5 Lumbar Spine
I. Key Points
– The three-column model of the spine, developed to prognosticate the stability of thoracolumbar fractures, provides a framework to categorize the relevant clinical anatomy of the lumbar spine (Fig. 5.1)1:
• Anterior column: anterior half of the disc and vertebral body, as well as the anterior longitudinal ligament
• Middle column: posterior half of the disc and vertebral body, as well as the posterior longitudinal ligament
• Posterior column: posterior bony arch, facet joint and its capsule, supraspinous and intraspinous ligaments, and ligamentum flavum.
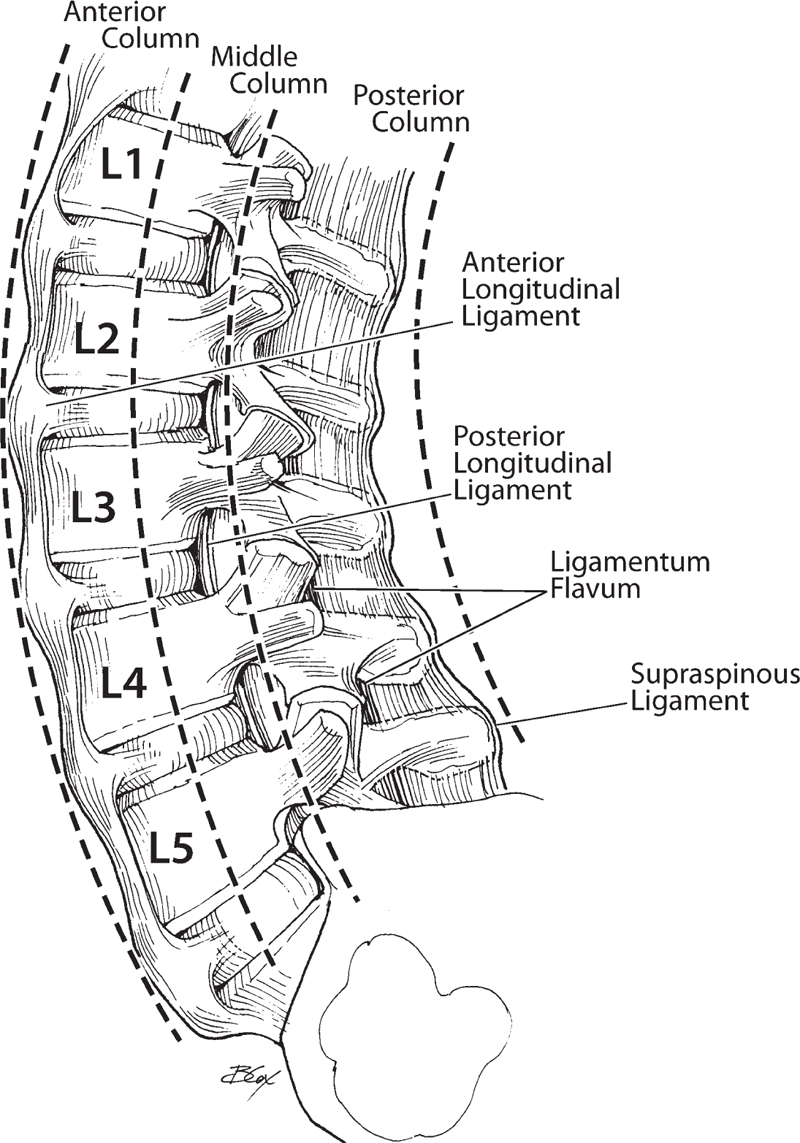
Fig. 5.1 Sagittal illustration of the lumbar spine demonstrating the three-column theory.
II. Bony Anatomy (Tables 5.1 and 5.2)
– The intervertebral discs lie between adjacent vertebral bodies. The annulus fibrosus is the outer layer of the disc; made of rings of collagen surrounding fibrocartilaginous zones, it limits the rotation between the vertebrae. The nucleus pulposus lies in the center of the disc; primarily gelatinous, its function is to absorb compression forces. Posterolateral herniation of the disc can compress an individual nerve root; central herniation can compress the entire cauda equina.1
– At the level of the pedicle, the transverse process arises. The processes of the first three lumbar vertebrae are long and slender, and those of the fourth and fifth are more pyramidal. In posterolateral lumbar fusion, the bone graft is often placed in the lateral gutter—the area lateral to the facets where the transverse processes lie.
– The pars interarticularis, also referred to as the isthmus, is a thin bone of the posterior arch of the lumbar vertebrae where the lamina and the inferior articular process join the pedicle and superior articular process. A fracture in the pars interarticularis is referred to as spondylolysis, can be found in 5 to 6% of the population, and predisposes the individual to the development of isthmic spondylolisthesis.1
– The facet joint is composed medially of the inferior articulating process of the superior vertebrae and laterally of the superior articulating process of the inferior vertebrae. Surrounding the facet joint is an articular capsule. Hypertrophy of the facet joint and its capsule can contribute to both spinal and foraminal stenosis.2
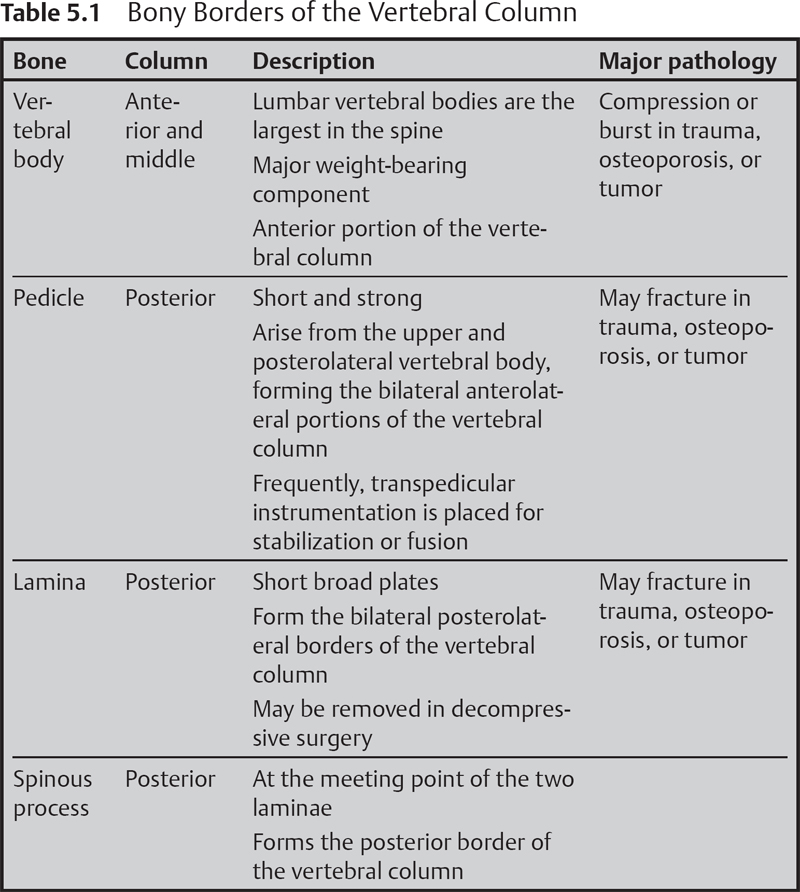
Table 5.2 Borders of the Intervertebral Foramen
| Anterior | Posterior borders of the adjacent vertebral bodies and discs | |
| Superior | Inferior border of the pedicle of the superior vertebrae | |
| Posterior | Pars interarticularis and facet joint | |
| Inferior | Superior border of the pedicle of the inferior vertebrae |
III. Neural Anatomy
– The spinal cord ends at the conus medullaris, most frequently at the level of the L1 vertebral body or the L1/L2 disc space. Inferiorly, the roots descend within the thecal sac as the cauda equina before they exit individually (Fig. 5.2).3
– The exiting nerve roots leave the vertebral column through the intervertebral foramen, closer to the superior pedicle. Far lateral disc herniations can compress the nerve root at this point (leading patients to present with radiculopathy); in such cases, the intervetebal disc actually compresses the nerve root of the superior level (for example, an L4/L5 disc compresses the L4 root). Far lateral herniation is much less common than posterolateral herniation of the disc. Facet hypertrophy can also lead to foraminal stenosis, which also causes radiculopathy.1
– Posterolateral disc herniation compresses the traversing nerve root at its lateral recess, before it reaches the intervertebral foramen. In this case, it compresses the inferior nerve root (for example, an L4/L5 disc compresses the L5 root).1
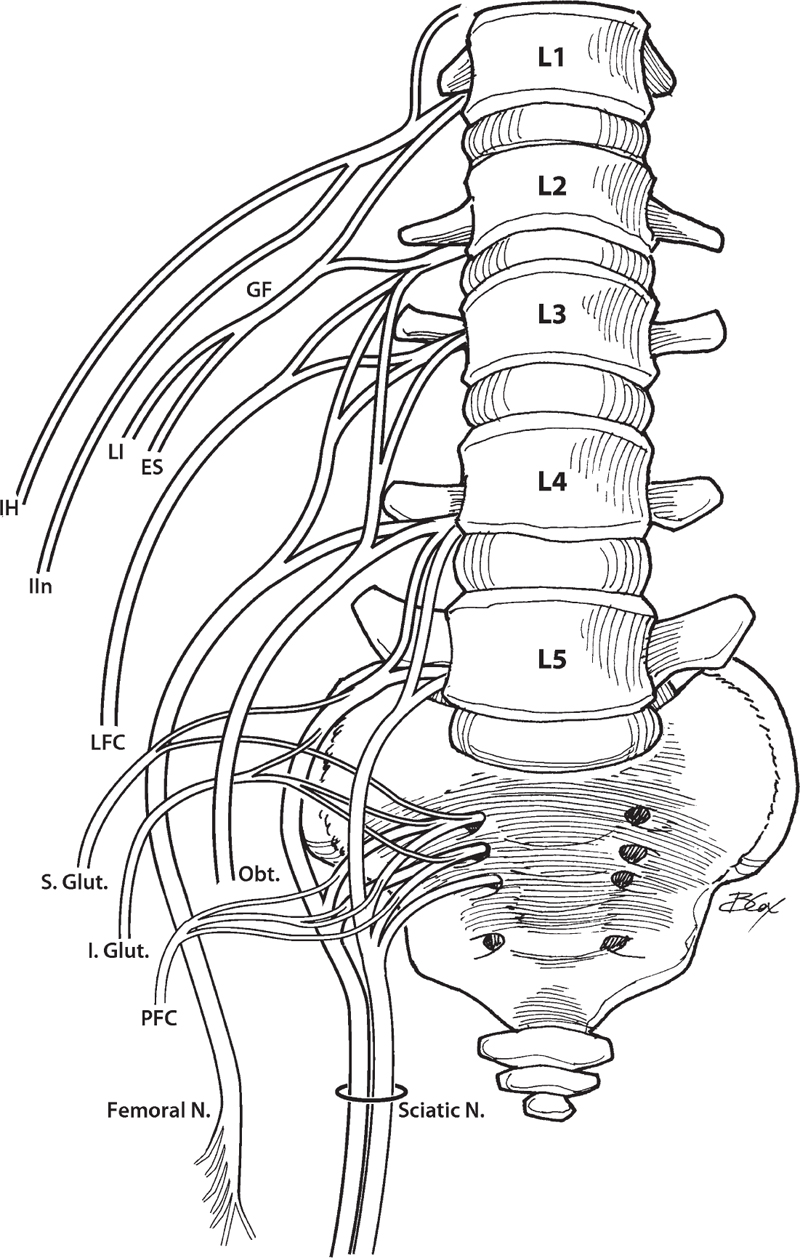
Fig. 5.2 Anterior view of the lumbar plexus.
IV. Vascular Anatomy
– Segmental arteries arise primarily from the lumbar arteries, which in turn divide into anterior and posterior radicular arteries, which enter the intervertebral foramen along with the nerve roots. The arterial feeders of the spinal cord include branches of these radicular arteries as well as the segmental medullary arteries, which also come off of the segmental spinal arteries, with one artery coursing anteriorly and two coursing posteriorly. The cauda equina is supplied by branches of the lumbar, iliolumbar, lateral, and median sacral arteries.3
– Two different plexuses of veins, one external and the other internal, extend along the vertebral column. The anterior external plexus lies in front of the vertebral bodies, and the posterior external plexus lies around the posterior arch of the vertebral column. The internal vertebral plexus is a network of veins in the epidural space within the vertebral canal that are in communication with the basivertebral plexus; the veins tunnel through the cancellous tissue of the vertebral bodies. Intradural venous drainage of the spinal cord involves retrograde anterior and posterior central veins.3
– Approaching the lumbar spine from an anterior approach, the great vessels (the aorta and the inferior vena cava) lie directly anterior to the vertebral bodies, with the bifurcation of the vessels at the level of the L4/L5 disc space or at the level of L5. The L5/S1 disc can generally be accessed inferior to the bifurcation; to reach the L4/L5 disc, these vessels must be retracted laterally.1
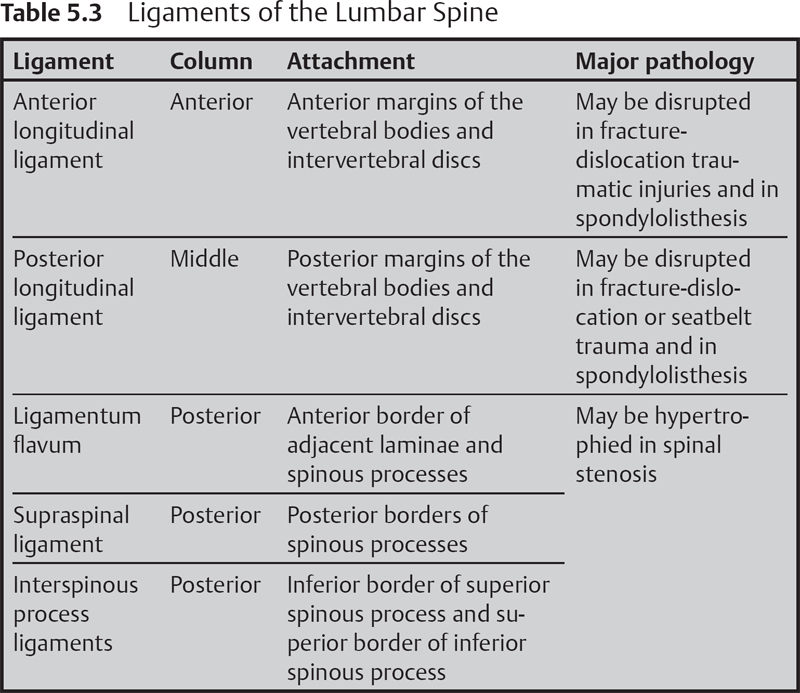
V. Ligamentous and Muscular Anatomy (Table 5.3)
– Exposure of the lumbar spine from a posterior approach requires traversing the throracolumbar fascia. In the lumbar region, the thoracolumbar fascia is thick and is attached to the spinous processes and the supraspinous ligament. It then extends laterally, covering the erector spinae muscles.2
– Deep in the thoracolumbar fascia lie the erector spinae muscles, which arise from the sacrum, the spinous processes of the lumbar and thoracic vertebrae, and the iliac crest. The erector spinae muscles include the iliocostalis, longissimus, and spinalis muscles, which are important in flexion, extension, and lateral rotation of the vertebral column. Deep in the erector spinae muscles are the multifidus and rotatores muscles.2
VI. Surgical Pearls
– During transpedicular instrumentation placement, the land-marks used for cannulation of the pedicles are the meeting point of the pars interarticularis, the superior articulating process, and the transverse process. There is a small ridge of bone at that level called the mammillary process.
– For lumbar disc herniation, after a laminotomy is performed, feel for the inferior pedicle (L5 in an L4-L5 disc herniation). Palpate its medial wall with a Woodsen dissector. Immediately inferior is the nerve root (L5). With a nerve hook, retract the root medially and dissect superiorly until you feel a bulge (which is the herniated disc fragment).
Common Clinical Questions
1. Compression of the nerve root in the neural foramen is most often due to hypertrophy of which facet?
2. An L4/L5 far lateral herniated disc will compress which nerve root?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







