Introduction
Neonatal seizures may represent the first, and perhaps only, clinical sign of a central nervous system (CNS) disorder in the neonate. They prompt immediate concerns related to their etiologic diagnosis and management and future concerns relevant to the long-term outcomes of those who experience them. Our traditional understanding of neonatal seizures continues to evolve. It was recently believed that neonatal seizures, although easily provoked by acute injury in the immature brain, imparted little or no permanent anatomic or physiologic sequelae. Current research in both animal models and humans challenge this traditional view, and it is now believed that neonatal seizures may leave a permanent mark on the developing CNS.
Despite recent basic and clinical research of neonatal seizures there still remain considerable gaps in knowledge in areas that relate to diagnosis, pathophysiology, etiology, therapy, and prognosis. Although such work continues, the clinician is left with the task of developing strategies in diagnosis and management with limited scientifically confirmed data. The following discussion is based on both the best available data and, in their absence, clinical practice. This discussion has in part been presented elsewhere and is now updated and expanded.31,113,114,119
Controversies related to the characterization and classification of neonatal seizures have for the most part been definitively addressed. However, data relating to treatment and prognosis have not. While the debate continues in the basic neuroscience literature as to whether and how seizures cause significant brain injury in the developing brain, even less information is available concerning whether these findings are applicable to human newborns and whether the degree of injury, if present, is clinically significant. Resolution of these issues will ultimately guide antiepileptic drug (AED) therapy in neonates and more clearly define factors that predict long-term outcome.
The more practical approach is to consider the notion that the overriding determinant of outcome is seizure etiology. Seizure occurrence may indicate the presence of a potentially treatable etiology and should prompt an immediate search for this cause and institution of appropriate therapy. Seizures themselves may require emergent therapy because they may, directly or indirectly, disrupt the infant’s homeostasis or contribute to additional brain injury. Seizure occurrence, and particularly the type of seizures, may have predictive value in determination of outcome.
The approach to the clinical management of an infant thought to have experienced a seizure is defined by the orderly consideration of issues that will improve long-term outcome: Accurate seizure characterization and classification, maintenance of infant homeostasis, urgent search for a treatable etiology, appropriate application of electroencephalography, institution of etiologic-specific treatment, thoughtful consideration of acute and then chronic AED treatment, and consideration of risk factors that predict outcome in order to plan for long-term care.
Definitions
The use of the term “seizure” to describe paroxysmal clinical events in the neonate represents a unique challenge. Early clinical investigations assumed that all such events were of epileptic origin; that is, such clinical events were generated by coincident electrographic seizures, composed of abnormal, excessive hypersynchronous discharges of networks of cortical neurons. Later studies suggested that, although most clinical seizures can be viewed in this way, some may be generated by nonepileptic mechanisms. Although it is appropriate to generically call all abnormal paroxysmal clinical events “seizures,” more detailed classification can relegate most of them to either epileptic or nonepileptic categories. These distinctions become most important clinically when considering AED therapy. However, the terms also become cumbersome in discussing neonatal “seizures” as a whole. Thus, in the discussions that follow, the term “neonatal seizures” will generally encompass those events of epileptic origin. There are, however, a few exceptions that will be specified.
The definition of an electrographic seizure also becomes important. This will be discussed in detail later. In brief, it is an abnormal electrical ictal event consisting of evolving, rhythmic activity of at least 10 seconds’ duration—with or without accompaniment of a clinical seizure.
Definitions of the age of the infant are also relevant, since they provide a measure of the degree of brain maturation. The neonatal period is defined as the first 4 weeks (28 days) of life. Legal age (LA) refers to the number of weeks the baby has been alive since birth. Estimated gestational age (EGA) refers to the duration of pregnancy prior to birth. The gestational age plus the chronologic age defines the age since conception or conceptional age (CA). The CA is a useful metric that benchmarks brain maturation, regardless of whether the infant was born prematurely or at term. Thus, the electroencephalogram (EEG) of 1-week-old (LA), 39 weeks EGA infants (CA of 40 weeks) should match that of a premature baby of EGA 34 weeks who is now 6 weeks old (LA).
