Multilobar Resections and Hemispherectomy
Devin K. Binder
Johannes Schramm
Introduction
Multilobar resection and hemispherectomy are surgical options available for the treatment of medically intractable seizures arising from a diffuse area of epileptogenicity that remains unilateral but extends beyond one lobe. The nature and extent of the underlying pathologic process, the patient’s neurologic status, and the results of preoperative neurophysiologic and neuroimaging studies together determine which surgical procedure should be recommended.
For clarity, hemispherectomy and multilobar resections are presented separately in this chapter.
Hemispherectomy
Historical Perspectives
The term hemispherectomy refers to a variety of operations that functionally isolate the cerebral cortex of one hemisphere from the rest of the nervous system. In 1928, Dandy24 and L’Hermite59 originally described hemispherectomy for diffuse infiltrative glioma, but in the next decade few other reports of hemispherectomy for tumor were published.40 Ten years later, McKenzie performed the first hemispherectomy for epilepsy.69 In 1950, Krynauw reported on hemispherectomies in 12 children with infantile hemiplegia and intractable epilepsy.58 In this report, he noted excellent seizure control as well as marked and long-lasting behavioral improvement.
Because of the success of the operation for improving seizure control and behavior, hemispherectomy became widely used in the treatment of seizures associated with infantile hemiplegia. In addition, it came into use for the treatment of other unihemispheric syndromes associated with intractable epilepsy, such as Sturge-Weber disease, Rasmussen encephalitis, and cerebral infarct. By 1961, White reviewed 267 cases from many neurosurgical centers.113 However, enthusiasm for hemispherectomy waned in the 1960s as more effective anticonvulsants became available and as significant long-term complications became apparent. Many patients developed delayed neurologic and intellectual deterioration postoperatively, and ultimately it became clear that hemorrhage, superficial cerebral hemosiderosis (SCH), and resultant mass effect and hydrocephalus were responsible, and even caused significant mortality.33,42,74,83
Over the next two decades, modifications to anatomic hemispherectomy were proposed, aimed at eliminating the late complications of SCH and hydrocephalus. The Oxford-Adams modification involved occlusion of the foramen of Monro with a muscle plug and stripping down the dura to reduce the subdural space.1,7 Peacock et al. routinely implanted a shunt system into the subdural cavity.78 Rasmussen developed a new technique termed functional hemispherectomy that involved a large central resection, temporal lobectomy, callosotomy, and fronto- and parieto-occipital disconnection.82 This procedure improved seizure control while maintaining a low incidence of SCH. Other approaches removed only the cortex, termed hemidecortication or hemicorticectomy.48,52,115
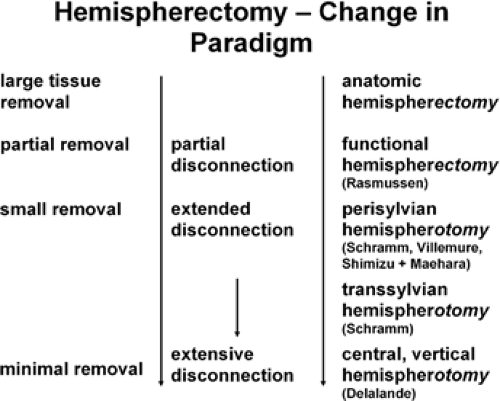
Over the past 10 to 15 years, there have been further development and modification of functional hemispherectomy techniques, including hemispheric deafferentation,89,90 peri-insular hemispherotomy,107 dorsal transcortical subinsular central hemispherotomy,26,109 Shimizu and Maehara’s variation,94 and the transsylvian keyhole functional hemispherectomy88,91 (Table 1). All of these procedures are aimed at less resection and more disconnection, increasing the safety of the procedure and reducing postoperative complications. The improved safety of these modifications and the improvements in neuroimaging and neurophysiologic monitoring have made hemispherectomy a more attractive option for patients with intractable unihemispheric epilepsy.
Role of Pathology
Typical pathologies leading to diffuse unihemispheric disease and intractable epilepsy include neonatal injury, vascular insults, hemimegalencephaly, hemispheric cortical dysplasia and other neuronal migration disorders, Sturge-Weber syndrome, and Rasmussen encephalitis.34,100 One group of patients has experienced the acute onset of a massive insult resulting in a fixed neurologic deficit. These include those with infantile hemiplegia resulting either from posttraumatic brain injury or vascular insults.12,58 A second group of patients has malformations of cortical development (MCD), which vary in severity from focal cortical dysplasias to hemispheric cortical dysplasia and hemimegalencephaly.16,53,102,108,110 In these patients, neurologic manifestations are often delayed or progressive. Another group of patients has Sturge-Weber syndrome (encephalotrigeminal angiomatosis).32,45,72 Characterized by a facial port wine stain (nevus flammeus) and pial angiomatosis, patients develop intractable epilepsy associated with impaired cognitive development and hemiparesis. A final group has acquired progressive neurologic deterioration with intractable epilepsy. The prototype for this is Rasmussen encephalitis. In 1958, Rasmussen et al. first described this chronic childhood encephalitis that leads to intractable epilepsy and neurocognitive deficits.84 In this disease, the presentation may be delayed but the disease course, once established, is inexorably progressive.
Table 1 Hemispherectomy Techniques | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Role of Functional Localization
Impact of Electrophysiologic Studies
The primary goal of electrophysiologic studies is to lateralize the disease to the radiographically and clinically abnormal hemisphere. Typically, a detailed investigation with both ictal and interictal recordings is performed. Most often, interictal surface electroencephalograms (EEG) show a clearly asymmetric tracing with abnormal slowing, low background voltage, and multifocal independent sharp waves and spikes over the affected hemisphere.96 In specific disorders, there may be characteristic EEG abnormalities; for example, in hemimegalencephaly, the EEG may demonstrate hemihypsarrhythmia.75,99
The other important goal is to determine whether there are abnormalities in the “good” hemisphere. Bilateral independent epileptogenic foci are associated with a poor prognosis for seizure control.14,96,118 In a study of 12 patients, Carmant et al. demonstrated that a good outcome from hemispherectomy was associated with interictal EEG suppression over the abnormal hemisphere, absence of contralateral slowing, absence of generalized discharges, and absence of bilateral independent spiking.14 In a study of 28 patients, Doring et al. found that 75% had bilateral EEG abnormalities preoperatively, which was more common in patients with MCD than with acquired lesions.29 Notably, 77% of patients with acquired lesions became seizure free, compared with only 47% of patients with MCD. Thus, the presence of bilateral EEG abnormalities alone does not preclude consideration for hemispherectomy.
In general, the EEG will lateralize well with structural imaging abnormalities. For hemispherectomy, accurate lateralization and not intrahemispheric localization is most important. In cases without radiographic lateralization, of course, both surface EEG and, when necessary, invasive EEG monitoring play a critical role in both lateralization and localization.
Impact of Neuroimaging
Structural neuroimaging plays an integral role in the preoperative evaluation of the hemispherectomy candidate. The advent of computed tomography (CT) imaging in the 1970s permitted direct visualization of the “good” and “abnormal” hemispheres. While CT can still provide important information (e.g., calcification in Sturge-Weber syndrome), magnetic resonance imaging (MRI) has become the study of choice, as it provides excellent visualization of structural abnormalities in the cerebral cortex and subcortical white matter. It also provides a high-resolution assessment of the “good” hemisphere.
Structural imaging may reveal the severity of disease in vascular or posttraumatic hemispheric injury, from atrophy to porencephalic cysts. Atrophy, characterized by loss of gray and white matter and the presence of an enlarged ventricle, is encountered in most conditions and may be of varying degree, depending on the severity or chronicity of the underlying disease process. In Sturge-Weber syndrome, CT and plain films may show “tram-track” hemispheric calcification, and gadolinium-enhanced MRI demonstrates pial angiomatosis.67,68 In hemimegalencephaly, structural imaging shows marked enlargement of the affected hemisphere with abnormal thickening of the cortical mantle.35,50,116 High-resolution structural MRI showing both large and subtle cortical abnormalities has also revolutionized the diagnosis of MCD.4,63 Early MRI may be useful in the diagnosis of Rasmussen encephalitis,17,61 but definitive diagnosis requires the appropriate clinical picture together with biopsy demonstrating perivascular lymphocytic cuffing and gliosis.8,9,36,43,84
Functional imaging may also be incorporated into the evaluation of the hemispherectomy candidate. For example, positron emission tomography (15O-PET) can be useful to follow disease progression, either with hemimegalencephaly,85 Sturge-Weber syndrome,19,60,79 or Rasmussen encephalitis.17,61 Diffuse unilateral interictal hypometabolism of the affected hemisphere is most commonly found. Single photon emission computed tomography (SPECT) scanning, which provides information regarding cerebral blood flow, may show hypoperfusion in the affected hemisphere.15,17,18 In one study of seven patients undergoing hemispherectomy, the six patients with unilateral preoperative SPECT findings all had a favorable outcome regardless of the surface EEG.15 Functional studies are most important in cases without lateralizing findings on structural imaging studies.
Frequency of Use
Hemispherectomy is primarily a pediatric operation, as perinatal, congenital, and early developmental pathologies account for the majority of conditions leading to intractable unihemispheric epilepsy. In 1993, of 47 surveyed epilepsy surgery centers, 29 were performing hemispherectomies; hemidecortication was advocated in three, the anatomic technique in four, and functional hemispherectomy in 22.97 In an extensive multicenter study of 333 hemispherectomies from 11 centers published by Holthausen et al. in 1994, distribution of etiologies was as follows: 31% hemispheric dysplasia, 25% Rasmussen encephalitis, 14% vascular, 13% hemiatrophy, 8% Sturge-Weber, and 8% other.47 Surgical techniques included functional hemispherectomy (33%), “Adams modification” (18%), hemidecortication (18%), hemispherotomy (17%), and anatomic hemispherectomy (13%). With the introduction of modern functional hemispherectomy techniques with reduced risk and postoperative complications,88 and as patients are offered the benefit of the operation earlier in life, it is expected that the number of centers and hemispherectomy cases will increase.
Indications
The indications for hemispherectomy include damage to one hemisphere accompanied by medically intractable epilepsy and accompanying neurologic deficits. As described above, etiologies include extensive hemispheric dysplasia, hemimegalencephaly, Sturge-Weber disease, Rasmussen encephalitis, and perinatal infarction. One group of patients presents with a maximal hemispheric deficit, with contralateral hemiplegia and hemianopsia, usually due to a fixed perinatal insult. The other group presents with intractable epilepsy associated with progressive neurologic deterioration, most often due to a pathology that will evolve ultimately into a maximal hemispheric deficit (e.g., Rasmussen encephalitis).
Hemispherectomy is contraindicated if preoperative evaluation fails to demonstrate that ictal activity arises from the affected hemisphere. Usually, the history of medically intractable epilepsy often with lateralizing semiology is combined with evidence of extensive hemispheric involvement on high-quality MRI and further lateralization and localization with inpatient video-EEG seizure monitoring. Furthermore, hemispherectomy is not employed if less extensive surgical therapy (callosotomy or focal or multilobar resection) may potentially be effective.
Evaluation Criteria
Evaluation of whether and when to recommend hemispherectomy relies on seizure characteristics, neurologic examination, language evaluation, EEG and imaging findings, and the natural history of the associated pathologic process.
Seizure Characteristics
Hemispherectomy candidates may have a variety of seizure types and severity, including drop attacks, focal motor seizures, complex partial seizures, epilepsia partialis continua, and generalized seizures. The seizures are frequent and severe enough to be incapacitating in daily activities; typically, patients will have 10 to 200 seizures per day. In around 80% of patients, a partial motor seizure pattern appears to predominate as a clinical manifestation. Epilepsia partialis continua is characteristic of chronic encephalitis, whereas infantile spasms appear related to a variety of etiologies.
The seizures must truly be medically intractable for a patient to be considered for hemispherectomy. Therapeutic trials of different antiepileptic drugs (AEDs), alone or in combination, should be attempted by a neurologist expert in AED management strategies. However, continued unsuccessful trials of many different AEDs must be balanced against the potential benefits of early surgery in individual cases.
Neurologic Examination
In addition to intractable epilepsy, these patients typically present with other findings of unilateral hemispheric damage, including impairment of cortical sensory modalities, hemianopsia, hemiplegia, and spasticity. Often they are able to walk and movement of the arm is often more impaired than that of the leg. Fine motor control (pincer grasp) is often absent, but gross motor control (e.g., handgrip) may be preserved. In these cases, no new motor deficit is created by hemispherectomy; occasionally, there may be immediate postoperative hypotonia and loss of voluntary movements that may last a few days to a few weeks. Postoperative completion of hemianopsia is unavoidable and should be part of informed consent, but is not considered an absolute contraindication to hemi-spherectomy.
