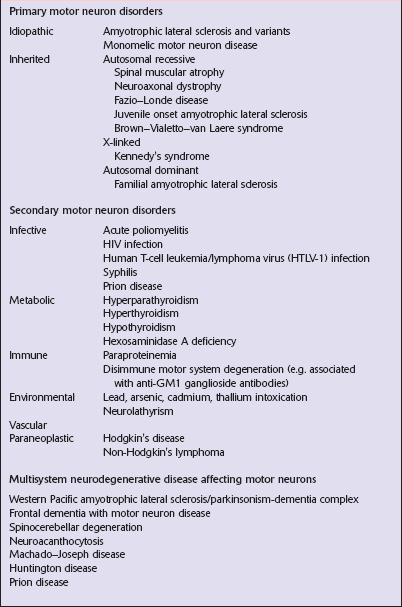
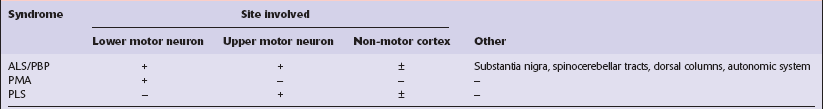
27 Diseases that affect motor neurons can be classified as either primary, secondary, or multisystem (Table 27.1). The terms ‘motor neuron diseases’ and ‘motor neuron disorders’ are used to refer to any disease affecting motor neurons. The specific term ‘motor neuron disease’ is used in Europe as a synonym for amyotrophic lateral sclerosis (ALS) and related disorders. ALS, progressive bulbar palsy (PBP), and progressive muscular atrophy (PMA) are generally considered to be variants of a single clinicopathologic syndrome. Primary lateral sclerosis (PLS) is regarded by many workers as a distinct entity because there is no involvement of lower motor neurons. These conditions (Table 27.2) are characterized as follows: Clinical criteria for diagnosis divide cases into definite and probable ALS (Table 27.3). Since several diseases can be associated with motor neuron loss, secondary causes of motor neuron disease must be excluded. Table 27.3 Revised World Federation of Neurology criteria for diagnosis of ALS The diagnosis of ALS requires: a. Evidence of LMN degeneration by clinical, electrophysiological or neuropathological examination; b. Evidence of UMN degeneration by clinical examination; c. Progression of the motor syndrome within a region or to other regions, as determined by history or examination; and Four diagnostic categories are recognized: 1. Clinically definite ALS: on clinical grounds alone, evidence of UMN plus LMN signs in the bulbar region and in at least two spinal regions, or the presence of UMN signs in two spinal regions and LMN signs in three spinal regions 2. Clinically probable ALS: on clinical grounds alone, UMN plus LMN signs in at least 2 regions with some UMN signs rostral to LMN signs 3. Probable, laboratory supported ALS: this is defined, after proper application of neuroimaging and clinical laboratory protocols has excluded other causes, as: a. clinical evidence of UMN and LMN signs in only one region; or b. UMN signs alone in one region and LMN signs defined by EMG criteria in at least two limbs 4. Possible ALS is defined, once other diagnoses have been excluded, as: The category of suspected ALS, previously included in the El Escorial criteria has been discarded UMN, upper motor neuron; LMN, lower motor neuron; ALS, amyotrophic lateral sclerosis. The anterior nerve roots may appear shrunken and gray when compared with the posterior sensory roots (Fig. 27.1). The spinal cord may be atrophic. In most instances, the brain is macroscopically normal, but in a small proportion of cases, the precentral gyrus appears atrophic (Fig. 27.2). In patients with dementia, the frontal and temporal lobes may be atrophied. 27.1 Spinal cord from patients with ALS. The most characteristic finding is loss of motor neurons and astrocytosis in the spinal cord, brain stem, and motor cortex (Fig. 27.3). The remaining motor neurons in the spinal cord and brain stem may show cytoskeletal abnormalities. 27.3 Loss of neurons in ALS. Inclusion bodies (Figs 27.4–27.8) may be seen in sections stained with hematoxylin and eosin (H&E) (Fig. 27.4), but the distinctive inclusions are more readily visualized by immunostaining for ubiquitin or P62 (Fig. 27.5). Inclusions are seen in both sporadic and familial ALS. In many patients with motor neuron disease there is aggregation and mislocation of the protein TDP-43. Normally located in the nucleus (Fig. 27.7) the protein accumulates in the cytoplasm and forms inclusions in disease (Fig. 27.8). More rarely, ALS of juvenile onset is associated with the formation of cytoplasmic aggregates of FUS (fused-in-sarcoma) protein, another protein normally located in the nucleus. 27.4 Neuronal inclusion bodies in ALS.
Motor neuron disorders
CLASSIFICATION
AMYOTROPHIC LATERAL SCLEROSIS (ALS)
 ALS is a neurodegenerative disorder affecting upper and lower motor neurons, and can be associated with variable pathology of non-motor systems.
ALS is a neurodegenerative disorder affecting upper and lower motor neurons, and can be associated with variable pathology of non-motor systems.
 PBP is a syndrome of progressive dysarthria and dysphagia. Approximately 25% of patients who later develop other features of ALS initially present with PBP.
PBP is a syndrome of progressive dysarthria and dysphagia. Approximately 25% of patients who later develop other features of ALS initially present with PBP.
 PLS is a condition in which upper motor neuron signs occur in the absence of lower motor neuron signs, and pathologic changes are restricted to the motor cortex and corticospinal tracts.
PLS is a condition in which upper motor neuron signs occur in the absence of lower motor neuron signs, and pathologic changes are restricted to the motor cortex and corticospinal tracts.
 PMA is a condition in which lower motor neuron signs correlating with a loss of anterior horn cells occur in the absence of upper motor neuron signs, and in which the upper motor neurons are preserved.
PMA is a condition in which lower motor neuron signs correlating with a loss of anterior horn cells occur in the absence of upper motor neuron signs, and in which the upper motor neurons are preserved.
MACROSCOPIC APPEARANCES


(a) Cervical spinal cord. The upper motor (anterior) roots appear normal while the lower cervical anterior roots are severely atrophic. (b) Thoracolumbar spinal cord showing extensive atrophy of the anterior nerve roots.
MICROSCOPIC APPEARANCES
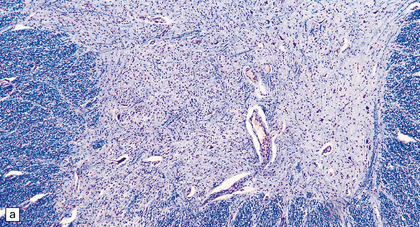
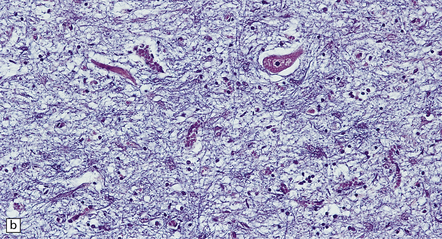
(a) Marked depletion of neurons from the anterior horn of the spinal cord. (b) Loss of neurons and gliosis of the hypoglossal nucleus.
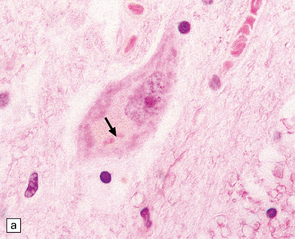
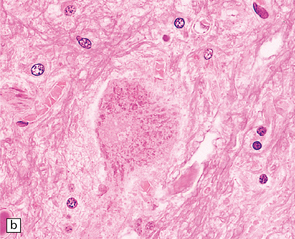
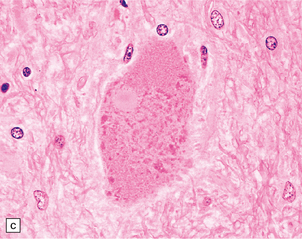
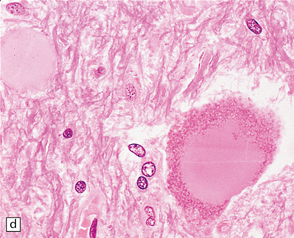
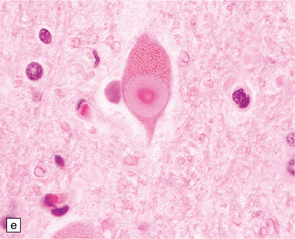
(a) Bunina bodies (arrow) are small eosinophilic inclusions, 2–5 μm in diameter. They are often arranged in small beaded chains and are sparse in most ALS cases. (b) Motor neuron containing a small hyaline inclusion. (c) This motor neuron contains a small spherical hyaline inclusion. (d) Many hyaline inclusions appear as large homogeneous bodies that displace the Nissl substance. (e) Uncommon inclusions superficially resemble the Lewy bodies seen in Parkinson‘s disease but do not contain alpha synuclein.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Motor neuron disorders
Only gold members can continue reading. Log In or Register to continue