Chapter 77 Insomnia
Diagnosis, Assessment, and Outcomes
Abstract
The goal of this chapter is to provide a comprehensive overview of the diagnosis of insomnia, the clinical assessment of insomnia, and the measurement of outcome and to provide a guide as to how to select from the growing array of assessment tools available. The focus is on the adult insomnia patient. The full assessment described here takes between 60 and 120 minutes, depending on the complexity of the patient’s insomnia. Given that many professionals needing to assess insomnia are time pressed, a quick assessment guide is included as Box 77-1. The information within Box 77-1 is elaborated in the text and can be used as a checklist or guide for the broad domains that should be covered during an assessment.
Box 77-1 Quick Assessment Guide
Type
Family and Social Factors
Diagnosing Insomnia
Insomnia is an ongoing difficulty getting to sleep, staying asleep, waking up too early, or waking up and feeling that the sleep obtained is not restorative. In addition to the sleep complaint, the person with insomnia reports daytime impairment and has an adequate opportunity for sleep.1 Three classification systems offer specific diagnostic criteria for insomnia. The Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision (DSM-IV-TR)2 and the International Classification of Diseases, 10th revision (ICD-10),3 offer a small number of broad categories based on current symptoms and functioning, but the International Classification of Sleep Disorders, second version (ICSD-2),4 offers a larger number of subtypes that require the assessor to make judgments about the causes of the insomnia. Table 77-1 lists the key features of the ICSD-2 diagnoses, and Table 77-2 summarizes the diagnostic codes of the ICSD-2 and the DSM-IV-TR. Research is needed to determine the validity and reproducibility of both the broad categories and the subtypes.
Table 77-1 Key features of ICSD-2 Insomnia Diagnoses
| INSOMNIA DIAGNOSIS | KEY FEATURES |
|---|---|
| 307.41 Adjustment sleep disorder | Associated with a specific stressor |
| 307.42 Psychophysiologic insomnia | Heightened arousal and learned sleep-preventing associations |
| 307.42 Paradoxical insomnia | Subjective report of severe sleeplessness not congruent with the absence or minor degree of daytime impairment |
| 327.02 Insomnia due to a mental disorder | Associated with mental disorder, but the insomnia constitutes a distinct complaint |
| 307.42 Idiopathic insomnia | Onset in infancy or early childhood |
| V69.4 Inadequate sleep hygiene | Associated with activities that are inconsistent with optimal sleep |
| V69.5 Behavioral insomnia of childhood | The result of inappropriate sleep associations or inadequate limit setting |
| 292.85 Insomnia due to a drug or substance | Disruption to sleep due to a drug or substance (prescribed, over-the-counter, or recreational) |
| 327.01 Insomnia due to a medical condition | Associated with a coexisting medical disorder or other physical issue |
| 780.52 Insomnia not due to a substance or physiologic condition, unspecified | Unable to be classified elsewhere but suspected to be associated with a mental disorder, psychological factor, or sleep-disruptive practice |
| 327.00 Physiologic (organic) insomnia, unspecified | Unable to be classified elsewhere but suspected to be associated with a medical disorder, physiologic state, or substance |
Table 77-2 Diagnostic Coding of Subtypes of Insomnia
| ICSD-2* INSOMNIA CATEGORIES | DSM-IV-TR† INSOMNIA CATEGORIES |
|---|---|
| 307.41 Adjustment sleep disorder | 307.42 Primary insomnia |
| 307.42 Psychophysiologic insomnia | 307.42 Primary insomnia |
| 307.42 Paradoxical insomnia | 307.42 Primary insomnia |
| 307.42 Idiopathic insomnia | 307.42 Primary insomnia |
| 327.02‡ Insomnia due to a mental disorder | 307.42 Insomnia related to another mental disorder |
| V69.4 Inadequate sleep hygiene | |
| V69.5 Behavioral insomnia of childhood | |
| 292.85 Insomnia due to a drug or substance | 292.89 Substance-induced sleep disorder, insomnia type |
| 327.01‡ Insomnia due to a medical condition | |
| 780.52 Other insomnia not due to a substance or physiological condition, unspecified | |
| 327.00 Organic insomnia, unspecified |
* American Academy of Sleep Medicine. International classification of sleep disorders (ICSD): diagnostic and coding manual, 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005.
† American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
‡ Code the primary condition first and the insomnia second (e.g., dysthymic disorder, 300.4, Insomnia due to a mental disorder, 327.02). Alternatively, one of the following codes may be used: ICD-10 Insomnia Categories,3 F51.0 Nonorganic sleep disorders, G47.0 Organic sleep disorders.
The Duke Structured Interview for Sleep Disorders (DSISD) is a structured series of questions that helps the clinician to efficiently establish DSM-IV-TR, ICSD-2, and research diagnostic criteria (RDC) insomnia diagnoses. Each section of the interview starts with a screening question. If this is endorsed, a series of follow-up questions are asked. If the screen is not endorsed the follow-up questions are skipped and the assessor moves to the screening question in the next category. The DSISD is divided into three sections: insomnia diagnoses, other sleep disorders (e.g., dyssomnia), and sleep disorders associated with excessive daytime sleepiness. The DSISD has been found to be effective for identifying those meeting criteria for an insomnia disorder.5
Clinical Assessment
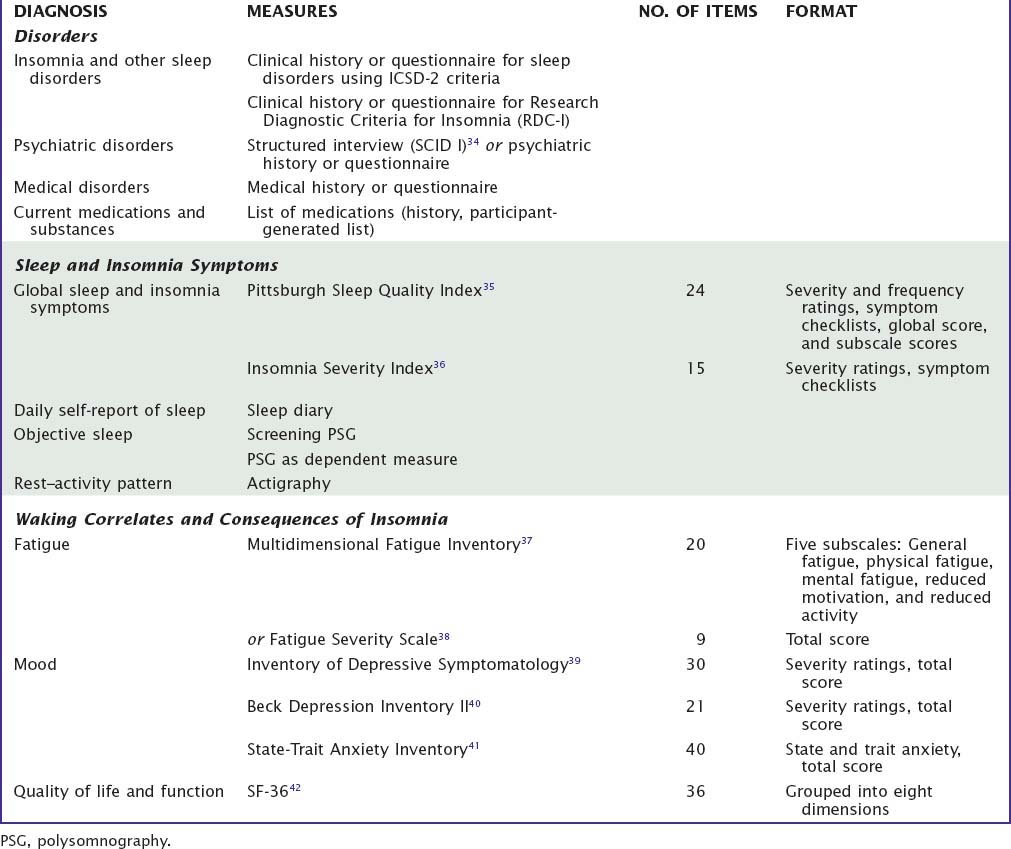
Recommendations for the standard research assessment of insomnia have been published.6 This was the result of a detailed review of the literature and an expert consensus process involving an evidence-based quantitative review of the available methods. Table 77-3 summarizes the measures selected by this process. Although these are recommendations for research contexts, they serve as a useful guide for clinicians to select from the vast array of instruments available.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree