Figure 1-1 A-D, Sequential steps in performance of fascicular nerve biopsy described in text.
(Modified from Dyck PJ, Lofgren EP. Method of fascicular biopsy of human peripheral nerve for electrophysiologic and histologic study. Mayo Clin Proc 1966;41(11):778–84.)
Symptoms from fascicular nerve biopsy
This was reported in an addendum from the medical article cited in the previous section.
Since this paper was submitted, one of the authors (P.J.D.) has himself had fascicular biopsy of the left sural nerve—for the purpose of obtaining normal nerve. Several subjective observations follow: During transection of the nerve fascicles isolated for biopsy, and without direct injection of local anesthetic agent into the nerve, a sharp, electric-like, painful, prickling sensation developed just below the lateral malleolus and persisted for a few seconds. On the third day after transection, and reaching a plateau during the second week after biopsy, the following symptoms occurred: (1) with stretching of the sciatic nerve, as occurs with flexion of the trunk with the knees extended, a rather intense, prickling, burning pain developed on the lateral surface of the heel which was promptly relieved on bending the knees or extending the trunk; (2) a light jabbing, prickling, and burning discomfort of short duration passed into the same area of the heel when the first two or three steps were taken after the subject arose from a sitting position; and (3) at rest, while he was sitting or lying down, an occasional light jabbing sensation occurred in the anesthetic area. This area was approximately 1 1/2 inches in diameter and was just below the lateral malleolus. These symptoms did not interfere in any way with work or sleep and disappeared during the third and fourth postoperative weeks.
Historic descriptions of magnetic resonance imaging—targeted fascicular nerve biopsy
Dyck PJB, Spinner RJ, Amrami KK, Klein CJ, Engelstad JK, Dyck PJ. Targeted fascicular biopsy of proximal nerves with MRI abnormality may be diagnostically informative. Presented at the 56th Annual Meeting of the American Academy of Neurology, San Francisco, CA, 2004.
With permission from the American Academy of Neurology we quote our submitted abstract.
Objective: To assess the utility of fascicular proximal nerve biopsies from sites of MRI abnormality of roots, plexus or limb nerves in selected patients with unexplained neuropathies.
Background: Nerve biopsies are usually taken from distal cutaneous sites because these nerves lie superficially, are purely sensory and are more affected in most polyneuropathies. However occasionally, we have performed fascicular nerve biopsies from proximal sites in focal nerve lesions.
Design/Methods: With improved resolution of MRI, experience in recognizing abnormal images and specialization of surgeons, we are now assessing the diagnostic yield of targeted fascicular nerve biopsy from roots, plexus and proximal limb nerves.
Results: Twenty-nine patients (15 men and 14 women) with unexplained neuropathy and abnormal MRIs of proximal limb nerves, plexus or roots were identified. Their mean age was 46.7 years (SD 18.5, range 12 to 76). Clinically, 16 patients had lower-limb mononeuropathies affecting 19 limbs (18 sciatic and 1 tibial); 5 patients had brachial plexus neuropathies; and 3 had lumbosacral radiculoplexus neuropathies. All had increased T2 signal and 27 of 29 had enlargement within the affected nerve segment. The MRI abnormality was in the sciatic (15 patients, 18 nerves), cauda equina (8), brachial plexus (5), and tibial (1) nerves. In 4 sciatic cases, the MRI involvement extended into the lumbosacral plexus. Whole distal cutaneous nerve biopsy (12 sural), fascicular mixed nerve biopsy (13 sciatic, 1 tibial and 5 brachial plexus), and rootlet biopsy (8 lumbar) were obtained. Ten patients had proximal after distal nerve biopsy, whereas 17 had only proximal and 2 had only distal nerve biopsy. The biopsies showed inflammatory demyelination (11), B-cell lymphoma (5), perineuroma (5), inflammatory/vasculitis (4), granuloma (2), angiofibrolipoma (1), and non-diagnostic (1). The distal biopsies showed specific pathologic alterations in 2 of 12, whereas the proximal biopsies showed specific changes in 26 of 27. Although proximal nerve biopsy is a major surgery requiring general anesthesia, neuropathic side effects were few (no patients had new weakness and 1 had problematic sensory loss).
Conclusions: (1) MRIs can identify focal nerve lesions but to date do not reliably identify the underlying pathological processes; (2) in selected cases, nerve biopsies at sites of imaging abnormality provide specific diagnostic information not identified in distal nerve and, despite being invasive, may be justified because of therapeutic implications; and (3) because of potential morbidity, proximal nerve biopsy should only be performed in medical centers with special expertise in peripheral nerve imaging, nerve surgery and nerve pathology.
Dyck PJB, Spinner RJ, Amrami KK, Klein CJ, Engelstad JK, Dyck PJ. Targeted fascicular biopsy of proximal nerves with MRI abnormality may be diagnostically informative. J Peripheral Nerv Syst 2007; 12 (Suppl 1):27–8.*
With permission from the Peripheral Nerve Society, we quote our submitted abstract.
Background: Nerve biopsies are usually taken from distal cutaneous sites. With improved resolution of MRI, we are now assessing the diagnostic yield of targeted fascicular nerve biopsy from proximal nerves.
