Chapter 165 Management of Degenerative Lumbar Stenosis and Spondylolisthesis
Lumbar Spinal Stenosis
Decision Making in Surgical Intervention
There is an overlap of radiologic findings between these two entities that requires further categorization. The differentiation of pure lumbar stenosis from degenerative spondylolisthesis begins with plain radiographs and dynamic lateral flexion and extension x-rays. The patient’s symptoms should correlate with the pathologic anatomy noted on all preoperative imaging studies. Greater than 4 mm of anterior translation of the superior vertebral body on the inferior body constitutes degenerative spondylolisthesis.1 Standing lateral flexion and extension x-rays can provide additional evidence of dynamic instability to supine lateral flexion and extension views. Each level of the lumbar spine can be assessed preoperatively for individual stability based on disc height, angular motion of the end plates, translation as measured on plain radiographs, or fixed or mobile translation as evaluated on dynamic radiographs. Unfortunately, the preoperative assessment of stability loses significance after destabilizing decompressive procedures are performed.
Surgical Intervention
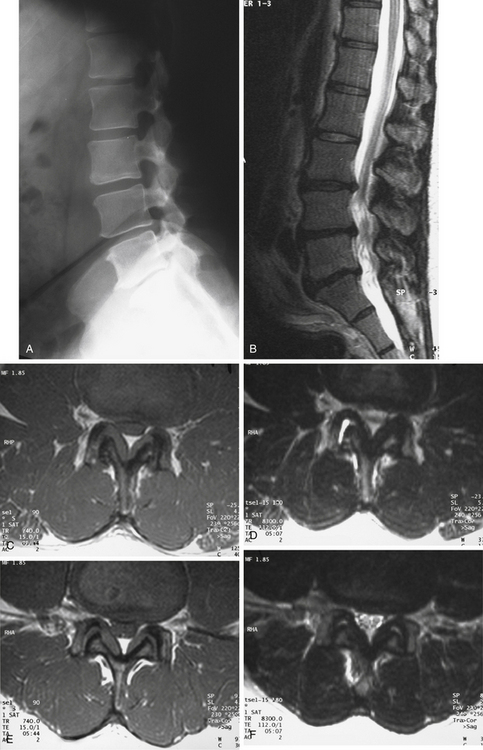
The purpose of any surgical intervention is to decrease pain, improve function, and prevent neurologic deterioration. The goal of surgical decompression is to decompress all of the neural elements that are producing the patient’s symptoms. Degenerative changes can span multiple vertebral levels on imaging studies, but not all levels may be involved in producing the patient’s stenotic symptoms at the time of examination. Neural compression is documented well by magnetic resonance imaging (MRI). Increased sophistication in the technology and interpretation of MRI scans, with or without supplemental computed tomography (CT) images, has decreased the “mandatory” use of CT-myelography for all surgical patients. Some radiologic facilities supplement MRIs with selected CT cuts through the spine areas where maximal compression has occurred. A CT image better defines the bony architecture of the spinal column, whereas an MRI scan better depicts the soft neural structures. The CT scan also provides information on the extent of the neural compression due to bone involvement. Neural compression is usually due to a reduction of the spinal canal from posterior protrusion of the disc material, hypertrophy of both the facets and ligamentum flavum, and the listhesis.
The lamina, hypertrophic ligamentum flavum, and osteophytic areas of facet joints can all contribute to the stenosis and therefore require removal. The excess ligamentum flavum should be removed prior to or as a part of the facetectomy. Part of the facet joint may be removed by means of undercutting the medial aspects of both facets. Once again, fusion must be considered if greater than 50% of either facet is removed. Decompression is often performed in a caudal to cranial direction, usually to the level of the pedicle of the vertebra below the involved level. This is accomplished in three steps: First, the central canal is decompressed using a high-speed bur and a Kerrison rongeur. Second, both lateral recesses are decompressed by partially removing the medial aspect of each inferior facet, with subsequent undercutting of the respective superior facets. Third and last, a fine instrument, such as a blunt dental tool or a Frazer dural angled elevator, is used to assess the degree of foraminal stenosis as well as the adequacy of foraminal decompression. The final foraminal decompression is performed using a fine Kerrison rongeur placed just dorsal to the nerve root. The neural foramen is adequately decompressed when the nerve root can be gently retracted about 1 cm medially. Visualization of the pars interarticularis must be maintained to avoid excessive bone removal (Fig. 165-1). Constant vigilance is required during this portion of the procedure.
A limited laminectomy has also been described for treating spinal stenosis.2 In this procedure, the central portion of the neural arch is preserved. Thus, the interspinous and supraspinous ligaments remain intact, minimizing spinal instability. Hemilaminectomy is indicated for patients with unilateral stenosis and unilateral symptoms. However, this procedure potentially makes it difficult to decompress the contralateral side or to perform adequate decompression of the ipsilateral foramen. This is due, in part, to the difficulty in angling instruments laterally to enter the foramen in the presence of an intact spinous process and midline ligaments. An alternative to limited laminectomy is a hemilaminotomy procedure, where two hemilaminotomies are performed on the adjacent hemilaminae. Partial facet excision is then performed for greater lateral decompression, as described for hemilaminectomy.
Another published method is a lumbar laminoplasty, a treatment used in active manual workers.3 It is a procedure similar to cervical laminoplasty. Affected spinous processes are removed at the base, and bilateral unicortical grooves are made at the junction of the lamina and facets. The laminae are then split in the midline and the canal is opened. Spinous process or bone allograft is placed between the open laminae and held secure with suture or steel wire through previously made holes in the laminae and grafts. A body cast is mandatory postoperatively for a minimum of 2 weeks to avoid stress on the construct during ambulation.3 This procedure has very limited clinical indications.
Discectomy is generally not required in the treatment of lumbar spinal stenosis. True herniations are uncommon. However, the surgeon should assess each case for the possibility of a concomitant disc herniation or hard ridge that might compress the root. In the presence of a markedly bulging disc or in the case of a true soft disc herniation that is contributing to significant nerve root compression, a discectomy may be needed. This being said, a discectomy can also cause subsequent spinal instability, because both anterior and posterior elements are sacrificed. In this circumstance, some surgeons recommend arthrodesis at the time of surgery. Spinal stability should be maintained during decompression by preserving both the pars interarticularis and the facet joints. However, in many cases, much of the facet joint might need to be removed for adequate decompression of the involved nerve root.
Surgical Outcome for Spinal Stenosis
Surgical outcome for lumbar spinal stenosis is quite varied. In a prospective, nonrandomized observational cohort study of patients with spinal stenosis followed for 1 year, 55% of surgical patients reported definite improvement. This was in contrast to the nonsurgical patients, of whom only 28% reported a satisfactory outcome.4 In a prospective study of 105 consecutive patients undergoing decompressive laminectomy, a 63% to 67% rate of satisfactory results was reported at 2 years. This result deteriorated to 52% at 5-year follow-up.5 Sixteen percent of these patients underwent reoperation for severe back pain or recurrence of their stenosis (or both) during the 5-year period. Risk factor for poor outcome was correlated to a preoperative duration of symptoms of more than 4 years, significant comorbidity, and preoperative back pain. In another series of 140 patients treated surgically, at an average follow-up of 3 years, 71% reported an improvement in back pain and 82% improvement in leg pain.6 In a longer follow-up of 2.8 to 6.8 years of 88 patients with decompression laminectomy, Katz concluded that 11% of patients had poor results at 1 year.7 This poor quality results later increased to 43% with a reoperation rate of 17% at final follow-up. Again, poor outcome was correlated to preoperative comorbidities and limited decompression. Turner and colleagues performed a meta-analysis of the lumbar stenosis literature and noted a 64% mean proportion of good to excellent results over the long term.8
Most studies indicate that decompression alone is adequate in pure lumbar stenosis without significant spondylolisthesis or other deformity. In a prospective randomized study by Grob and colleagues, 45 patients underwent decompression or decompression with arthrodesis for pure stenosis. There was no significant difference in clinical outcome among patients.9 Overall satisfactory results were 78% for patient-related outcome data in all groups, including decompression without arthrodesis, decompression plus fusion of the most significant stenotic segment, and decompression with arthrodesis of all stenotic levels. They concluded that lumbar spine decompression alone changed the natural history of this disease, with improvement in quality of life. They also determined that arthrodesis is indicated when stenosis is associated with degenerative spondylolisthesis, scoliosis or kyphosis, recurrent stenosis at the same level, stenosis adjacent to a prior fusion, aggressive facetectomy, or need for a disc excision. Other prospective randomized studies have concurred on the role of fusion for stenosis associated with degenerative spondylolisthesis.10,11
Complications associated with surgical intervention for lumbar stenosis are more common in cases of increased preoperative morbidities, advancing age, and complex surgical procedures. Two studies have demonstrated a relationship between mortality rate and age. One study showed a higher mortality rate of 0.6% in patients older than 75 years (about ninefold compared with patients younger than 75 years) with a complication rate of 17.7% (compared with 9.1%).12 The second study showed similarly increased rates for patients older than 80 years.13 The most commonly cited comorbidities in the literature are osteoarthritis, cardiac disease, rheumatoid arthritis, and chronic pulmonary disease. However, the risk factors most closely correlated with a poor outcome are preoperative complaints of predominantly low back pain, followed by preoperative comorbidities. Complications of decompression procedures are postoperative neurologic deficit, dural tear, cerebrospinal fluid fistulas and pseudomeningoceles, facet fractures, infection, and vascular injury.
Weinstein and colleagues14 examined 1244 patients in the Spine Patient Outcomes Research Trial (SPORT) and divided patients into prospective randomized (501 participants) and observational (743 participants) cohorts at 13 spine clinics in 11 U.S. states. Patients were observed at 4 years using SF-36 Bodily Pain (BP) and Physical Function (PF) scales and the modified Oswestry Disability Index (ODI, AAOS/Modems version) assessed at 6 weeks, 3 months, 6 months, and annually thereafter. In the 4-year combined as-treated analysis, those receiving surgery demonstrated significantly greater improvement in all the primary outcome measures (mean change surgery versus nonoperative; treatment effect): BP (45.6 vs. 30.7; 15.0; 11.8 to 18.1), PF (44.6 vs. 29.7; 14.9;12.0 to 17.8) and ODI (−38.1 vs. −24.9; −13.2; −15.6 to −10.9). The percentage of patients working was similar between the surgery and nonoperative groups, 84.4% versus 78.4%, respectively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree