve can be blocked with either the lateral pterygoid approach or the foramen oval approach.
The mandibular nerve can be blocked with either the lateral pterygoid approach or the foramen oval approach. When performing SPG RFA, first look for inducing paresthesia at the root of the nose only to avoid injuring the maxillary nerve.
When performing SPG RFA, first look for inducing paresthesia at the root of the nose only to avoid injuring the maxillary nerve. When performing Gasserian ganglion RFA, try to be as selective as possible to the division affected to minimize potential adverse events.
When performing Gasserian ganglion RFA, try to be as selective as possible to the division affected to minimize potential adverse events. The approach to maxillary nerve block is essentially the same approach to SPG block; however, the needle is advanced more cephalad towards the foramen rotundum.
The approach to maxillary nerve block is essentially the same approach to SPG block; however, the needle is advanced more cephalad towards the foramen rotundum. Cranial nerves and ganglia blocks are advanced techniques that may be associated with considerable adverse events. One must be very familiar with the relevant anatomy to ensure a good outcome.
Cranial nerves and ganglia blocks are advanced techniques that may be associated with considerable adverse events. One must be very familiar with the relevant anatomy to ensure a good outcome.Sphenopalatine Ganglion Block and Radiofrequency Ablation
Indications
Cluster headache involves activation of the parasympathetic outflow from the superior salivary nucleus of the facial nerve, predominantly through the sphenopalatine ganglion (SPG).1 The SPG is a large extracranial structure that has rich autonomic innervation (both sympathetic and parasympathetic), which explains the autonomic features associated with cluster headache. SPG block and radiofrequency ablation (RFA) are indicated in the management of intractable medically-resistant cluster headaches, migraines, and other trigeminal autonomic cephalalgias, and intractable orofacial pain syndromes after exhausting other conservative treatment options (e.g., persistent idiopathic facial pain, “atypical facial pain”).
Sphenopalatine Ganglion Anatomy
The SPG is located in the pterygopalatine fossa (PPF), which is a small, upside-down pyramidal space 2 cm high and 1 cm wide. The PPF is located behind the posterior wall of the maxillary sinus and is bordered posteriorly by the medial plate of the pterygoid process, superiorly by the sphenoid sinus, and medially by the perpendicular plate of the palatine bone; laterally, it communicates with the infratemporal fossa. Superolaterally lies the foramen rotundum with the exiting maxillary nerve, and inferomedially, there is the vidian nerve (greater petrosal and deep petrosal nerves) within the pterygoid canal. The PPF contains the internal maxillary artery and its branches, the maxillary nerve, and the SPG and its afferent and efferent branches. The SPG is located posterior to the middle turbinate and is a few millimeters deep to the lateral nasal mucosa. It is suspended from the maxillary nerve by the pterygopalatine nerves; inferiorly, it is connected to the greater and lesser palatine nerves; and posteriorly, it is connected to the vidian nerve. Efferent branches of the SPG form the posterior lateral nasal and pharyngeal nerves.2,3
Approaches to the Sphenopalatine Ganglion
Transnasal Approach
Transnasal blockade of the SPG was first reported using topical cocaine.4 Currently, lidocaine 4% is usually used.
Transnasal Endoscopic Approach
This endoscopic technique for transnasal injection and blockade of the SPG was first described by Prasanna and Murthy in 1993.5 This technique allows a needle to be inserted transnasally under vision through the sphenopalatine foramen into the PPF.
Transoral Approach
The PPF can also be accessed transorally by placing a 27-gauge needle inside the greater palatine foramen. This approach is usually used by dentists to block the palatine nerves.6
Infrazygomatic Approach
Neuroablation techniques are only feasible with this infrazygomatic approach. Needle placement is usually guided by fluoroscopy; however, computed tomography guidance is reported as well.7
Anterior Approach
The needle entry is inferior to the zygomatic arch, just anterior to the mandible, between the mandibular ramus and the posterior border of the zygomatic bone. The author prefers this approach because the needle can be advanced in a target view toward the PPF without the need to walk the needle off the lateral pterygoid plate (which is usually very painful) (Fig. 5-1). Also, it is much easier to steer the needle (cephalad–caudad or anterior–posterior) within the fossa to selectively target different structures within the fossa. However, this approach is not feasible in all patients because there might not be enough room between the mandible and the zygoma to insert the needle.
Coronoid Approach
The needle entry is through the coronoid notch of the mandible. The needle is usually advanced to target the lateral pterygoid plate first and then walked off the bone interiorly to enter the PPF. By that time, the needle usually acquires certain direction, and it is hard to manipulate the needle after it is inside the fossa (Fig. 5-2).
Technique of Sphenopalatine Ganglion Block (Infrazygomatic Approach)
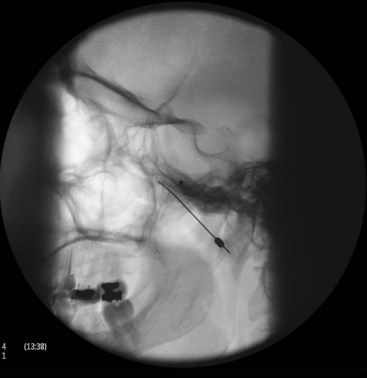
With the patient in the supine position and the head inside the C-arm, a lateral view is obtained and either the C-arm or the head of the patient is rotated until both pterygoid plates are superimposed on each other to better visualize the PPF. The skin entry site overlying the fossa is marked just inferior to the zygomatic arch either anterior to the mandible or through the coronoid notch. A 22-gauge, 3.5-inch blunt needle with a slight bend at the tip is used. The needle is first introduced in the lateral view and advanced medially and superiorly toward the PPF using real-time fluoroscopy. When in a proper direction, an anteroposterior (AP) view is obtained, and the tip of the needle is advanced to be just lateral to the nasal wall (Fig. 5-3). If the lateral pterygoid plate is encountered, the needle should be walked off the bone anteriorly and cephalad to slip into the fossa (the curved tip will help to guide the needle). A total of 0.1 to 0.2 mL of contrast agent is injected under real-time fluoroscopy to rule out intravascular spread because the PPF contains the maxillary artery and its branches (mainly the sphenopalatine artery). After negative aspiration of blood or air (the needle tip is too advanced into the nasal cavity or the maxillary sinus), 1 to 2 mL of 0.5% bupivacaine with or without steroids is injected slowly.
Radiofrequency Ablation Technique
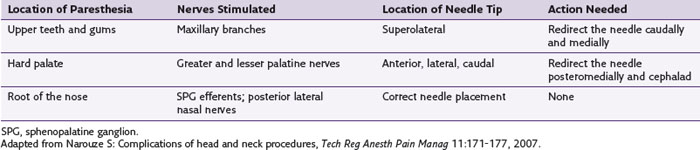
With the patient in the supine position and the head inside the C-arm, a lateral view is obtained and either the C-arm or the head of the patient is rotated until both pterygoid plates are superimposed on each other to better visualize the PPF. The skin entry site overlying the fossa is marked just inferior to the zygomatic arch either anterior to the mandible or through the coronoid notch. A 22-gauge, 10-cm, blunt RFA needle with a 2- or 5-mm active tip with a slight bend at the tip is used (Fig. 5-4). The needle is first introduced in the lateral view and advanced medially and superiorly toward the PPF using real-time fluoroscopy. When in a proper direction, an AP view is obtained, and the tip of the needle is advanced to be just lateral to the nasal wall. If the lateral pterygoid plate is encountered, the needle should be walked off the bone anteriorly and cephalad to slip into the fossa (the curved tip will help to guide the needle). Sensory stimulation is obtained with 50 Hz to look for deep paresthesias behind the root of the nose at less than 0.5 V (Table 5-1). After proper stimulation is achieved and before lesioning, 0.1 to 0.2 mL of contrast agent is injected under real-time fluoroscopy to rule out intravascular spread. Then 0.5 mL of lidocaine 2% is injected, and two radiofrequency lesions are carried out at 80° C for 60 seconds each. After lesioning, 0.5 mL of bupivacaine 0.5% and 5 mg of triamcinolone is injected with the aim of preventing postprocedure neuritis.8
Efficacy of Sphenopalatine Ganglion Radiofrequency Ablation
In a retrospective analysis of patients with refractory cluster headache treated by RFA of the SPG, 56 patients with episodic cluster headache and 10 patients with chronic cluster headache were followed over a period of 12 to 70 months.5 In the episodic cluster headache group, 60.7% experienced complete pain relief, but only three of 10 patients with chronic cluster headache had the same result. This report showed that RFA of the PPG may improve episodic cluster headache but not chronic cluster headache. Recently, however, Narouze and colleagues8 reported a favorable outcome after intractable chronic cluster headache as well. They reported significant improvement in both mean attack intensity and mean attack frequency for up to 18 months in 15 patients. Of these patients, 20% (three of 15) reported no change or increase in the headache intensity or frequency during the first few postprocedure weeks before noticing improvements in their headache pattern. However, 46.7% (seven of 15) of the patients reported a change in the headache pattern with return to the episodic form of cluster headache at a mean follow-up period of 18 months. Three patients remained headache free and off medications for the duration of the follow-up (18 to 24 months).
Two patients reported complete relief of their usual unilateral headache symptoms, and instead they developed episodic cluster headache on the contralateral side.8
Complications of Radiofrequency Ablation
Epistaxis is more frequent after the traditional intranasal topical application of local anesthetic; however, it can occur with this infrazygomatic approach if the needle is advanced too far medially through the lateral nasal wall.9
Intravascular injection and hematoma formation can occur after maxillary artery injury, which lies within the PPF (Fig. 5-5). Cheek hematoma is the most common complication. Infection is always a possibility, especially if the oral or nasal mucosa was accidentally penetrated.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree