11 Interventional Pain/Nonoperative Spine Procedures: Diagnostic and Therapeutic
I. Key Points
This chapter focuses on nonoperative diagnostic and therapeutic spine procedures for the purpose of understanding their context, purpose, technique, and diagnostic usefulness from a perspective limited to the spine. Appropriate ordering and analysis of these procedures requires proper documentation of the severity of pain, presence of numbness, presence of weakness, and detailed distribution of pain. The chapter is not intended to be a guide or a practicum to the performance of these procedures.
II. Description
– Diagnostic procedures: disc stimulation (provocation discography)
• Purpose: to identify pain originating from specific intervertebral discs (cervical, lumbar), typically axial in nature
• Single-needle technique: With particular attention to sterility, and with fluoroscopic guidance, a spinal needle is inserted obliquely and advanced carefully, avoiding the ventral ramus (Fig. 11.1, DC), into the center of the intervertebral disc. Provocation follows using slow contrast injection attached to a line pressure transducer. Attention to disc morphology is important, and level of pain/concordance, pressure, and volume injected must continuously be monitored. Final documentation of nucleus pulposus morphology according to the Dallas discogram scale should then be made, and the patient sent for computed tomography (CT) imaging.1
• Applicability: discogenic mediated pain
– Diagnostic procedures: medial branch block
• Purpose: to block pain transmission from the medial branches of the dorsal primary rami (cervical, thoracic, lumbar) that innervate the zygapophysial joints, significant mediators of axial neck and back pain
• Technique: With fluoroscopic guidance, a spinal needle is inserted obliquely (thoracic, lumbar), or posteriorly/laterally (cervical) and directed at the medial branch target, which is the centroid of the articular pillar in the cervical region (Fig. 11.2, MB), and the junction of the superior articular process and the transverse process in the thoracolumbar region2 (Fig. 11.1, MB). Each joint requires a block of the superior and inferior medial branch components. Comparative local anesthetic blocks should then be performed to diagnose the correct pain level and exclude false-positives.
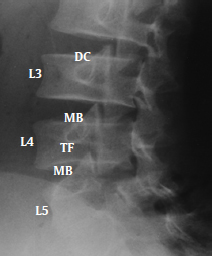
Fig. 11.1 Lumbar spine left oblique view. DC, intradiscal target; MB, medial branch target; TF, transforaminal target.
• Applicability: cervical spondylosis, thoracic spondylosis, lumbar spondylosis
– Diagnostic: sacroiliac joint block
• Purpose: to inject anesthetic into the sacroiliac joint and evaluate for alleviation of pain. Corticosteroid can be added to decrease inflammation and for therapeutic effect.
• Technique: Under the guidance of fluoroscopy, a spinal needle is inserted posteriorly and directed toward the inferior and posterior sacroiliac joint line. Confirmation of location is made with the use of contrast, and medication delivered.
• Applicability: sacroiliac pain
– Diagnostic procedures: selective spinal nerve block
• Purpose: to deliver a medication solution (usually anesthetic) to a spinal nerve root selectively (cervical, lumbar) in correlation with the alleviation (or absence) of a patient’s symptoms
• Technique: With fluoroscopic guidance, a spinal needle is inserted obliquely via a transforaminal approach into the neuroforamen of the spinal nerve root (cervical, thoracic, lumbar, or sacral spine). The target is the 6 o’clock position of the pedicle shadow of the corresponding nerve root level (Fig. 11.1, TF). Confirmation of location is then achieved with the use of contrast, and anesthetic delivered.
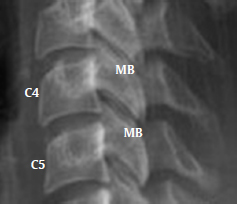
Fig. 11.2 Cervical spine lateral view. MB, medial branch target.
• Applicability: radiculopathy, polyradiculopathy, post-laminectomy syndrome
– Therapeutic procedures: epidural steroid injection
• Purpose: to alleviate pain by placing corticosteroids into the epidural space in response to the symptoms of discogenic pain, spinal stenosis, radicular pain, and epidural scarring
• Technique: With fluoroscopic guidance, a spinal needle is inserted posteriorly via a caudal, transforaminal (Fig. 11.1, TF), or interlaminar approach into the epidural space (cervical, thoracic, lumbar, or sacral spine). Confirmation of location is then obtained with the use of contrast, and medication delivered.
• Applicability: discogenic mediated pain, spinal stenosis, radiculopathy, post-laminectomy syndrome
– Therapeutic procedures: percutaneous medial branch radiofrequency neurotomy
• Purpose: to alleviate pain transmission from the medial branches of the dorsal primary rami (cervical, thoracic, lumbar) via ablation with a radiofrequency needle
• Technique: A radiofrequency electrode needle is inserted in a manner identical to that used for the medial branch blocks mentioned earlier. Sensory and motor stimulation testing are then performed to ensure appropriate positioning and nonstimulation of a nerve root. Upon confirmation, local anesthetic is provided and medial branch nerve lesioning commenced.
• Applicability: cervical spondylosis, thoracic spondylosis, lumbar spondylosis
– Therapeutic procedures: percutaneous lead spinal cord stimulation
• Purpose: to utilize the gate control theory1 and block transmission of pain signals through the spinal cord by electrical stimulation over the dorsal column of the spinal cord after an appropriate percutaneous trial has been conducted
• Technique: Place percutaneous lead(s) via an interlaminar approach, or a paddle surgical lead (typically improves coverage of axial back pain) into the epidural space (cervical or thoracic) with appropriate intraoperative testing or targeting to “cover” the patient’s pain.
• Applicability: post-laminectomy syndrome, chronic radiculopathy, peripheral neuropathy, complex regional pain syndrome
– Therapeutic procedures: trigger point injection
• Purpose: to break up lactic acid deposit in muscles to decrease myofascial pain
• Technique: After identification of painful taut bands in muscle, local anesthetic is applied and a small-gauge injection needle is used to pierce the skin and enter the muscle belly with the objective of breaking up the deposit.
• Applicability: myofascial pain
III. Pearls
– Specific diagnostic spinal injections can address targeted spinal pain conditions with the goal of identifying the origin of the pain and guiding surgery.
– Epidural injections typically target canal and foraminal mediated pathology.
– Injections directed at the medial branch and dorsal primary ramus typically target posterior element sources of pain.
Common Clinical Questions
1. Which procedure(s) could be beneficial in diagnosing axial lumbar back pain?
2. What is a potential benefit of the percutaneous approach to dorsal column stimulation over the paddle lead, and vice versa?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







