53 Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF)
I. Key Points
– Minimally invasive transformational lumbar interbody fusion (MIS TLIF) can be utilized to achieve lumbar spinal decompression, fixation, and fusion.
– The intent behind this approach, which is still unproven, is to reduce soft-tissue injury, blood loss, recovery time, and length of hospital stay associated with open TLIF.
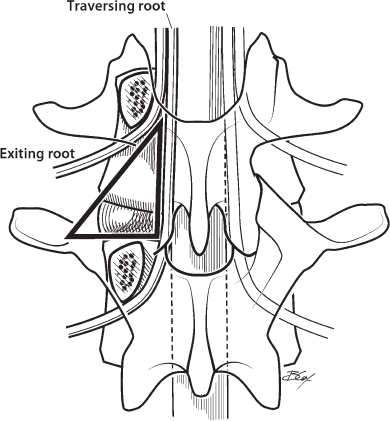
– It is important to recognize the anatomic landmarks at the interpedicular space, referred to as a Kambin triangle: medial (traversing root), lateral (exiting root), and base (inferior pedicle)
II. Indications
Harms first described the transforaminal lumbar interbody fusion (TLIF) technique for circumferential fusion in 1982 using an interbody spacer and a supplemental pedicle screw construct.1 This procedure was a departure from the traditional posterior lumbar interbody fusion (PLIF) in that the TLIF required only a unilateral facetectomy and a single interbody cage. TLIF then became popular due to the lower rates of nerve root injury given the reduced surgical manipulation of neural elements, and it was also found to be effective for revision surgery because the midline dural sac did not have to be exposed.
A minimally invasive approach for accomplishing the TLIF procedure was subsequently developed.2 This technique utilized the advantages of expandable working tubes and percutaneous pedicle screw technology to reduce the soft-tissue injury that has been documented to result from open surgery.3 Although no class I evidence exists to demonstrate the superiority of MIS TLIF over open TLIF, comparative studies suggest a trend toward reduced postoperative pain, hospital length of stay, infection rates, and blood loss.4 MIS TLIF can generally be applied in all situations where an open TLIF can be used.
– Single-or two-level degenerative disc disease with correlative clinical symptoms
– Spondylolisthesis less than Meyerding grade III
– Recurrent lumbar disc herniation
– Spondylosis with radiculopathy and back pain
– Focal spinal deformity concentrated at less than three intersegmental levels
– Synovial cysts exhibiting spinal instability
III. Technique
There are several variations of the MIS TLIF technique. Here a standard approach is described that has been successfully utilized by numerous surgeons.
– The patient is positioned prone on a Jackson operating room table, which offers several advantages. The location of the incision is targeted under fluoroscopy, and two paramedian skin incisions are made between 3 and 4 cm lateral to the midline. Sharp incision of the fascia allows for blunt finger dissection between the longissimus and multifidus muscles along a modified Wiltse plane (Fig. 53.1).5 This not only minimizes trauma to muscular tissues but also minimizes intraoperative bleeding and creates a natural plane that allows for efficient maintenance of the trajectory of the retractors. The approach, if unilateral, is taken from the side where decompression is most necessary.
– Tubular dilator retractors are then placed through this plane and the level confirmed with fluoroscopy. Monopolar cautery is then used to clear any muscle tissue over the facet joint, making sure to expose the lateral aspect of the joint.
– Once the surgeon has confirmed the location of the pars and the lower pedicle, a quarter-inch osteotome or high-speed burr is used to remove the facet joint. Either a partial or complete facetectomy can be performed, with greater bone removal for cases with more medial compression. Care must be taken not to drill into the pedicle. After facet removal the lateral aspect of the ligamentum flavum is visualized. This is resected until the lateral thecal sac is seen (Fig. 53.2). Autograft bone is saved for later grafting purposes.
– Further decompression can then be performed as needed, with removal of ipsilateral ligamentum flavum, decompression under the pars, or contralateral decompression. This is best achieved by angling the retractors more medially. Alternatively, bilateral decompression can be accomplished through dual ports placed on each side.
– After palpation of the caudal pedicle and confirmation of the location of the exiting and traversing nerve roots, the annulus is incised, followed by aggressive intervertebral disc removal and end plate preparation, as with the open technique. This is followed by intervertebral cage placement.
– The neural elements are reinspected. If a posterolateral fusion is desired, the dura is covered with Gelfoam (Pfizer, New York) and the lateral facets and transverse processes are decorticated with a drill. This is followed by bone graft application.
– Supplemental pedicle screw placement can then be accomplished either using a mini-open technique (through the re-tractor with visualization) or percutaneously before or after the decompression. For the mini-open method, the screw placement is very similar to open TLIF. Various methods are used for percutaneous targeting, including (1) AP only, (2) the owl’seye en face approach, (3) biplanar fluoroscopy, and (4) image guidance. All percutaneous methods involve placement of a joshed needle into the pedicle, followed by the use of a cannulated awl and tap to create a screw entry tract. Finally, screw placement and rod tunneling are used to connect the construct components.
– A drain is not typically used.

Fig. 53.1 Axial magnetic resonance image (MRI) showing the modified Wiltse plane between the longissimus and multifidus muscles. High MRI signal can be seen along this plane between the muscles, giving direct access to the facet joints.
IV. Complications
– Cerebrospinal fluid (CSF) leakage is uncommon with these procedures because the dural exposure is limited to those areas that are to be decompressed directly. Dural repair can be difficult. Some surgeons have advocated leaving the durotomy unrepaired and applying a collagen sponge locally, which suggests that the limited dead space reduces the risk of CSF leakage postoperatively.
– Incomplete neural decompression is more problematic than in open surgery given the small working corridor. Care must be taken to visualize critical landmarks to ensure that any compression (such as at a far lateral disc) is adequately addressed. The critical landmarks include the caudal pedicle, pars interarticularis, and lateral ligamentum flavum.
– Nerve root injury is best avoided by maintaining an appreciation of the medial-lateral location in which the surgeon is working. Careful identification and control of the exiting and traversing nerve roots prior to discectomy is critical.
– Cage misplacement occurs most frequently when inadequate disc material has been removed or the bony end plate has been violated. Care in end plate preparation is essential to minimize graft settling. In addition, it is desirable that the cage cross the midline, and this can be confirmed with fluoroscopy.
– Screw misplacement is most commonly the result of poor targeting technique. Thus, close familiarity with one technique for ensuring that the pedicle is not breached is essential. The anteroposterior (AP) targeting techniques are excellent for preventing neural injuries.
– Pseudarthrosis can be minimized but never totally prevented. Proper end plate preparation, cage sizing, and the use of osteobiologic adjuvants will limit this complication. In addition, attention to postoperative nutrition, bracing, and external electrical bone stimulation are helpful.
V. Postoperative Care
Care after surgery is the same as with open TLIF. Patients should be rapidly mobilized with physical therapists, with external bracing as a treatment option. Muscle spasm occurs more commonly with MIS procedures and is best treated with muscle relaxants and benzodiazepines, as opposed to narcotics.
VI. Outcomes
Proper patient selection is vital for achieving excellent outcomes. Although MIS TLIF has not been conclusively shown to be superior to open TLIF, several reports suggest this pattern. In a well-selected population, radiculopathy will show meaningful improvement in 80 to 95% of cases; axial back pain will improve in 70 to 85% of cases.
VII. Surgical Pearls
– In cases where substantial muscle creeps under the edges of the retractor, consider pharmacologic paralysis. Also consider removing the retractor and making a longer fascial opening, followed by placement of a deeper retractor.
– When performing a contralateral neural decompression, leave the ipsilateral ligamentum flavum intact at first. This will push the thecal sac ventrally, keeping it out of the way while the contralateral work is being performed.
– Intervertebral disc can be removed efficiently using an insert-and-rotate scraper. These devices allow entry into collapsed disc spaces and also effectively remove any disc herniations causing neural compression.
– Self-distracting cages, usually with a “bulleted” nose, will allow the placement of larger interbody cages, as it is difficult to use pedicle screw manipulation of a laminar spreader to open the disc space in MIS surgery.
Common Clinical Questions
1. MIS TLIF is utilized because it is believed to result in all of the following except:
A. Decreased soft-tissue damage
B. Higher fusion rates
C. Shorter hospital stays
D. Reduced blood loss
2. One of the critical maneuvers to reduce neural injury is:
A. Remove more facet bone so that less nerve retraction is needed
B. Use of intraoperative intravenous steroids
C. Stronger pedicle screw fixation
D. Repair of dural tears
3. When placing intervertebral cages in a MIS TLIF it is important to:
A. Make sure the cage is higher than 13 mm
B. Make sure the cage is longer than 27 mm
C. Use only nondegradable interbody devices
D. Cross the midline
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