Methods: One hundred and thirty-eight patients (68 male and 70 female) with unexplained neuropathy and abnormal MRIs of proximal limb nerves, plexus or roots were identified. Their mean age was 48.8 years (range 3 to 77) and 12 were children. Clinically, 59 patients had mononeuropathies, 39 brachial plexopathies, 12 lumbosacral radiculoplexus neuropathies, 29 polyradiculopathies, 6 cranial neuropathies, and 1 multiple mononeuropathy (8 had combinations of neuropathy). All 138 cases had abnormal nerve MRI studies. Whole distal cutaneous nerve biopsy (31) and proximal fascicular nerve biopsy (130; 69 mixed sensorimotor, 35 brachial plexus, 28 lumbar rootlet, 1 proximal cutaneous and 1 cranial) were obtained. Twenty-two had both proximal and distal, 108 had only proximal and 8 had only distal nerve biopsy.
Results: Overall, 115 of 138 patients (83%) had biopsies with meaningful or diagnostic pathology of which 85 (74%) were potentially treatable. Pathological diagnoses included: inflammatory demyelination (42), perineuroma (15), vasculitic (12), lymphoma (12), metastatic tumor (10), injury neuroma (4), vascular malformation (4), amyloidoma (2), Schwannoma (2), radiation injury (2), other (10) and non-diagnostic (23). The distal biopsies were diagnostic in 11 of 31 (35%), whereas the proximal biopsies were diagnostic in 109 of 130 (84%) (p<0.0001). Neuropathic side effects were few.
Conclusions: We conclude: (1) In highly selected cases, proximal nerve biopsies at sites of MRI abnormality provide specific diagnostic information not identified in distal nerve; (2) despite being invasive, proximal biopsies may be justifiable because of therapeutic implications; (3) MRIs can localize focal nerve lesions but to date do not reliably identify the underlying pathological process and (4) because of potential morbidity, proximal nerve biopsy should only be performed in medical centers with special expertise in peripheral nerve evaluation, imaging, surgery and pathology.
CASE REPORTS
Case A
A 30-year-old man with a history of Hodgkin’s disease 19 years earlier and treated twice with radiation and chemotherapy developed recurrent facial numbness and weakness (responsive to prednisone), transitory diplopia, and 2 years of progressive left footdrop, leg pain, and nerve conduction and electromyography (EMG) findings in keeping with a diagnosis of left sciatic nerve or lumbosacral plexus involvement. Magnetic resonance imaging (MRI) studies of his spine were reported to be normal.
We performed MRI evaluation of the lumbosacral plexuses and thighs using gadolinium. As shown in Figure 1-2 (see the arrows), the lumbosacral plexus and the upper sciatic nerve, especially of the left side, displayed an abnormal signal and enlargement. Although an inflammatory process was suspected, it was unclear which type of inflammatory process was involved and whether lymphoma could be confidently excluded. Therefore, a fascicular biopsy of the upper sciatic nerve was obtained and was found to be in keeping with a granulomatous process (sarcoidosis) (Fig. 1-3). The findings were not that of Hodgkin’s disease or that of an inflammatory demyelinating polyneuropathy. The patient was treated with prednisone for sarcoidosis.
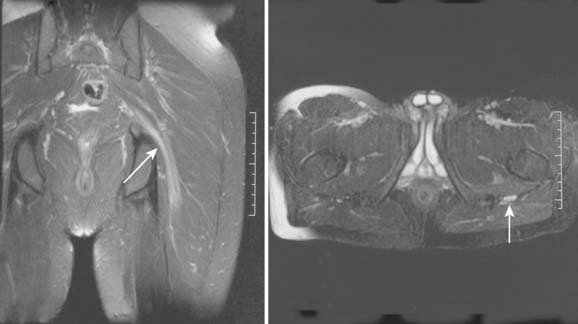
Figure 1-2 Shown are T2-weighted fast spin echo images with fat suppression—on the left, coronal, and on the right, axial planes of Case A. Arrows show areas of enlargement and increased signal of the sciatic nerve.
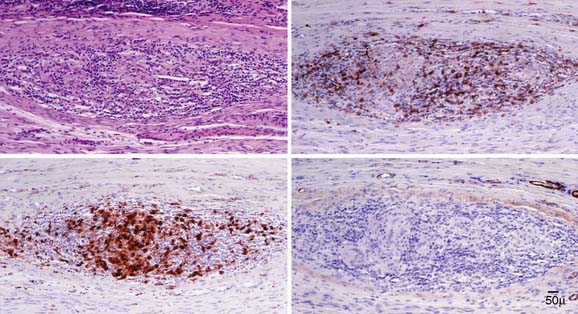
Figure 1-3 Serial longitudinal paraffin sections from the patient (Case A) with a sciatic neuropathy-lumbosacral plexus neuropathy that shows a large nerve granuloma from a targeted sciatic nerve fascicular biopsy. Upper left (H&E) shows a large perivascular epineurial inflammatory infiltration with lymphocytes and epithelioid cells. Upper right shows CD45 reactivity (common leukocyte antigen) of the lymphocytes, and lower left shows reactivity of the epithelioid cells (macrophages) to CD68. Lower right shows smooth muscle actin reactivity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








