Chapter 9 Nerve Destruction for the Alleviation of Visceral Pain
 Visceral pain is commonly more challenging to treat. It is often more diffuse and poorly localizable.
Visceral pain is commonly more challenging to treat. It is often more diffuse and poorly localizable. Visceral organs are rarely innervated by single localizable nerve structures; most organs, especially the perineal and pelvic structures, have dual or more innervation, resulting in only partial treatment when one innervation source is treated in isolation.
Visceral organs are rarely innervated by single localizable nerve structures; most organs, especially the perineal and pelvic structures, have dual or more innervation, resulting in only partial treatment when one innervation source is treated in isolation. With the development of modern imaging techniques, procedures to provide analgesia to the visceral organs have become low to moderate risk. The majority of catastrophic outcomes associated with neurolytic procedures predated the use of the imaging to visualize the intended structure before administration of neurolytics.
With the development of modern imaging techniques, procedures to provide analgesia to the visceral organs have become low to moderate risk. The majority of catastrophic outcomes associated with neurolytic procedures predated the use of the imaging to visualize the intended structure before administration of neurolytics. Patient selection is one of the most important factors in the success of these procedures in the short and long terms. Neurolysis of visceral nerve fibers is controversial in the nonmalignant (noncancer) population because of legitimate concerns regarding deafferentation pain.
Patient selection is one of the most important factors in the success of these procedures in the short and long terms. Neurolysis of visceral nerve fibers is controversial in the nonmalignant (noncancer) population because of legitimate concerns regarding deafferentation pain. Neurolytic procedures of the visceral nervous system should be considered early in the treatment of cancer patients whose pain is no longer well controlled on moderate doses of analgesics or who are unable to tolerate systemic analgesic medications because of adverse effects.
Neurolytic procedures of the visceral nervous system should be considered early in the treatment of cancer patients whose pain is no longer well controlled on moderate doses of analgesics or who are unable to tolerate systemic analgesic medications because of adverse effects. Neurolytic procedures for visceral cancer pain are an effective adjunctive treatment that can co-occur with other allopathic and alternative analgesic modalities.
Neurolytic procedures for visceral cancer pain are an effective adjunctive treatment that can co-occur with other allopathic and alternative analgesic modalities. Given that there is redundant innervation to many of the visceral organs, it may prove difficult to impossible to alleviate all of a patient’s visceral pain with a single intervention; thus a multimodal approach should be taken with these patients.
Given that there is redundant innervation to many of the visceral organs, it may prove difficult to impossible to alleviate all of a patient’s visceral pain with a single intervention; thus a multimodal approach should be taken with these patients. Celiac plexus blocks will help to alleviate visceral pain in a multitude of organs from the distal third of the esophagus to the descending colon, including the liver, pancreas, gallbladder, stomach, spleen, kidneys, small intestine, large intestine, and adrenal gland.
Celiac plexus blocks will help to alleviate visceral pain in a multitude of organs from the distal third of the esophagus to the descending colon, including the liver, pancreas, gallbladder, stomach, spleen, kidneys, small intestine, large intestine, and adrenal gland. The lumbar sympathetic chain is located just anterolateral to the lumbar vertebral bodies, anterior to the origin of the psoas muscle, and is best approached at L2, L3, or L4. This block is performed for visceral pain from the descending colon, upper portion of the sigmoid colon, and kidneys.
The lumbar sympathetic chain is located just anterolateral to the lumbar vertebral bodies, anterior to the origin of the psoas muscle, and is best approached at L2, L3, or L4. This block is performed for visceral pain from the descending colon, upper portion of the sigmoid colon, and kidneys. The superior hypogastric block is performed at the level of L5 to S1 for treatment of visceral pain of the lower sigmoid colon, rectum, testicles, ovaries, and uterus.
The superior hypogastric block is performed at the level of L5 to S1 for treatment of visceral pain of the lower sigmoid colon, rectum, testicles, ovaries, and uterus. A ganglion impar block is performed for pain in the perineal area. The ganglion impar is where the two sympathetic chains join together and is located retroperitoneally at the level of the sacrococcygeal ligament.