Language Evaluation
Preoperative language function depends on whether the dominant hemisphere is affected and the severity of disease progression. The younger the age of injury, the more likely language transfer to the healthy hemisphere will occur. Thus, the potential for postoperative language deficits depends on the timing of transfer of language function, and incomplete transfer of language function is a relative contraindication to hemispherectomy. Older children with dominant hemisphere disease and some language function should undergo assessment of lateralization of language (e.g., with the intracarotid amobarbital [Wada] test). The “worst-case scenario” is late appearance of progressive disease (e.g., Rasmussen encephalitis) in the dominant hemisphere; these patients may have severe language deficits following dominant hemispherectomy.
Electroencephalography and Imaging Findings
As described above, there is usually a concordance between EEG abnormalities and a structurally abnormal hemisphere as seen on preoperative imaging studies. In a significant number of cases, however, EEG abnormalities may be recorded from the good hemisphere, either secondary to or independent of the abnormalities of the diseased hemisphere.47 Bilateral abnormal EEG findings do not represent an absolute contraindication to hemispherectomy, as they may reflect secondary epileptogenesis and disappear after surgery. An explanation for the presence of independent epileptic activity recorded from the good hemisphere should be taken into account during the decision-making process for hemispherectomy.
Etiology, Natural History, and Timing of Surgery
Three aspects of the etiology and natural history of the condition may affect timing of surgery: Whether the condition is congenital or acquired, whether it is strictly unilateral or possibly bilateral, and whether it is static or progressive. Congenital pathologies such as large porencephaly resulting from in utero or perinatal insult or the Sturge-Weber syndrome, which are usually strictly unilateral, have a better prognosis with surgery than a congenital lesion such as hemimegalencephaly or hemispheric dysplasia, which may be associated with some degree of contralateral involvement. Acquired unilateral pathology, such as Rasmussen encephalitis, has a better prognosis than infectious processes, which usually have bilateral involvement.
Timing of surgery is determined by the severity of epilepsy, the age of the patient, the natural history of the disease, and the adequacy of therapeutic trials of anticonvulsant medications. Hemispherectomy before the second or third year of life carries no risk of increasing deficit and is therefore ideal in those cases that present early for diagnosis and evaluation. In later-onset cases (e.g., Rasmussen encephalitis in older children), timing is controversial; while complete transfer of language and motor function to the healthy hemisphere is less likely to occur in older children, nevertheless, the intractable seizures can produce neuropsychological deterioration and may prompt earlier surgery. Evidence is accumulating that seizures themselves as opposed to the pathologic substrate may significantly delay cognitive and psychosocial development.49,64,87 In certain conditions (e.g., inborn brain malformations) leading to catastrophic infantile epilepsy, very early surgery may be optimal; in our experience, hemispherectomy can be performed safely at 4 months of age.
Goals of Surgery
The primary goal of hemispherectomy is to achieve seizure control via complete disconnection of the epileptogenic abnormal
hemisphere from the “good” hemisphere. In anatomic hemispherectomies, this was accomplished by extirpation of the affected hemisphere. In functional hemispherectomies, the emphasis is on complete disconnection rather than resection, although some tissue is resected in each of the current variations of functional hemispherectomy.
hemisphere from the “good” hemisphere. In anatomic hemispherectomies, this was accomplished by extirpation of the affected hemisphere. In functional hemispherectomies, the emphasis is on complete disconnection rather than resection, although some tissue is resected in each of the current variations of functional hemispherectomy.
The classic anatomic hemispherectomy involved a large T-shaped skin incision along the midline down to the temporal base; hemicraniotomy; occlusion of the anterior and middle cerebral artery and parasagittal veins; interhemispheric callosotomy and frontobasal disconnection; disconnection of insular cortex and temporal stem; and removal of the hemisphere en bloc or in lobes. Total anatomic hemispherectomy was associated with severe intraoperative hemorrhage, hypotension, early and late hydrocephalus, and SCH.25,33,42,44,74,83,88,104 Development of hydrocephalus necessitated shunting in ∼50% of patients. SCH typically developed after 8 to 15 years and led to progressive neurologic deterioration, increased intracranial pressure, and death in many cases.33,42,74,83
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree