26 Hydroscopy: Application to Pituitary Surgery
W. Derek Leight and Brent A. Senior
 Introduction
Introduction
Endoscopic transsphenoidal pituitary surgery as we know it today has been enabled by a series of advances in our understanding of physiology, medicine, and technology, in addition to advances in other fields, including endocrinology, microbiology, general surgery, urology, orthopedics, neurosurgery, and otolaryngology. Paradigm shifts in one field of medicine or surgery often come from borrowing and adapting techniques from other fields. In this fashion, endoscopic techniques have been transferred from one field to another, adapting to the specific requirements of each field. Neurosurgery, although a relative latecomer to endoscopic surgery, recently adapted traditional endoscopic techniques from the fields of urology, orthopedic surgery, and otolaryngology. This has produced a novel technique that is gaining worldwide acceptance: hydroscopy. Hydroscopy refers to the process of endoscopically visualizing the sella turcica using saline for low-pressure fluid distention. This technique has led to improvements in surgical techniques and outcomes for endoscopic transsphenoidal pituitary surgery.1,2
 History
History
The history of hydroscopy begins with the development of the cystoscope. While Bozzini developed the “Lichtleiter” in the early 1800s, modern endoscopy began with Nitze’s development of a functional cystoscope in 1878.3 This cystoscope was the first to utilize a lens and an electric light source at the tip of the instrument (Fig. 26.1). Cystoscopes were adapted to other disciplines, which led to the advancement of endoscopic techniques in many branches of medicine. Early cystoscopes used only air insufflation, which was very difficult in males and required patients to be in the uncomfortable genupectoral position to allow air to be vacuumed into the bladder by the downward pull of the abdomen. Application of a second cylinder for fluid instillation by Couriard and Evermann and advances in electronics and lighting led to fluid distention cystoscopy, which provided better visualization, easier exams in males, cooling for the light element, improved safety, and allowed the patient to be in the more comfortable lithotomy position.3,4
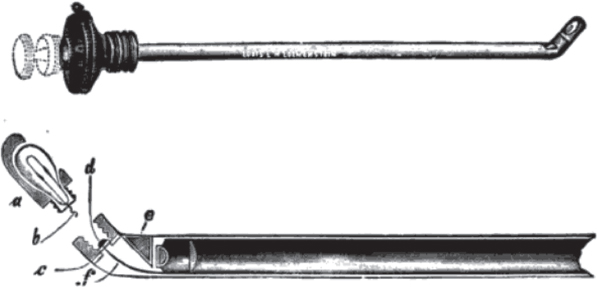
Fig. 26.1 Nitze’s cystoscope featured the first lens system and the first feasible light source at the tip of the endoscope, which paved the way for fluid distention cystoscopy. (From Luys G. A Treatise on Cystoscopy and Urethroscopy. St. Louis: Mosby, 1918. [This book is in the public domain.])
Although fluid distention eventually became standard in cystoscopy, most other branches of medicine adopted the method of air insufflation. In 1912, when Severin Nordentoft published his results of knee examinations using the trochar endoscope, arthroscopy using fluid distention was born.5 Japanese professor Kenji Takagi, unaware of Nordentoft’s findings, developed the first widely used arthroscopic instruments. Takagi’s protégé, Masaki Watanabe, developed the standard technique and instrumentation for arthroscopy using fluid distention, removed the first knee lesion arthroscopically in 1955, and eventually became known as the father of modern arthroscopy.6,7
Early neuroendoscopy centered on endoscopy of the ventricles and cerebrospinal fluid (CSF)-containing spaces. The first neuroendoscopic procedure was performed by urologist Victor L’Espinasse in 1910. He used a cystoscope to ablate the choroid plexus in two infants with hydrocephalus.8 Neuroendoscopic procedures such as choroid plexectomy and endoscopic ventriculostomy were performed by Dandy and others; however, the field did not catch on due to the technical difficulty, lack of adequate instrumentation, high mortality rates, and the development of the ventricular shunt and the operating microscope. By the 1970s, advances in endoscope and camera technology permitted the reintroduction of neuroendoscopic techniques.9 By 1992, Jankowski reported the first pure endoscopic transsphenoidal pituitary resection. In 1997, Jho and Carrau published the first large series of results using the pure endoscopic endonasal transsphenoidal approach. This approach became the basis for endoscopic skull base surgery.10 In 2005, Senior et al,1 combining the techniques of fluid distention endoscopy, nasal endoscopy, and neuroendoscopy, published the first description of hydroscopy of the sella turcica during endoscopic endonasal transsphenoidal pituitary surgery.
 Rationale
Rationale
The sella turcica is not a rigid space (Fig. 26.2). The bony tuberculum sella and dorsum sella tent up the diaphragma superiorly and the cavernous sinuses laterally. It is very distensible superiorly and relatively distensible laterally. After excision of a pituitary tumor, the potential space is filled in as the diaphragma collapses and the pituitary is decompressed. The result is that the lateral and superior corners of the sella become extremely difficult to thoroughly evaluate. Often, pockets of solid tumor may be left behind after an initial aspiration of a gelatinous portion of tumor. Other groups have advocated addressing this problem by having one surgeon retract the diaphragma superiorly and examine the cavity with angled endoscopes, while the other removes residual tumor with curettes and suction.11 In our experience, this technique has produced suboptimal visualization and been technically difficult, requiring two surgeons to have three or four instruments inside the sella at once. Other groups have tried using suction curettes as retractors in the sella; however, in our experience, this increases the risk of CSF leak by tearing the diaphragma, and it still provides only a focal view of the sella.
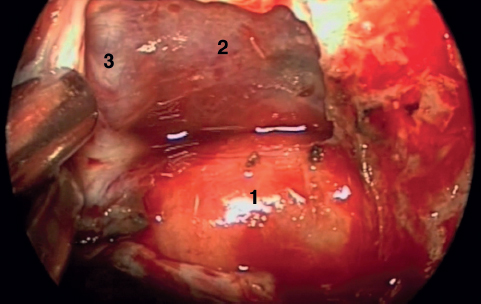
Fig. 26.2 This expanded view illustrates that the sella is a potential space, not a cerebrospinal fluid (CSF)-containing space. The tuberculum sella and planum sphenoidale have been removed. The pituitary (1), planar dura (2), diaphragma and C6 carotid segment (3) are visualized. (Courtesy of Dr. Adam M. Zanation.)





