A diagnosis of brachial plexopathy was considered but deemed unlikely on clinical grounds. Even though weakness can be confined to the distribution of an individual nerve in both the inherited and sporadic forms of brachial neuritis, the onset of the illness tends to be painful, and sensory symptoms are generally present. Hereditary neuropathy with liability to pressure palsies can present with a mononeuropathy, but conduction slowing is at compression sites and sensory symptoms are common. Chronic inflammatory demyelinating multiple mononeuropathy is associated with sensory symptoms and more widespread demyelinating electrophysiologic findings.
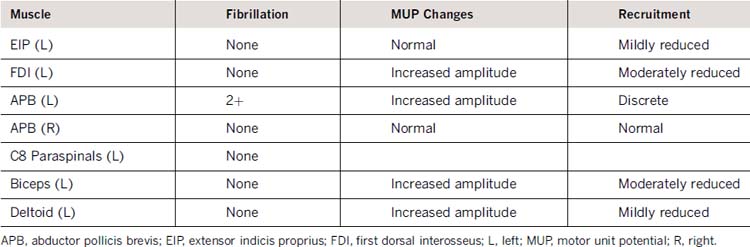
In our patient, weakness in the left arm was most consistent with multiple mononeuropathies; for example, there was profound weakness in the median innervated thenar muscles, but ulnar muscles innervated by the same spinal segment were normal. On the right, weakness was restricted to muscles innervated by the posterior interosseous and peroneal nerves. Electrophysiologic changes were restricted to motor fibers of the left median nerve, with sparing of the sensory fibers, and without widespread demyelinating changes or conduction slowing at sites of entrapment. Therefore, a tentative diagnosis of MMNWOCB was made, and the patient was treated with intravenous immunoglobulin (IVIg) at a dose of 2 g/kg per month for 3 months with normalization of strength in all the weak muscles. Three months after the last IVIg treatment, weakness returned, and the patient was again treated effectively with IVIg. Over the ensuing 8 years, she has remained stable but dependant on IVIg and the dose had been gradually tapered to 0.4 g/kg every 4 weeks.
CONCLUSIONS
The consensus criteria for MMN6 require the presence of CB in two or more motor nerves outside common entrapment sites. Our patient did not meet these criteria and yet responded to treatment. This indicates that patients with multiple motor neuropathies without CB can respond to immunomodulatory treatments.
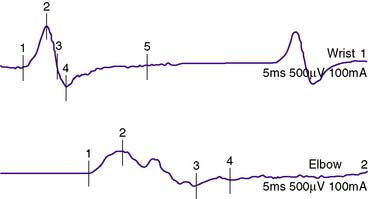
Patients diagnosed with MMNWOCB may indeed have CB that is not obvious with routine testing such as very proximal CB at the nerve root or plexus level. Furthermore, axon loss presumably secondary to prior focal demyelination, may preclude confident diagnosis of CB because segmental amplitude change in low-amplitude motor responses can occur as a result of phase cancellation. In our case, a segmental amplitude decrement with mild dispersion of the proximal response was seen in the median nerve in the forearm, suggesting demyelination, even though CB could not be confirmed and motor conduction velocity was normal. This suggests that the primary pathology was demyelination and that CB was present but at sites that were not amenable to routine motor nerve conduction studies. In one study, transcranial magnetic stimulation using the triple stimulation technique revealed a proximal focal CB in four of 10 patients with MMNWOCB,7 and in another study, six of nine patients had temporal dispersion or CB after magnetically stimulating nerve roots before and after 1 minute of maximal voluntary contraction (magnetic fatigue test).8 These studies suggest that the electrophysiologic differences between these two entities may be superficial and that they may differ only in the location or severity of CB.
Further evidence that weakness in patients with MMNWOCB is secondary to covert focal demyelination (CB) is the rapid response to treatment that can be seen in some patients; in our patient, strength returned to normal after 3 months of IVIg. Although some cases can be purely axonal,9 demyelinating features (conduction slowing or temporal dispersion)5,10 are seen in the majority of cases. It has been suggested that GM1 antibodies and CB are more prevalent in patients who respond to IVIg than in nonresponders,11 but others suggest that the clinical presentation, GM1 antibody positivity and IVIg responsiveness are identical in patients with or without CB. In our experience, patients without CB do not respond as favorably to treatment as patients with CB. The relative refractoriness in patients with MMNWOCB may be related to longer disease duration and more widespread axonal degeneration.10
It is important to recognize that patients with multifocal pure motor neuropathies do not always have demonstrable CB and yet may respond satisfactorily to immunomodulatory treatment. Consequently, absence of CB should not preclude a trial of immunotherapy. The mainstay of diagnosis is meticulous clinical examination to identify weakness in a peripheral nerve distribution that when confluent can be misinterpreted as being segmental. We believe that MMNWOCB and MMN share common pathophysiologic mechanisms and are different manifestations of the same underlying disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree