Fig. 57.1
Lymphocytic hypophysitis. (a) Sagittal T1-weighted gadolinium-enhanced MR image. (b) Coronal T1-weighted gadolinium-enhanced image. Nodular thickening involves the superior pituitary stalk. The pituitary gland appears normal in size
Fig. 57.2
Lymphocytic hypophysitis. (a) Sagittal T1-weighted gadolinium-enhanced MR image. (b) Coronal T1-weighted gadolinium-enhanced image. Nodular thickening involves the pituitary stalk and the pituitary gland, which is mildly enlarged. There is also mucosal thickening in the adjacent sphenoid sinuses
Loss of the posterior pituitary bright spot has been described frequently [20].
Cystic components may be seen on MRI.
Tongue-shaped extension of the lesion along the base of the hypothalamus has been described [22].
Cavernous sinus invasion may occur in up to 18 % of patients, but is an atypical feature of this entity [2, 3, 23].
57.3 Histopathology
Histologically, inflammatory hypophysitis may be classified into three main categories—lymphocytic, granulomatous, and xanthomatous (including xanthogranulomatous)—which frequently demonstrate overlapping features [7].
57.3.1 Lymphocytic Hypophysitis
Histologically, lymphocytic hypophysitis is characterized by infiltration of the anterior pituitary gland by lymphocytes and plasma cells (Fig. 57.3). Germinal centers occasionally can be present.
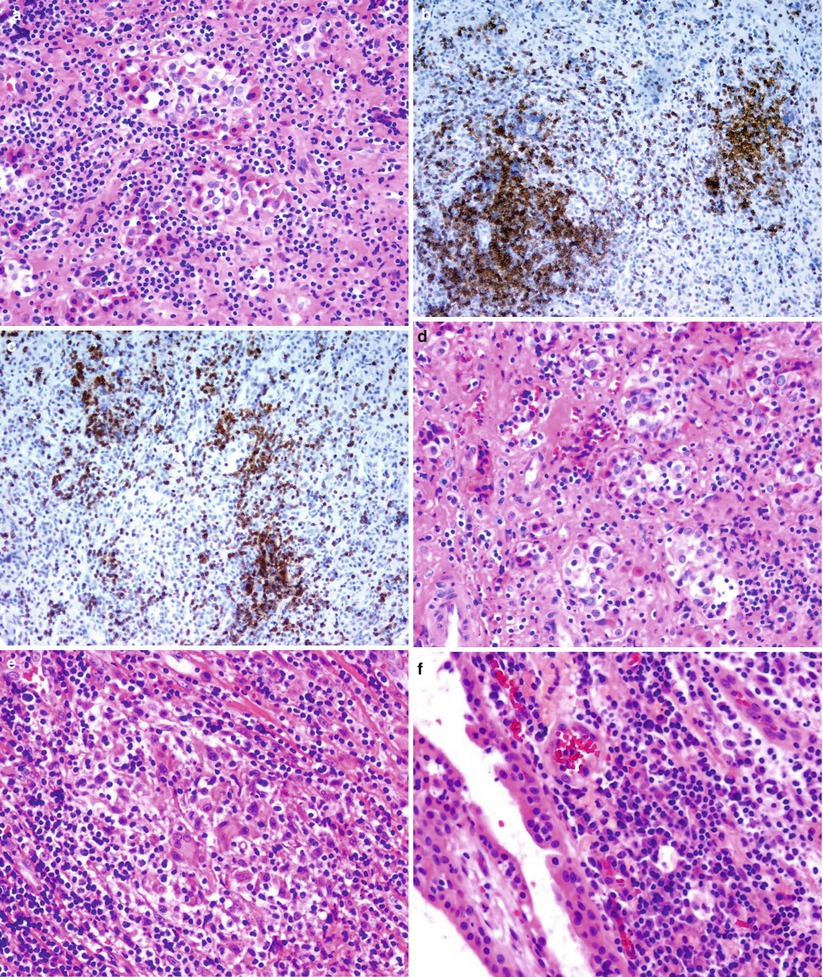
Fig. 57.3
Hypophysitis. Lymphocytic hypophysitis, the most common primary hypophysitis, is characterized by densely lymphoplasmacytic inflammatory cells that diffusely infiltrate the pituitary gland (a). The inflammatory infiltrate shows a mixed inflammatory population of CD3-positive T cells (b) and CD20-positive B cells (c). Extensive stromal fibrosis of the gland is seen in end-stage lymphocytic hypophysitis (d). Granulomatous hypophysitis displays dense, lymphoplasmacytic infiltrates and scattered granulomas with giant cells destroying and replacing the pituitary gland (e). Secondary hypophysitis is not uncommon in association with Rathke cleft cysts (f)
Later stages of the disease demonstrate atrophy of the gland parenchyma, a variable degree of fibrosis, and residual lymphocytic aggregates.
The inflammatory infiltrate is rich in T cells with CD4+ and CD8+ immunoreactivity [24].
57.3.2 Granulomatous Hypophysitis
Granulomatous hypophysitis is characterized by well-formed, noncaseating granulomas associated with variable lymphocytic infiltrates (Fig. 57.3e).
Varying degrees of parenchymal fibrosis also may be present.
Other granulomatous diseases (such as sarcoidosis and Langerhans cell histiocytosis) and infectious processes (such as tuberculosis) must be excluded before the final diagnosis.
57.3.3 Xanthomatous and Xanthogranulomatous Hypophysitis
Xanthomatous hypophysitis is characterized by infiltration of foamy histiocytes with no granuloma formation.
The cells are immunoreactive for CD68, but are negative for S100 protein and CD1a.
Intact anterior pituitary acini and vasculature are present, with inflammatory infiltrates of foamy histiocytes, lymphocytes, and multinucleated giant cells [9, 25].
Often granulation tissue and acellular debris can be seen [9].
Positive immunoreactivity for CD68 (macrophage marker) has been reported [9].
57.4 Clinical and Surgical Management
Medical management consists of high-dose corticosteroids and hormone replacement therapy.
More recently, azathioprine has been utilized with favorable responses in some patients.
Approximately half of patients will respond favorably to steroids, but those with visual loss on presentation or with otherwise refractory or progressive disease may require surgical management. The role of surgical intervention is for biopsy, sellar decompression, and improvement of visual symptoms [3, 7].
Transsphenoidal surgery is the mainstay procedure for biopsy, decompression, and partial resection of the mass.
Intraoperatively, the pituitary gland is frequently noted to have a firm, indurated consistency.
Most patients experience improvement in headaches and visual symptoms following surgical decompression [3].
Hypopituitarism secondary to hypophysitis is less likely to improve after surgery, and a majority of patients require long-term hormone replacement.
Medical therapy reduces the pituitary mass in 84 % of patients, improves anterior pituitary function in 45 %, and restores posterior pituitary function in 41 % [27].
Recurrence occurs in up to 15 % of patients, mandating close hormonal monitoring for several years following initial remission [3, 28].
It may be difficult to wean patients off high-dose corticosteroids, often mandating the use of other medical agents such as methotrexate, azathioprine, or rituximab [29, 30].
References
1.
Cheung CC, Ezzat S, Smyth HS, Asa SL. The spectrum and significance of primary hypophysitis. J Clin Endocrinol Metab. 2001;86:1048–53.CrossRefPubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