A ganglion impar block is performed for pain in the perineal area. The ganglion impar is where the two sympathetic chains join together and is located retroperitoneally at the level of the sacrococcygeal ligament. The benefits of neurolysis are time limited and patients with non-cancer originated pain may have a life expectancy well past the analgesic effect of the block. This can leave the patient with not only their original abdominal pain but also deafferentation pain, which can be more severe than the original pain.
The benefits of neurolysis are time limited and patients with non-cancer originated pain may have a life expectancy well past the analgesic effect of the block. This can leave the patient with not only their original abdominal pain but also deafferentation pain, which can be more severe than the original pain. A backache in addition to orthostatic hypotension following a celiac plexus block should be assumed to be a retroperitoneal hematoma until proven otherwise, warranting serial hematocrits.
A backache in addition to orthostatic hypotension following a celiac plexus block should be assumed to be a retroperitoneal hematoma until proven otherwise, warranting serial hematocrits. There is some controversy regarding the timing of neurolytic interventional therapy, leaving each individual practitioner to make the final decision. If you place the block early in the disease process you may decrease the likelihood of central or peripheral sensitization and you may decrease the unwanted side effects of high dose opioids. Others argue that these blocks should be performed only when undesirable side effects occur from non-invasive methods (such as opioid management).
There is some controversy regarding the timing of neurolytic interventional therapy, leaving each individual practitioner to make the final decision. If you place the block early in the disease process you may decrease the likelihood of central or peripheral sensitization and you may decrease the unwanted side effects of high dose opioids. Others argue that these blocks should be performed only when undesirable side effects occur from non-invasive methods (such as opioid management). The most common clinical complication after lumbar sympathetic neurolysis is genitofemoral neuralgia, albeit usually transient.
The most common clinical complication after lumbar sympathetic neurolysis is genitofemoral neuralgia, albeit usually transient.Introduction
Visceral pain is a common complaint seen by many different types of physicians, including family medicine, gastroenterologists, oncologists, surgeons, and pain medicine. Visceral pain can be very challenging to diagnose, manage, and treat. This pain can be somatic or visceral in origin, can be related to a malignancy or be noncancer in origin, and is often very diffuse and nonlocalized. Therefore, treatment and management not only depends on the type of pain and its origin but also very often is aimed at the additional factors in the patient’s life exacerbating the pain such as stress and anxiety.1,2
The history provided by the patient involving the description of pain quality and referral pattern will help elucidate the origin of the pain symptoms. Somatic pain is generally described as well localized and constant in nature with an aching or sharp quality. Somatic pain can often be treated with a combination of nonopioid adjuvant analgesics and local pain interventions. Visceral pain is typically described as vague in origin and of a squeezing, deep, pressure-like quality. Visceral pain is a result of organ injury with resulting transmission of pain via fibers that travel with the sympathetic nervous system.3 Visceral pain may result from distention, traction, torsion, ischemia, or abnormal contraction of visceral organs and may result in referred somatic complaints.4 Interventional procedures involving the sympathetic chain may be used to ease the pain of some patients with abdominal malignancies. Finally, neuropathic pain is usually described as a shooting, numbness, tingling, burning type of pain. This type of pain is usually caused by some injury or irritation of the nervous system itself whether it is via direct postsurgical injury or from a tumor encroachment, compression, or invasion of a nerve structure. This type of pain requires a multimodal pharmacological approach, including opioids, tricyclic antidepressants, selective serotonin norepinephrine reuptake inhibitors, and N-methyl-d-aspartate blockers and early aggressive interventional management with spinal cord stimulation; intrathecal medication administration; and, in the case of malignancy-related pain, neurolysis. This chapter focuses on peripheral neurolytic treatment of visceral pain.
Visceral input arrives in the dorsal horn of the spinal cord; lamina I, II and V; and the intermediolateral cell column, sacral parasympathetic nucleus and lamina X.4 Multiple visceral inputs converge at a single site, thus making exact diagnosis of the location of pain difficult and hence the vague symptoms described by patients.1 The signal travels from the dorsal horn of the spinal cord to the spinothalamic, spinoreticular, spinomesencephalic, and spinohypothalamic tract.4 Visceral input terminates in the brain at multiple sites, including the medulla, pons, mesencephalon, hypothalamus, and thalamus,4 and results in activity of the anterior and midcingulate cortex, frontal cortex, parietal cortex, and cerebellum.5 The cortical sites associated with visceral pain have involvement in the affective perception of pain and memory and may account for the preponderance of co-morbidities such as anxiety and depression with visceral pain.
The treatment of visceral pain resulting from malignancy is integral to the overall treatment of patients with cancer, the goals being improvement in quality of life and improved functional status.6 Evidence suggests pain control plays a significant role in cancer survival.7,8 In treating patients with cancer-related pain, a multimodal and multidisciplinary approach involving medical, interventional, psychological, and social support management produces the highest level of patient satisfaction.
Chemical Neurolysis
Chemical neurolysis has been used since the early 1900s when Schloesser used alcohol for the treatment of trigeminal neuralgia.9 In 1919, Kappis10 performed the first neurolytic procedure for the relief of visceral pain when he performed a percutaneous celiac plexus block in the treatment of intractable abdominal pain.9 Many pharmacological agents have been used for neurolysis, including alcohol (ethanol), phenol, glycerol, and hypertonic saline. Nerve destruction depends on the agent, amount, concentration, and rate of injection.9
The neurolytic action of alcohol is produced by the extraction of cholesterol, phospholipids, and cerebrosides and the precipitation of mucopeptides from the nerve and supporting myelin sheath.11 The basal lamina of the Schwann cell sheath remains intact, allowing for new Schwann cell growth, thereby providing the framework for subsequent nerve fiber growth. This framework encourages the regeneration of axons, but only if the cell bodies of these nerves are not completely destroyed.12 The pathway of degeneration is nonselective and can be observed in peripheral nerves and spinal nerve roots after intrathecal injection and in perineural structures (peritoneum, bowel) after peripheral injections.
Phenol is a benzene ring with one hydroxyl group substituted for a hydrogen atom. It is usually prepared by the hospital or compounding pharmacy because it is not commercially available in premixed liquid form; however, this practice has ceased in many hospital organizations because of the complexity of sterile compounding. Phenol is poorly soluble in water and, at room temperature, forms only a 6.7% aqueous solution. Consequently, phenol is frequently prepared with contrast dyes and sterile water, saline, or glycerin. When phenol is exposed to room air, it undergoes oxidation and turns a reddish color; however, it has a shelf life of approximately 1 year if refrigerated and shielded from light exposure. When phenol is prepared with glycerin, it has limited spread; hence, injections are well localized. In rats, the aqueous solution of phenol has greater ability to penetrate the perineurium and produce greater endoneurial damage than glycerin preparations, but there is no difference in results after intraneural injection.13
Putnam and Hampton14 first used phenol as a neurolytic agent in 1936, and Mandl used it for a sympathetic ganglion neurolysis in animals in 1947.15 Originally, it was surmised that phenol had a selective effect on small-diameter, unmyelinated and lightly myelinated nerve fibers, such as C-fiber afferents and A-δ afferents, respectively. Subsequent studies have shown that phenol concentrations determine the type and extent of nerve disruption that also include A-α and A-β fiber damage.16 At concentrations less than 5%, phenol causes protein denaturation of axons and surrounding blood vessels. At concentrations greater than 5%, phenol can produce protein coagulation and nonselective segmental demyelination.17
Unlike alcohol, phenol injection has an initial local anesthetic effect. It is not associated with localized burning but instead creates a sensation of warmth and numbness. Concentrations of 4% to 10% are typically used for neurolysis. Preparations of phenol in glycerin are highly viscous, which may make administration through a small gauge (25-gauge) spinal needle difficult. Careful patient positioning to allow phenol to settle into the desired location is important. When compared with alcohol, phenol seems to facilitate axonal regeneration in a shorter period of time. Electrophysiological studies comparing peripheral nerve destruction in cats showed that those injected with phenol had returned to normal by 2 months; at the end of the same time period, those injected with alcohol still demonstrated depression of compound action potentials.18 However, another study by Smith19 suggests regeneration is not completed until approximately 14 weeks after the administration of phenol.
Celiac Plexus Neurolysis
Indication
Neurolysis of the celiac plexus is one of the most commonly performed neurolytic procedures for the treatment of visceral cancer pain. The nerves of the celiac plexus are responsible for the painful sensation of an extremely large anatomical area, innervating the visceral organs from the distal third of the esophagus to the descending colon. This, therefore, includes the liver, pancreas, gallbladder, stomach, spleen, kidneys, small intestines, large intestines (to the descending colon), and adrenal glands; a partial contribution to the bladder; and a small contribution to the testes and epididymis, the ovaries, and the blood vessels surrounding them.9 Both malignant and nonmalignant pain associated with these organs can be reduced with the neurolytic destruction of the celiac plexus. Although the treatment of nonmalignant pain conditions can be achieved with this technique, it is not recommended for routine use in the treatment of noncancer pain because the procedure is associated with significant and serious complications that may not outweigh the benefits of the procedure. Celiac plexus neurolysis for the treatment of nonmalignant abdominal pain conditions such as chronic pancreatitis has been reported to be more short-lived analgesia than those treated with the same procedure for the treatment of cancer-related pain.9,20,21 Furthermore, the benefits of the neurolysis are likely to be time limited, and the noncancer patient’s life may extend well past the analgesia associated with the procedure. This can leave the patient with their original abdominal pain and partial deafferentation pain, which can be more severe than the initial pain and now with more limited treatment options.
Anatomy
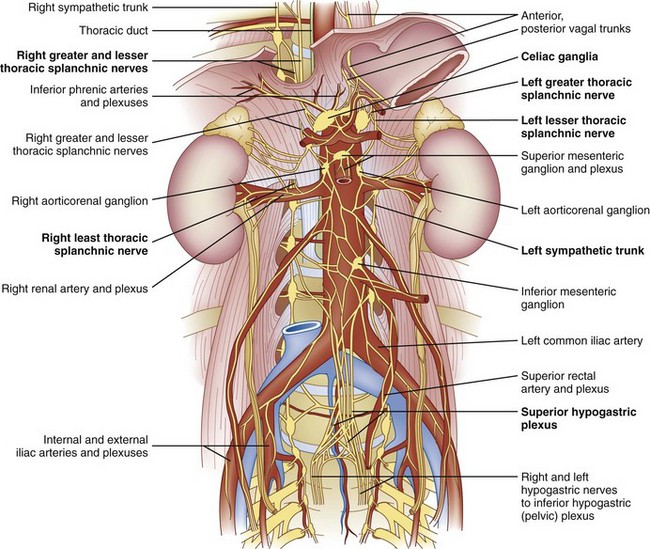
The celiac plexus is located at the level of T12 to L1. It is found in the retroperitoneal space, just anterior and caudad to the crura of the diaphragm (Fig. 9-1). It surrounds the anterior and lateral aspects of the aorta and celiac and superior mesenteric trunks as they divide from the aorta.22 Most commonly, the celiac plexus ganglia are 0.6 cm and 0.9 cm caudad to the celiac artery on the right and left, respectively.23 The location of the celiac plexus varies with respect to bony landmarks and can be located anywhere from the T12 to L1 disc space to the middle of the L2 vertebral body.24 The plexus receives sympathetic fibers from the greater (T9-T10), lesser (T10-T11), and least (T12) splanchnic nerves and parasympathetic fibers from the vagus nerve (Fig. 9-1).
Procedure
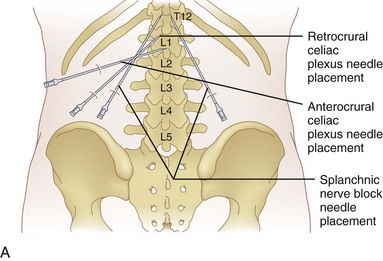
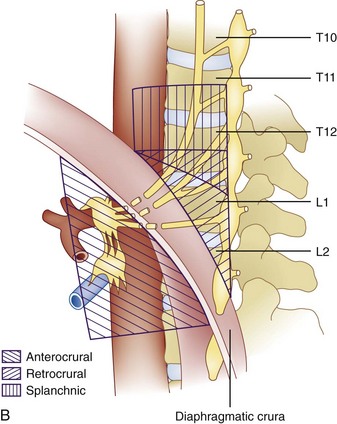
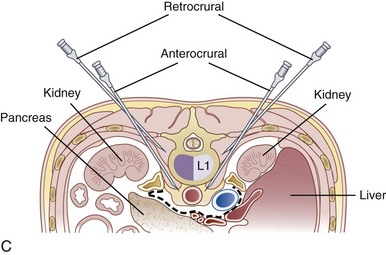
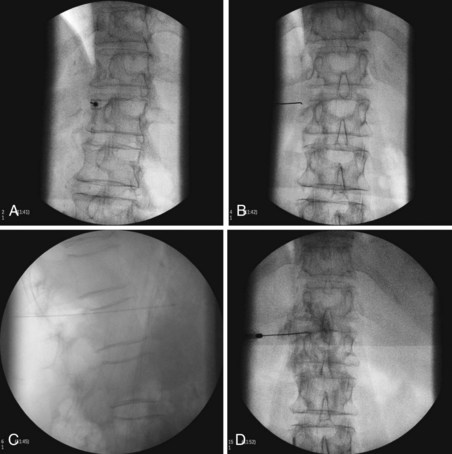
The celiac plexus may be approached in three different ways: retrocrural, anterocrural, and the splanchnic nerves (Fig. 9-2). It can be performed percutaneously in the prone and supine positions using anatomic landmarks, ultrasonography, fluoroscopy, or computed tomography (CT), or through the gastric wall with the assistance of an endoscope.
The most common approach and most thoroughly studied approach is the fluoroscopic or CT-guided posterior percutaneous approach. In this approach, the patient is placed prone, and a 5- to 7-inch small-gauge needle is inserted at the level of the L1 transverse process approximately 5 to 7 cm to the left of midline. This location should coincide with the lateral edge of the L1 vertebral body when viewed in the oblique orientation at approximately 25 to 35 degrees (Fig. 9-3, A) depending on the patient’s body mass index. After the needle is inserted, it is directed toward the upper third of L1 (Fig. 9-3, B) for the retrocrural approach and the lower third of L1 for the anterocrural approach. In performing the retrocrural approach, the needle is advanced just anterior to the anterior border of the body of L1, no more than 0.5 cm. In the anterocrural approach, from the left, the needle is advanced through the aorta (Fig. 9-3, C), and the needle is advanced until no more blood is aspirated. At this time, contrast dye should be injected to confirm location in the anteroposterior (AP) and lateral views (Fig. 9-3, D). If dye spread appears anterior to the aorta and covers the left and right sides and if the provider is intending anterocrural injection, then a second needle from the right side need not be placed. In a retrocrural injection, if the dye spread remains in the anterior third of the vertebral body when examined in the lateral view and on both sides when viewed in AP, then a second needle need not be placed. In performing the splanchnic nerve block, the needles are aimed at the body of T12 using a caudocephalad angle (camera cephalad, image intensifier caudad) of 10 to 15 degrees with skin insertion at the L1 level similar to that of the celiac plexus neurolysis to best avoid puncture of the lung pleural or parenchyma. The needle is then directed until it is just short of the anterior border of the T12 vertebral body. After the needle is placed and secure, a local anesthetic agent with epinephrine is injected to test for inadvertent intravascular access. A long-acting local anesthetic is then injected to produce analgesia before ethanol administration (this can be excluded if phenol is the neurolytic).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree