61 Lumbosacroiliac Fixation
I. Key Points
– Lumbosacroiliac (LSI) fixation provides the strongest biomechanical construct for sacral fractures and lumbopelvic dissociations.1
– The construct spans the sacrum and allows for relatively normal load transfer from the lumbar spine through the sacroiliac (SI) joints to the pelvis, permitting early post-op weight bearing.
– In long constructs, including L5-S1, iliac (pelvic) fixation improves fusion rates of vertebrae.2
– Iliac screws must remain in bone throughout their length to prevent injury to pelvic viscera and neurovascular structures.3
– Sacropelvic relationships should be measured and taken into account in performing long-segment fixation extending into the sacrum/ilium (Table 61.1 and Fig. 61.1).
II. Indications
– Complex sacral fractures with or without pelvic discontinuity
– Adult scoliosis patients with L5-S1 spondylolisthesis
Table 61.1 Commonly Measured Pelvic Parameters
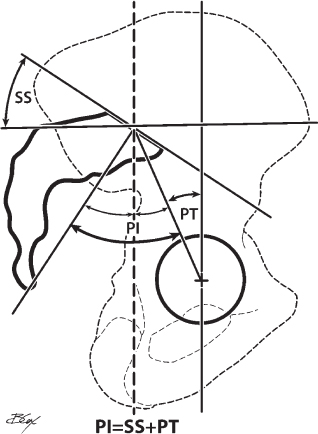
Fig. 61.1 Sacropelvic radiographic measurements.
– Revision lumbosacral fusion
– Adult isthmic spondylolisthesis
– High-grade dysplastic spondylolisthesis
III. Technique
– A subperiosteal dissection is made to the lumbar transverse processes, sacral ala, and posterior superior iliac spine (PSIS).3
• While exposing the sacrum, stay extraperiosteal and avoid falling into the dorsal sacral foramina.
– Using blunt and sharp elevators, lift the musculature off of the inner and outer aspects of both iliac wings to help establish the direction for iliac screw placement.
– S1 pedicle screw: Placement begins by identifying the region where the ala and lateral S1 facet meet; a high-speed bur can be used to mark the starting point (Fig. 61.2).3
• This point is typically 1 cm cephalad to and slightly lateral to the S1 foramen.
– S2 pedicle screw: Placement begins by identifying the inferior medial aspect of the dorsal S1 foramen and the superior medial aspect of the dorsal S2 foramen; the starting point is the middle of an imaginary line connecting the two points, which can be marked with a high-speed bur (Fig. 61.2).3
– Use a gearshift probe to create a path from this starting point to the anterior cortex of the sacrum; gently tap the gearshift with a mallet to perforate the anterior cortex.3
• S1 screw: typically 6.5 mm in diameter and 40 to 45 mm in length; should be aimed medially for the sacral promontory
• S2 screw: typically 6.5 mm in diameter and 50 to 60 mm in length; should aim 30 to 35 degrees laterally and tilt cephalad 15 to 20 degrees (parallel to the SI joint)
– Iliac (pelvic) screw: placement begins by identifying the inferiomedial aspect of the PSIS (Fig. 61.2)
– Using a high-speed bur or a rongeur at the PSIS, find cancellous bone and then use the gearshift probe to develop a screw path that runs between the inner and outer cortex of the ilium.
– The path, directed toward the anterior inferior iliac spine (AIIS), should not be forced and should be produced easily; if resistance is met, consider a larger soft-tissue exposure and/or the use of fluoroscopy to guide the gearshift along a more appropriate path.3
• The combination obturator-outlet view best shows the proper starting point and path of the iliac screw.1
• The combination obturator-inlet view confirms that the screw has not violated the inner or outer iliac cortex (Fig. 61.3). 1
• A true lateral oblique view of the pelvis or iliac ensures that there is no sciatic notch or acetabular encroachment of the iliac screws and confirms full accommodation of the screw length (Fig. 61.4).
• A simplified method of iliac screw insertion is to place one’s finger within the sciatic notch along the outer table of the ilium and use this landmark as a guide in probe and screw insertion, without the need for intraoperative fluoroscopy or Kirschner wire (K-wire) guidance.
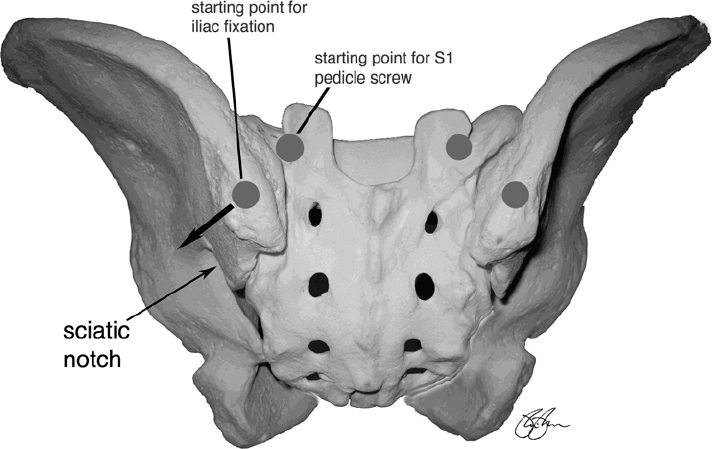
Fig. 61.2 Posterior view of pelvis. Note starting points for the sacral and iliac screws.
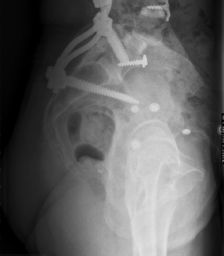
Fig. 61.3 Lateral lumbopelvic x-ray demonstrating appropriately positioned pelvic fixation. Note position of pelvic screws in relation to the sciatic notch.
– Using a K-wire and tap, the final iliac screw is placed; it is typically 7.5 to 8 mm in diameter and 65 to 90 mm in length.
• In revision cases where iliac crest bone was harvested for grafting for the index procedure, iliac screw placement can be more challenging and longer screws may be used.3
• Iliac screws must stay entirely within bone given the proximity of various pelvic structures.
– A rod is used to connect the sacral screw, the iliac screw, and the construct.
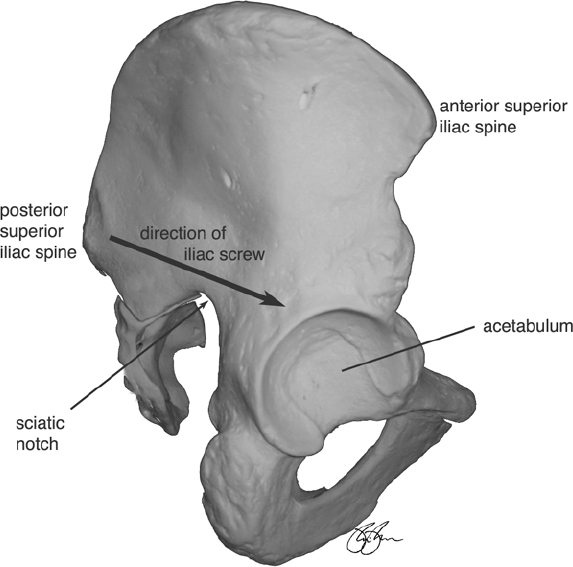
Fig. 61.4 Lateral view of pelvis showing anatomic landmarks and direction of safe placement of the iliac screws.
IV. Complications
– Infection and wound rates approach 20%.4
– Symptomatic hardware requiring removal3
– A formal SI joint arthrodesis is generally not performed; as a consequence, the implant may fracture due to fatigue failure.4
– Superior gluteal artery injury from sciatic notch violation4
– Wound breakdown due to disruption of the distal erector spinae musculature attachment. When elevating the posterior paraspinal muscles to expose the medial border of the ilium, be careful not to disrupt the distal attachment of the erector spinae muscles as that may lead to wound problems.
V. Postoperative Care
– Early patient mobilization
– External orthosis (if utilized) must include leg extension (to immobilize hip).1
VI. Outcomes
– L5-S1 fusion rates approach 92% with utilization of sacropelvic fixation.4
– Iliac screw placement is possible in revision cases; in one series, 34 of 36 patients had successfully placed iliac screws despite previous iliac crest graft harvesting.4
– Iliac screw loosening is reportedly as high as 52%, although this did not correlate with pseudarthrosis; the rate of iliac screw breakage is considerably lower (5.3%).2
– Nearly half of patients report being able to feel their instrumentation.2
– The infection rate is reported at 3.7%.4
VII. Surgical Pearls
– The site of iliac crest bone grafting should be made more superiorly along the crest to maintain adequate bone stock for iliac/ pelvic bolt fixation.3
– LSI fixation can be combined with iliosacral screws (triangular osteosynthesis) to stabilize the weight-bearing axis and the pelvic ring.5
– In the placement of bicortical S1 screws, medial screw angulation is necessary to avoid traversing the L5 nerve root.1
– Separate (accessory) incisions can be utilized for iliac fixation with the use of subcutaneous tunneling to connect to lumbosacral fixation.3
Common Clinical Questions
1. Which pelvic view best confirms that the iliac screw has not violated the inner or outer cortex of the ilium?
A. Lateral
B. Anteroposterior
C. Iliac oblique
D. Obturator-inlet
E. Obturator-outlet
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







