Figure 43-1 Nerve conduction studies from a case of pork workers’ associated polyradiculopathy. Peroneal motor nerve conduction study (top): note prolonged distal latency at the ankle (A2) (normal <6.6 ms) with normal amplitude and conduction velocity (> 40 ms); peroneal F-wave study (bottom): markedly prolonged F-wave latency compared to F-estimate.
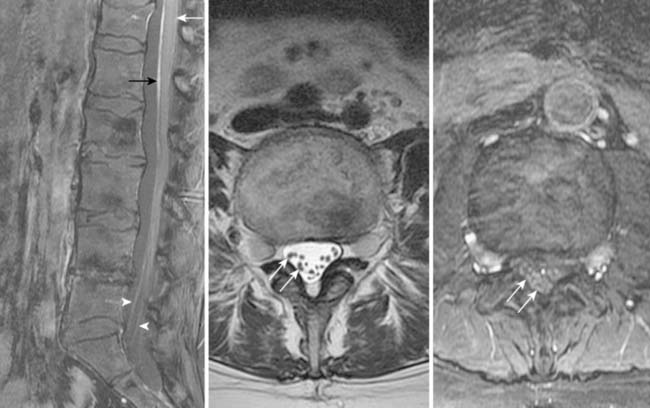
Figure 43-2 Lumbar magnetic resonance imaging studies from a case of pork workers’ associated polyradiculoneuropathy. Left, a sagittal T1-weighted (with fat saturation) postgadolinium image of the lumbar spine shows pial enhancement (white arrow), enhancement of the filum terminale (black arrow) and enhancement and enlargement of the cauda equina roots (arrowheads). Middle, an axial T2-weighted lumbar spine study shows enlarged nerve roots (arrows). Right, axial T1-weighted (with fat saturation) postgadolinium image shows enlarged, enhancing nerve roots (arrows).
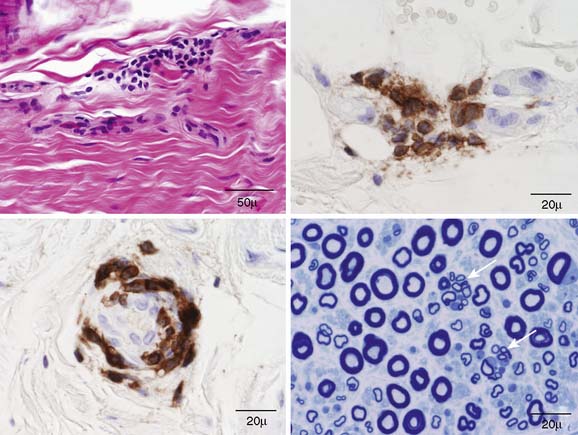
Figure 43-3 Sural nerve biopsy from patient with pork workers’ associated polyradiculoneuropathy. On upper left, a longitudinal paraffin hematoxylin and eosin section shows a small perivascular epineurial mononuclear cell collection. The upper right (longitudinal) and the lower left (cross-section) are CD45-reacted paraffin sections that show small epineurial perivascular inflammatory collections that involve the outer leaflets of the vessel walls. The lower right shows an epoxy section stained with methylene blue and shows two clusters of regenerating fibers (arrows). These findings are suggestive of an inflammatory immune pathophysiology.
CONCLUSION
Inflammatory demyelinating polyradiculoneuropathies are frequently seen by neurologists, the most well studied being chronic inflammatory demyelinating polyradiculoneuropathy (CIDP). A CIDP-like syndrome may occur with multiple other disease states, including cancers, monoclonal proteins, and perhaps diabetes mellitus. The development of an inflammatory neuritis has been studied in animal models, most notably with experimental allergic neuritis.
The discussed patient was one of a cluster of patients with neurologic disease (24 known at present) who worked in a pork processing facility with exposure to a specific pig brain removal process. The removal of the brain was accomplished through insertion of a hose into the foramen magnum of the hog, with expulsion of compressed air, which would break up the brain, and aerosolize parts of it, which could splatter the worker performing the procedure and workers nearby, and could be inhaled by nearby workers. The brain aerosolization process has since been discontinued at this pork processing plant.1
These patients tended to have a subacute onset of symptoms, with polyradiculoneuropathy as the most common presentation. Three patients had prominent central nervous system findings, one with encephalitis, another with transverse myelitis, and one with aseptic meningitis. Pain was a predominant feature, with nearly all patients having pain symptoms that were predominant in the lower extremities; burning and aching were commonly reported. Most patients had positive nerve stretch signs. The majority had weakness on examination, but it was usually distal and mild; it was more common to have self-reported feelings of “heaviness” and “fatigue” and difficulty walking, rather than significant objective weakness. Most patients developed numbness or tingling as part of their syndrome; cranial nerve and bowel/bladder dysfunction was rare. NCS/EMG commonly revealed markedly prolonged distal latencies and F-waves, with relatively spared conduction velocities, suggesting a process mainly of very distal and very proximal nerve. Thickened and/or enhancing nerve roots were common findings on neuroimaging. Most patients had some degree of small fiber dysfunction with aggressive evaluation. Nerve biopsies were performed on three of the patients with polyradiculoneuropathy and showed an abnormal degree of inflammation. All of these patients showed a distinct pattern of antibody reactivity on neuroimmunology testing.1
The suspected mechanism is that the aerosolization of brain material produced an overwhelming amount of nervous tissue antigens, which after inhalation, induced an autoimmune response. In most of the affected patients, the presentation was an autoimmune inflammatory polyradiculoneuropathy, differentiated from CIDP by the pain and sensory predominance, the preferential involvement of very distal and very proximal levels of nerve, and the frequency of small fiber involvement. Evaluation of the potential mechanism is ongoing at this time. This may represent a similar phenomenon to complications of the Semple rabies vaccine (which contained sheep nervous system tissue), in which both central and peripheral nervous system disease could be induced2; in these cases, high titers of antibody to myelin basic protein in the serum and CSF was correlated with severe neurologic disease.3 The specific antigen or antigens targeted in the series of patients on which we are reporting is not yet identified at the time of writing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