Epidemiology
The neonatal period is one of greatest periods of seizure hazard during the human life span. The incidence of seizure occurrence is greatest in childhood,77,182 especially in the first month of life. Reported incidence rates of neonatal seizures range from 1.5 to 5.5 per 1,000 neonates10,51,147,148,153,172 depending on the study methodologies and the populations investigated. Most neonatal seizures first appear within the first week of life.87 It has also been suggested that seizure incidence varies with specific risk factors such as birthweight, degree of illness, and possible etiology. Lanska et al.87 reported “seizure” occurrence, based solely on clinical recognition, to be greatest in preterm or low-birth-weight infants compared with term infants. They reported an incidence of clinically
suspected seizures in all neonates to be 3.5 per 1,000, but 57.5 per 1,000 in very–low-birth-weight (<1,500 g) infants, 4.4 per 1,000 in low-birth-weight (1,500–2,499 g) infants, and 2.8 per 1,000 in normal-birth-weight (2,500–3,999 g) infants. Scher et al.158,159 reported that seizures occurred in 3.9% of neonates of less than 30 weeks’ conceptional age and 1.5% in neonates older than 30 weeks. Similarly, Kohelet et al.82 found an overall incidence of seizures in a cohort of very–low-birth-weight infants to be 5.6 per 1,000. However, the incidence of 57.5 per 1,000 in very–low-birth-weight infants reported by Lanska et al.87 may be skewed by the inclusion of nonepileptic clinical events in the very premature population studied.
suspected seizures in all neonates to be 3.5 per 1,000, but 57.5 per 1,000 in very–low-birth-weight (<1,500 g) infants, 4.4 per 1,000 in low-birth-weight (1,500–2,499 g) infants, and 2.8 per 1,000 in normal-birth-weight (2,500–3,999 g) infants. Scher et al.158,159 reported that seizures occurred in 3.9% of neonates of less than 30 weeks’ conceptional age and 1.5% in neonates older than 30 weeks. Similarly, Kohelet et al.82 found an overall incidence of seizures in a cohort of very–low-birth-weight infants to be 5.6 per 1,000. However, the incidence of 57.5 per 1,000 in very–low-birth-weight infants reported by Lanska et al.87 may be skewed by the inclusion of nonepileptic clinical events in the very premature population studied.
The International League Against Epilepsy (ILAE) has used the terms “acute reactive” or “symptomatic” to describe the trigger of most neonatal seizures. The ILAE has also designated unprovoked neonatal epileptic syndromes: Benign neonatal convulsions, benign familial neonatal convulsions, early myoclonic encephalopathy (EME), and early epileptic encephalopathy (EIEE).32,33,114,182 Acute reactive or symptomatic seizures are very frequent, whereas, in contrast, the occurrence of specific neonatal epileptic syndromes, as defined by ILAE, are rare.
Clinical Features
Ictal Features
Seizures in the neonate have clinical features that are unique compared with those occurring in older infants and children. Such features include: Fragmentation, disorganization, unusual patterns of spread, and simultaneous, but asynchronous multiple regions of involvement. Some of these differences are based on mechanisms of epileptogenesis and the state of early development in the immature brain. Other differences are based on the relative importance of nonepileptic mechanism of “seizures” generation in this age group. Some similarities also are noted between neonatal seizures and those of older infants and children. These include the types of movements that characterize the events, such as clonic, tonic, and myoclonic seizures.
A number of methods have been used to classify neonatal seizures: According to clinical features, the relation between clinical seizures and electrical seizure activity on the EEG, seizure pathophysiology, and epileptic syndromes. Each classification has some clinical utility, and each provides some further insight into the clinical problems of diagnosis and management.
Clinical Classification
Efforts over the years to characterize and classify neonatal seizures49,94,117,150,152,156,189,190,196 demonstrate an evolution of thought and also underscore the importance of the ground-breaking work of French investigators reported over 40 years ago.49 Early classification schemes focused on the differences between neonatal seizures and those of older children: Neonatal seizures were reported to be clonic or tonic, not tonic–clonic, and, when the seizures were focal, they were characterized as unifocal or multifocal. Later classifications included myoclonus.150
Early investigators also identified clinical events that had less of a traditional organization of motor activity, considered an important distinction between seizures of the neonate and older children.49,111,152 These seizures were initially characterized as “anarchic”49 and later as “subtle”189 or “minimal.”94 These descriptions included events of oral-buccal-lingual movements such as sucking and chewing; movements of progression, such as bicycling of the legs and swimming movements of the arms; and random eye movements. Although these events were initially considered to be epileptic in origin, others later suggested that they were exaggerated reflex behaviors and referred to them as “brainstem release phenomena” or “motor automatisms.”117 Table 1 lists the clinical characteristics of neonatal seizures according to a current classification scheme.118 This scheme can be applied through clinical observation of the neonate. The basic classification includes seizures characterized as: Focal clonic, focal tonic, myoclonic, spasms, generalized tonic, and motor automatisms (also referred to as “subtle seizures”).
Paroxysmal changes related to the autonomic nervous system have also been reported to be manifestations of seizures. These events include alterations in heart rate, respiration, and blood pressure as well as flushing, salivation, and pupillary dilation.53,58,98,196,197 Any of these findings occurring as isolated epileptic events are rare. When they do occur, they do so most consistently in association with other clinical manifestations of seizures.117
Classification According to Temporal Relation to Electrical Seizure Activity
Although the classification scheme just described is based on the clinical characteristics of the seizures, other codification schemes consider the temporal relation of clinical events to the occurrence of electrical seizure activity on EEG. An “electroclinical” seizure occurs when the clinical event overlaps in time with electrographic seizure activity. A seizure is referred to as “clinical only” when it occurs in the absence of any EEG seizure activity. A seizure is referred to as electrographic “only” if the electrical seizure occurs without any coincident clinical seizure activity.
Table 1 Clinical characteristics, classification, and presumed pathophysiology of neonatal seizures | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||
Classification According to Pathophysiology
Seizures may also be classified according to their pathophysiology: Epileptic or nonepileptic in character (Table 2). This was suggested by Mizrahi and Kellaway,117 who reported their findings of neonates experiencing seizures during video-EEG monitoring. These authors classified neonatal seizures based on clinical characteristics, the relation between EEG and clinical events, and also on presumed pathophysiology. They suggested that a group of behaviors, previously referred to as “subtle” seizures, had features more consistent with reflex phenomena rather than epileptic seizures. They demonstrated that the paroxysmal clinical events in some could be provoked by tactile stimulation of the infant; that the intensity of the response could be proportional to the intensity of the stimulus (both in terms of intensity at a single site of stimulation or consistent intensity with increasing sites of stimulation); that the response could spread to regions of the body distant from the site of stimulation; and that the clinical events could be suppressed by restraint of the infant. These were considered features of reflex behaviors.
When the concept of nonepileptic seizures is discussed in the literature, the absence of electrical seizure during clinical seizure activity is strongly emphasized by some.191 These discussions speculate that electrical seizure discharges can be generated in “deeper” cortical or even subcortical regions and thus may not be visible by conventional EEG recorded at the scalp surface. Data from human adults and mature animal studies are provided to support this concept. Although this possibility cannot be discounted in human neonates, there is no supportive evidence of its occurrence. In addition, ictal single photon emission computed tomography (SPECT) performed in neonates with “nonepileptic” events (brainstem release phenomenon) have failed to demonstrate the characteristic hyperperfusion
hallmark of genuine epileptic seizures.7 Finally, the lack of associated EEG seizure activity is not the only finding that suggests a nonepileptic pathophysiology; rather, the similarity of the events to the experimental models of reflex behaviors provides additional compelling data (Table 3).
hallmark of genuine epileptic seizures.7 Finally, the lack of associated EEG seizure activity is not the only finding that suggests a nonepileptic pathophysiology; rather, the similarity of the events to the experimental models of reflex behaviors provides additional compelling data (Table 3).
Seizures of Epileptic Origin
Current research reveals that some clinical seizures can be confidently classified as epileptic in origin based solely on their clinical characteristics. Some seizures may be confidently classified as “epileptic” in nature just by their clinical appearance. The clinical events that are most clearly epileptic in origin are: Focal clonic, focal tonic, some types of myoclonic seizures, and spasms (Tables 1 and 2). These seizure types can be recognized and characterized at the bedside by the visible features of the spontaneous event. In addition, during the event, the clinician can attempt to suppress the motor behavior by holding the affected limb; a continuation of rhythmic muscle contractions indicates the epileptic basis of the event. These seizures occur in close association with EEG seizure activity, and the clinical event cannot be provoked by stimulation nor suppressed by
restraint of the infant. When EEG is utilized, seizures character- ized as electrical-only seizures are also considered, by definition, epileptic in origin. Specific features of the developing brain enhance acute seizure initiation, maintenance, and propagation. Similar factors promote a greater predisposition to epileptogenesis, the development of long-term, postnatal epilepsy in the wake of acute, reactive neonatal seizures. These properties include enhanced cellular excitation, enhanced synaptic excitation, and a tendency to promote propagation of an epileptic discharge.62,68,121,144,161,179
restraint of the infant. When EEG is utilized, seizures character- ized as electrical-only seizures are also considered, by definition, epileptic in origin. Specific features of the developing brain enhance acute seizure initiation, maintenance, and propagation. Similar factors promote a greater predisposition to epileptogenesis, the development of long-term, postnatal epilepsy in the wake of acute, reactive neonatal seizures. These properties include enhanced cellular excitation, enhanced synaptic excitation, and a tendency to promote propagation of an epileptic discharge.62,68,121,144,161,179
Table 2 Classification of neonatal seizures based on electroclinical findings | |||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Seizures of Nonepileptic Origin
Other seizures are best considered as nonepileptic in origin.77,117 Clinical events classified as nonepileptic in origin include some types of myoclonic events, generalized tonic posturing, and motor automatisms such as oral-buccal-lingual movements, movements of progression, and some ocular signs (Tables 1 and 2). These events occur in the absence of electrical seizure activity, but more importantly, have clinical characteristics similar to reflex behaviors. These clinical events can be provoked by stimulation of the infant. Both the provoked and spontaneous events can be suppressed by restraint or by repositioning the infant during the event. In addition, the clinical events may increase in intensity with the increase in the repetition rate of stimulation (temporal summation) or the sites of simultaneous stimulation (spatial summation).
Table 3 Reflex physiology demonstrated in animal models compared with generalized tonic seizures and motor automatisms (so-called nonepileptic) seizures in human neonates | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
Syndromic Classification
Most neonatal seizures are classified as acute reactive or symptomatic by the ILAE.3,33,182 They occur as a consequence of a specific external trigger, such as hypoxic ischemic encephalopathy.120 However, four specific neonatal epileptic syndromes also are identified by the ILAE. Two are relatively innocuous: Benign neonatal convulsions and benign familial neonatal convulsions; two others are associated with poor outcomes: Early myoclonic encephalopathy5 and early epileptic encephalopathy.128 The syndromes of neonatal seizures are discussed in detail in the following sections. A discussion also is included concerning other disorders that may have a consistent constellation of findings that may also suggest syndromic classification, including epilepsy in focal cortical dysplasia in infancy.97
Interictal Feature
Neonates who have experienced seizures have no typical clinical features, except for those with specific epileptic syndromes as defined by ILAE (these will be discussed in detail later).
However, clinical interictal findings in individual infants are significant. The interictal state of consciousness will vary depending on the etiology of the seizures, from alert to comatose. Often, these clinical findings may suggest cause and prognosis. The state of alertness usually correlates with the EEG background activity. In addition, focal neurologic signs may suggest focal brain lesions. Dysmorphic features may suggest genetic or developmental etiologies.
However, clinical interictal findings in individual infants are significant. The interictal state of consciousness will vary depending on the etiology of the seizures, from alert to comatose. Often, these clinical findings may suggest cause and prognosis. The state of alertness usually correlates with the EEG background activity. In addition, focal neurologic signs may suggest focal brain lesions. Dysmorphic features may suggest genetic or developmental etiologies.
Postictal Features
Clinical and electroencephalographic postictal features are also not consistent. Usually, few, if any, postictal changes are present, particularly in neonates with more benign etiologies. They enjoy a rapid return to their baseline clinical and electrographic state. Prolonged focal paralysis is unusual and, if present, should suggest a structural brain lesion. In addition, a prolonged altered state of conscious is also unusual following individual neonatal seizures. Infants with severe acute encephalopathies often have abnormal levels of tone, activity, and awareness before seizures with little noticeable change in the postictal state.
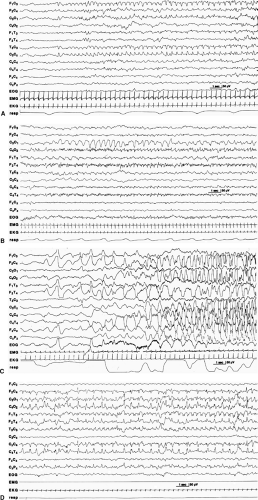 FIGURE 1. Electrical seizure activity may be varied in frequency, morphology, voltage, and onset. A: Rhythmic sharp waves in the left central region, remaining confined to that region (2-week-old, 40-week gestational age). B: Rhythmic sharp and slow wave activity in the left occipital region (6-day-old, 40-week gestational age). C: High-voltage, repetitive, slow, sharp waves arising in the right frontal region, later appearing as faster and sharper activity spreading to the right central region (3-day-old, 40-week gestational age). D: Initial rhythmic, moderate-voltage, sharp-wave activity arising in the right central-temporal region, which remains unchanged as another seizure arises independently from the left temporal region with a complex morphology (2-day old, 39-week gestational age). From Mizrahi EM, Kellaway P. Diagnosis and Management of Neonatal Seizures. Philadelphia: Lippincott-Raven: 1998:181, with permission.118 |
Electroencephalographic Findings
The EEG is the most important laboratory examination to assist in the diagnosis of neonatal seizures. However, its application differs in the neonate when compared with older children and adults.
Interictal Findings
Interictal Focal Abnormalities
Focal sharp waves may be present interictally in the neonatal EEG, but are not considered epileptiform. Some focal sharp waves are normal, developmentally determined findings, such as frontal sharp transients (encoches frontales) and temporal sharp waves that occur randomly, that are low or moderate in voltage, and are present in transitional or light sleep.116 Focal sharp waves that are persistent, excessively numerous, high amplitude, present in wakefulness and sleep, and have complex morphology suggest focal injury. Multifocal sharp waves may suggest diffuse dysfunction, such as might occur in meningitis or hypoglycemia. Focal spikes may suggest focal injury, such as localized stroke, or may have uncertain diagnostic significance.73 In the neonate, interictal focal sharp waves and spikes are not considered direct evidence or confirmation that an individual has had or will have electrographic seizures. A similar conundrum arises in some older infants and children. A small percentage of nonepileptic infants have an incidental finding of interictal spikes or sharp waves. In others, unmistakable seizures can arise from an interictal background that lacks identifiable spikes or sharp waves.
Interictal Background EEG
The degree of abnormality of the interictal background activity may provide information concerning the extent and type of CNS dysfunction associated with seizures. The nature of the interictal background activity may also suggest the risk individual infants have in experiencing a seizure.88 Infants with initial normal background activity are less likely to eventually experience electrographic seizures than are those with persistent diffuse background abnormalities. In addition, the extent, degree, evolution, and rate of resolution (if any) of background EEG abnormalities can suggest prognosis. An EEG with normal background activity recording within the first 24 hours of life may suggest a good outcome,72 whereas EEG background activity with abnormal features that persist or resolve slowly suggests a poorer outcome.73
Ictal Findings
Although not clearly defined, it appears that electrical seizure activity in neonates is rare before 34 to 35 weeks. As previously noted,87 suspected clinical seizures are reported with great frequency in very–low-birth-weight infants, but few of these have confirmed simultaneous EEG ictal patterns. When electrical seizure activity is recorded, its manifestations on EEG can vary widely.116,135,156 Frequency, voltage, and morphology of the seizure discharges may change within an individual seizure, between seizures in an individual infant, or among infants (Fig. 1). The minimum duration has been designated to be 10 seconds,28 but the duration of seizure discharges varies widely. The electrical events are predominantly focal and well circumscribed. They frequently arise from the central or centrotemporal region of one hemisphere and less commonly in the occipital, frontal, or midline central regions (Fig. 1). Although seizures may arise focally and remain confined to that region, they may also spread to other regions (Fig. 2): As a gradual widening of the focal area, by an abrupt change from a small regional focus to involvement of the entire hemisphere (a finding that characterizes a hemiconvulsive seizure), or by migration of the electrical seizure from one area of a hemisphere to another or from one hemisphere to another.118
Unique Neonatal Ictal Patterns
Two ictal patterns are relatively unique to the neonatal period; both are typically associated with severe encephalopathies and their associated abnormal background EEG. Seizure discharges of the depressed brain are typically low in voltage, long in duration, and highly localized (Fig. 3).77 They may be unifocal or multifocal and show little tendency to spread or modulate. They are typically not associated with clinical seizures, even in the untreated infant. Seizure discharges of the depressed brain occur when the EEG background is depressed and undifferentiated, and their presence suggests a poor prognosis.
α-Seizure activity is characterized by a sudden appearance of paroxysmal, rhythmic activity of the α frequency (8–12 Hz), typically in the temporal or central region.80,197,199 This pattern may evolve from the more typical seizure discharges or may appear de novo. As with seizure discharges of the depressed brain, clinical events usually do not occur with α-seizure discharges. The presence of an α-seizure discharge usually indicates the presence of a severe encephalopathy and poor prognosis (Fig. 4). Electrical seizure activity that is persistently focal may be consistent with a focal lesion in the corresponding region,97 for example focal cortical dysplasia (Fig. 5).
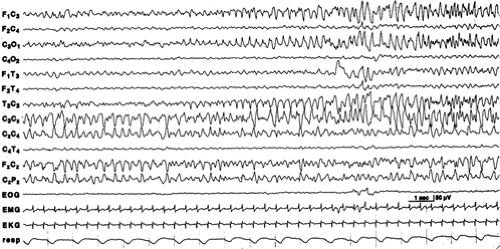 FIGURE 2. Migration of electrical seizure activity that begins in the midline region (CZ) and shifts to the left central region (C3) as the CZ region becomes less involved. This EEG was recorded from a 4-day-old, 40-week gestational age female infant with hypoxic–ischemic encephalopathy and suppression-burst EEG background. No clinical seizures were present during the electrical seizure activity. From Mizrahi EM, Kellaway P. Diagnosis and Management of Neonatal Seizures. Philadelphia: Lippincott-Raven: 1998:181, with permission.118 |
Video-EEG Monitoring
Video-EEG monitoring is a powerful tool in the diagnosis and management of neonatal seizures and initially had been the basis of clinical investigations that addressed seizure classification, therapy, and prognosis.17,21,30,112,117 It is becoming increasingly more available at many centers for routine use, and is more widely employed in neonatal intensive care units.27 However, its increasing popularity should not detract from the fact that attended EEG can provide important clinical information, when the recorded infant is observed by a trained
electroneurodiagnostic technologist (ENDT) who can carefully observe an infant’s behavior and characterize the events.
electroneurodiagnostic technologist (ENDT) who can carefully observe an infant’s behavior and characterize the events.
Computer-Assisted EEG Analysis of Neonatal Seizures
Computer-assisted analysis of EEG to detect and quantify electrical seizure activity has been utilized reliably in long-term EEG monitoring of older children and adults in epilepsy monitoring units. EEG seizure detection in neonates is more challenging because of variability of the electrographic events. More recently, such programs have been developed and may provide reliable data, particularly if the recordings are attended by a trained ENDT.59,122 There has also been renewed interest in the use of cerebral function monitors (CFMs), such as amplitude integrated EEG (aEEG), to detect neonatal seizures.63,162,185 This technique is limited in terms of its ability to provide data from all brain regions and its reliance on nonexpert health care professionals. A recent study reports that, using CFMs, up to 50% of neonatal seizures were misclassified or unrecognized.146 However, advocates suggest that the ability to monitor specific brain regions for long periods may, in some ways, balance the limited localization capability of the technique.44 Another recent study examined 851 electrographic neonatal seizures detected in 125 conventional, full-array EEG recordings. A one-channel EEG (C3 → C4) was digitally created to simulate the contemporary use of single-channel EEGs for seizure detection by CFMs.165 Although 78% of the seizures were visible in the single-EEG channel, the seizures were briefer and lower in amplitude, and less than half were diagnosed by aEEG based on the C3 → C4 channel.
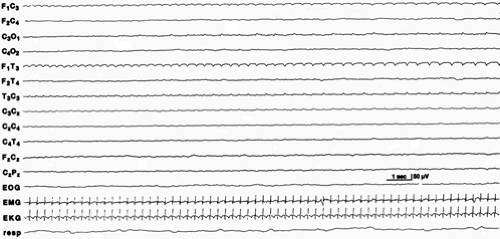 FIGURE 3. Seizure discharge of the depressed brain in the left temporal region occurring in the EEG of a 2-day-old, 38-week gestational age female infant with hypoxic–ischemic encephalopathy. The EEG background is depressed and undifferentiated. No clinical seizures ac-companied the electrical seizure activity. From Mizrahi EM, Kellaway P. Diagnosis and Management of Neonatal Seizures. Philadelphia: Lippincott-Raven: 1998:181, with permission.118 |
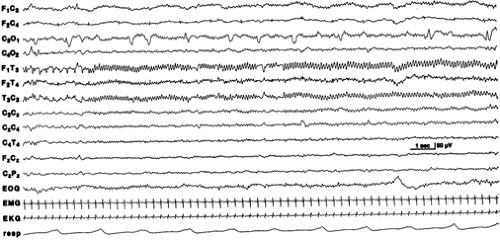 FIGURE 4. α-Seizure discharge in the left temporal region is characterized by sinusoidal 10- to 11-Hz rhythmic activity that evolved from rhythmic sharp-wave activity. There is also an independent, repetitive, slow, sharp transient in the left occipital region. The EEG background activity is depressed and undifferentiated. This EEG is recorded from a 4-week-old, 38-week gestational age male infant with pneumococcal meningitis. No clinical seizures occurred with these electrical seizure discharges. From Mizrahi EM, Kellaway P. Diagnosis and Management of Neonatal Seizures. Philadelphia: Lippincott-Raven: 1998:181, with permission.118 |
Diagnostic Considerations
Etiology
The occurrence of neonatal seizures indicates the presence of CNS disease and, in clinical practice, prompts a thorough evaluation for etiology and, if found, the institution of etiologic-specific therapy. A large number of potential causes exist for neonatal seizures. This, coupled with the susceptibility of the immature brain to injury may account for the high incidence of acute neonatal seizures and chronic postnatal epilepsy in this population. Although the list of potential etiologies is extensive,118 most causes can be broadly categorized as hypoxia–ischemia, metabolic disturbances, CNS or systemic infections, and structural brain lesions. Table 4 lists the most
frequently identified etiologies of neonatal seizures in the order of their relative occurrence.
frequently identified etiologies of neonatal seizures in the order of their relative occurrence.
Symptomatic Neonatal Seizures
The presence of hypoxic–ischemic encephalopathy (HIE) can be difficult to establish because diagnostic criteria have not been uniformly established or accepted. In addition, some proposed criteria have been so restrictive that infants with encephalopathy may not meet all of them but still carry the diagnosis of “suspected HIE.” In other proposed schemes, the criteria are too lenient and may not predict the occurrence of long-term neurologic sequelae.123,134 The American College of Obstetricians and Gynecologists, in association with the American Academy of Pediatrics, have provided guidelines for HIE diagnosis.34 At some centers, current practice is directed toward identification of measures of asphyxia that have predictive value in the occurrence of long-term sequelae.137 This strategy has resulted in less restrictive criteria for HIE. Both approaches, however, include the tabulation of delivery room Apgar scores, blood gases, need for resuscitation, recognition of clinical aspects of encephalopathy including seizures, and confirmation of multisystem involvement. There is also an emerging discussion of the use of computer-assisted analysis of EEG, including aEEG, to aid in the staging of the severity of HIE,163 although this is still considered investigational.
Metabolic disturbances ranging from electrolyte imbalances to inborn errors of metabolism may also be associated with neonatal seizures. This category of etiologies represents an important group of potentially treatable disorders and include hypocalcemia, hypomagnesemia, and hypoglycemia. Much less frequent is the finding of an inborn error of metabolism, such as an aminoaciduria, urea cycle defect, or organic aciduria. Other rare causes of medically refractory neonatal seizures that are potentially treatable include pyridoxine and biotinidase deficiency and others.
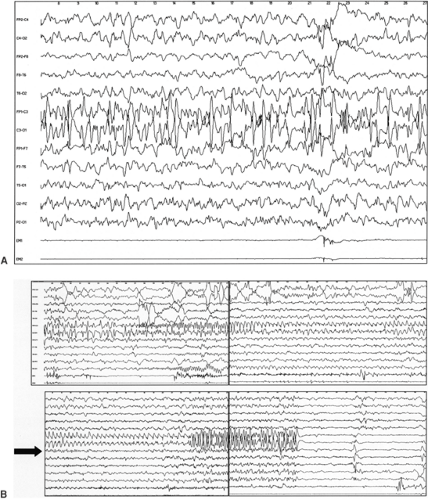 FIGURE 5. Interictal and ictal seizure activity associated with focal cortical dysplasia. A: Interictal high-voltage sharp waves are present in the left central region of this recording of a 1-month-old infant. B: Four sequential and continuous segments of the EEG from the same infant in A demonstrating, in the first panel, the transition from interictal to ictal seizure activity and then the evolution of the electrical seizure all confined to the left central region. (Note in this example post-ictal depression of the EEG occurs, a relatively unusual finding in neonatal seizures). From Lortie A, Plouin P, Chiron C, et al. Epilepsy Res. 2002;51(1–2):133–145, with permission.97 |
Both bacterial and viral agents can be causes of CNS infection in the neonate that are associated with seizures, to the extent that almost all neonates with new-onset seizures are investigated for such infection. Some viral infections, such as herpes simplex encephalitis, may be treated empirically at clinical presentation prior to confirmation of the diagnosis. In addition, prenatal toxoplasmosis, other agents, rubella, cytomegalovirus, herpes simplex (TORCH) infections can be risk factors for neonatal seizures.
Structural brain conditions associated with neonatal seizures include acquired conditions such as stroke or hemorrhage and developmental anomalies of the brain. Congenital brain malformations may range from highly localized focal dysplasias to catastrophic defects such as holoprosencephaly. Some malformations, such as lissencephaly, are associated with specific genetic disorders.
Special circumstances also arise in which neonates may be at risk for seizures, providing opportunities for increased
surveillance and development of preventative therapies. Clancy et al.30 prospectively studied neonates undergoing cardiac surgery that required deep hypothermic circulatory arrest. They found that 19% of all infants with nonhypoplastic left heart syndrome experienced a postoperative acute neurologic event, including seizures and coma.
surveillance and development of preventative therapies. Clancy et al.30 prospectively studied neonates undergoing cardiac surgery that required deep hypothermic circulatory arrest. They found that 19% of all infants with nonhypoplastic left heart syndrome experienced a postoperative acute neurologic event, including seizures and coma.
Table 4 Most frequently occurring etiologies of neonatal seizures | ||
|---|---|---|
|
Prognosis
In clinical practice, the long-term outcome of neonates with seizures is predominantly determined by the etiology underlying seizure onset. However, two other specific issues frequently arise in discussion of prognosis: The possibility that the seizures themselves contribute harm to the developing brain, and the possibility that AED administration may adversely affect the neonate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






