CHAPTER 243 Nerve Injuries of the Lower Extremity
Epidemiology
It is commonly recognized that traumatic injury of the lower extremity nerves is less common than injury to the upper extremity nerves. In a recent review of lower extremity nerve injuries in Wroclaw, Poland,1 the incidence of lower extremity nerve injuries was 20% of upper extremity nerve injuries. Irrespective of series, the peroneal nerve was the single most common lower extremity nerve to be injured.
All the mechanisms of nerve damage, stretch, contusion, laceration, and compression may be in play in the lower extremity, together or in isolation. Throughout the leg, the relative mix of these mechanisms will vary. For those injuries in the pelvis, surgical options will be significantly limited; elsewhere, the decision making, management, and surgical treatment of lower extremity injuries will be similar to that in the upper extremity, whereas mechanisms and results will vary from location to location. Unfortunately, intraoperative iatrogenic injuries to all nerves of the lower extremity occur. They will be included as traumatic injuries to lower extremity nerves as well. For uniformity and consistency of reporting, all grades of motor recovery calculated originally by the Louisiana State University Health Sciences Center (LSUHSC) system will be transposed into the British Medical Research Grading (BMRC) system2 (Table 243-1) given its nearly universal acceptance. For descriptions of the standard anatomy of individual nerves, the reader is referred to Sunderland’s Nerve and Nerve Injuries.3
TABLE 243-1 British Medical Research Council Scale of Muscle Recovery for Entire Nerve2,85
| M0 | No contraction |
| M1 | Return of perceptible contraction in proximal muscles |
| M2 | Return of perceptible contraction in proximal and distal muscles |
| M3* | All important muscles contract against resistance |
| M4 | All synergistic and independent movements are possible |
| M5 | Full recovery of all muscles |
* A grade of 3 for an individual muscle is only contraction against gravity.
From Medical Research Council. Aids to the Examination of the Peripheral Nervous System [pamphlet]. Memorandum No. 45. London, Her Majesty’s Stationery Office; 1976; and Seddon H. Peripheral Nerve Injuries. Medical Research Council Special Report, Series No. 282. London: Her Majesty’s Stationery Office; 1954.
Lumbosacral Plexus Injuries
Traumatic nerve avulsion injuries of the lumbar and sacral roots are usually seen in severe fractures of the sacrum and pelvis. Only 61 cases of frank root avulsion are documented in the English-speaking literature,4 mostly associated with lumbar and pelvic fractures. The development of a pseudomeningocele (Fig. 243-1) gives evidence of such an avulsion. Furthermore, the nerves and plexus may be injured distal to the exiting nerve roots. Many posttraumatic cases remain undiagnosed because of the high mortality in this patient population. Huittinen5 performed autopsies on 42 fatalities with pelvic fractures and established that 20 patients (48%) had evidence of injury to the lumbosacral plexus.6
In the past, these injuries (Fig. 243-2) were considered inoperable, and no specific treatment directed at nerve repair was offered. More recently, this position has been challenged with the strategies of nerve transfer and nerve grafting.7 Although these approaches remain experimental, they represent an advance beyond the previous nihilist approach to high lumbosacral injuries.
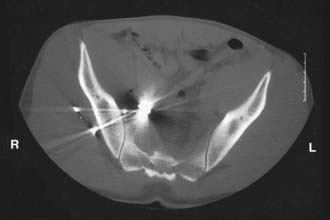
FIGURE 243-2 Gunshot injury to right lower extremity associated with a lumbosacral plexus injury. No operative repair was offered.
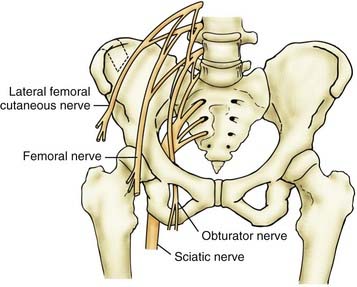
Obturator Nerve
The obturator nerve (Fig. 243-3) is the only nerve of the pelvis to pass through the pelvis without innervating any pelvic structures. This nerve is infrequently affected by external trauma, and the deficits, both sensory and motor, are usually mild. Injury to this nerve has been associated with total hip arthroplasties, acetabular fractures (Figs. 243-4 and 243-5),8 anterior extrusion of cement for total hip arthroplasty, and malpositioned acetabular screws. Loss of adductor function is usually well tolerated, and diminution of sensation in the medial thigh obturator distribution rarely causes significant deficit. Nevertheless, such a deficit has been reported in a few cases as causing significant disability.9
Femoral Nerve
The femoral nerve (see Fig. 243-3) is largely protected by its retroperitoneal position from most daily external trauma but is subject to a number of injuries (Table 243-2). Penetrating injuries to the groin can damage the nerve and may be associated with life-threatening injuries to both the femoral artery and vein.10 Pelvic fractures can sometimes be associated with femoral nerve injuries,11 including acetabular fractures.12 Similarly, missile injuries to the retroperitoneum and proximal thigh can result in injury to the femoral nerve.11,13,14–16 In a civilian practice, however, most injuries to the femoral nerve are iatrogenic16,17 and have been associated with abdominal hysterectomy for more than a century18–21 as well as with oophorectomy,22 renal transplantation,23 abdominal and pelvic laparoscopic procedures,24 laparoscopic hernia repair,25,26 and aortic surgery.27 Although sciatic injuries are more common with total hip arthroplasty (THA) and represent 80% of THA-associated nerve injuries, femoral nerve injury can also result from this procedure. The anterior extrusion of cement with exothermic femoral nerve coagulation has been shown to be a mechanism for injury.28,29 In addition, secondary iliacus hematomas have also been reported as causative factors in operative and postoperative femoral palsies associated with THA.30 The nerve may also be injured by nearby femoral artery31,32 or vein33,34 catheterization. Iliacus hematoma can occur in relationship to minor trauma (Fig. 243-6) and normal coagulation status35,36 as well as secondary to anticoagulation therapy37 or hemophilia.38 Although unusual, femoral injury has also been reported as a complication of injection injury or toxic reaction to local anesthetic.39
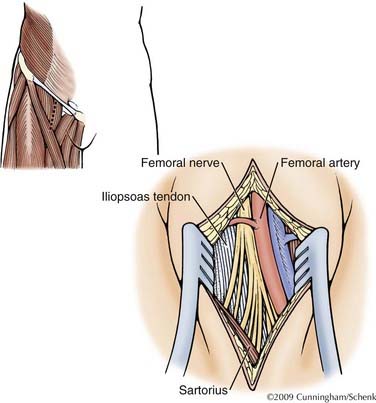
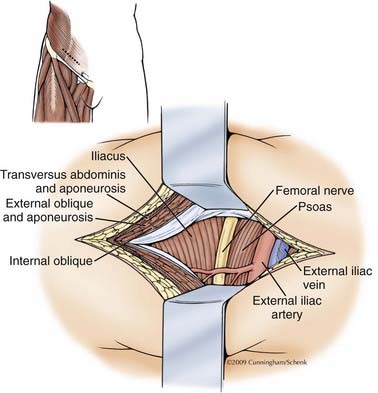
Surgery
Surgery is divided into two approaches depending on level involved: thigh-level exposure and retroperitoneal exposure (Figs. 243-7 and 243-8). The inguinal ligament separates the exposable area. By a combination of approaches, the inguinal ligament is left intact, with dissection of the intervening segment achieved from both above and below. If necessary, the inguinal ligament can be divided and subsequently repaired.
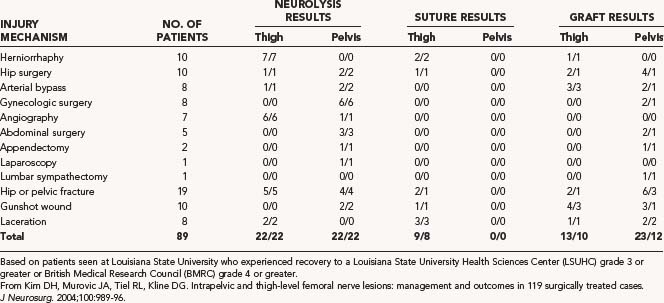
Results
Kim and colleagues16 reported on the management of 89 traumatic injuries of the femoral nerve gathered over a 32-year period (see Table 243-2). Fifty-two patients, or 58.4% of injuries, were iatrogenic. All patients demonstrating an adequate nerve action potential (NAP) and treated by neurolysis had a successful recovery based on recovery to a LSUHSC grade 3 or better or a BMRC grade of about 4, as did those suffering injury from a lacerating mechanism. Of those injuries repaired with simple neurorrhaphy at the thigh level, 89% were judged to be successful. Of the femoral lesions that required grafting, 52% made a successful recovery. In the civilian missile category, 75% of patients had a successful recovery of thigh-level injuries, whereas only 33% of patients with pelvic-level injuries has a successful recovery. Secer,15 in his review of 40 years of treatment of missile injuries, collected 19 femoral nerve injuries separated into high, intermediate, and low categories, treated between 4 and 6 months postinjury. One patient was treated with intrafascicular nerve grafting, 9 with end-to-end suture, and 9 with neurolysis. BMRC M3 or greater motor function was reported in 78% of all femoral injuries collectively, whereas BMRC sensory recovery to S3 or greater occurred 89% of the time. Similarly, Roganovic and Pavlicevic13 reported on 15 patients suffering missile injury during the Bosnian conflict to the femoral nerve at an intermediate level, 14 of whom required graft repair and 12 of whom had grafts less than 4 cm in length. They demonstrated recovery to BMRC M3 or greater in 73% of patients.
Lateral Femoral Cutaneous Nerve
The union of the posterior branches of the L2 and L3 roots forms the lateral femoral cutaneous nerve (LFCN) (see Fig. 243-3). Tightening of the abdominal fascia and “scissoring” of the LFCN may be a mechanism responsible for compression after abdominal or gynecologic operations as well as direct injury from retractor blades on the lateral abdominal wall. Postpartum delivery injuries in the mother have also caused injury to the LFCN or exacerbated the symptoms of prior compression. LFCN injury was the most common nerve injury associated with parturition in nulliparous patients with prolonged second-stage labor.40
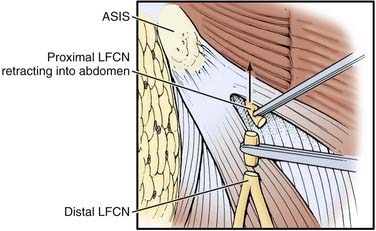
Harvesting of iliac crest in proximity to anterior superior iliac spine (ASIS) (Fig. 243-9) has been known to damage this nerve. Damage was more common with a bone graft depth of more than 30 mm. The incidence of nerve injury was 20% with graft length of more than 45 mm, 16% when graft length was between 30 and 45 mm, and 8% when graft length was less than 30 mm. It is recommended that the iliac crest graft should be no closer than 15 to 20 mm posterior from the ASIS.41 Direct external pressure on the LFCN medial to the ASIS is thought to be responsible in posterior spine operations, especially in the Relton-Hall frame.42 The symptoms after direct nerve injury may be quite persistent and unremitting in contradistinction to those complaints caused by simple compression. The natural history of meralgia paresthetica is usually one of resolution43 but rarely in large series. Postsurgical injury patients may, however, need operation. Symptomatic treatment with tricylic antidepressants or gabapentin may provide adequate relief for some. In addition, local administration of topical steroids with or without anesthetic may prove efficacious.43 After surgery has been selected, there are two operative strategies that may be offered.44 The operations for decompression are described elsewhere (see Chapter 241). For more proximal LFCN injuries, there are no simple surgical treatments to be recommended, and most education is focused on prevention. Occasionally, spinal cord stimulation has been offered45 in the absence of any direct definitive treatment. In some cases, section of the LFCN may be helpful (Fig. 243-10), but this remains a controversial treatment.
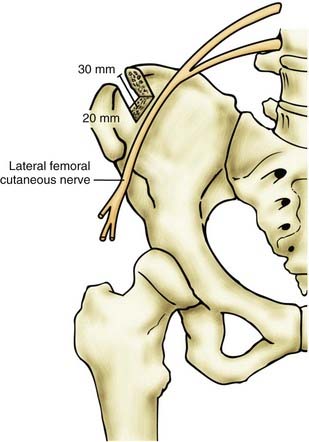
FIGURE 243-9 Diagram illustrating danger zones for lateral femoral cutaneous nerve injury with iliac crest harvesting. Damage was more common41 with a graft depth of greater than 30 mm and proximity to the anterior superior iliac spine of less than 1.5 to 2 cm.
(© M. Schenk and W. K. Cunningham, Biomedical Illustration Services, University of Mississippi Medical Center, Jackson, Mississippi.)
Sciatic Nerve
The sciatic nerve is the largest nerve of the body and arises from the L4-S3 nerve roots (Fig. 243-11). At the level of the buttock, iatrogenic injuries are more common than noniatrogenic injuries,46 with injection leading this list, followed by injuries sustained during THA.
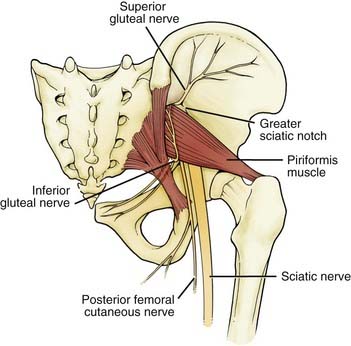
FIGURE 243-11 The emergence of the sciatic nerve under the piriformis and its descent inferiorly.
(© M. Schenk and W. K. Cunningham, Biomedical Illustration Services, University of Mississippi Medical Center, Jackson, Mississippi.)
Sciatic nerve injury has been reported in all categories of the Thompson and Epstein classification of hip fractures. The precise mechanisms of injury varies; direct femoral head compression, compression by acetabular fragments, laceration by acetabular fragments, and trapped acetabular fragments have all been described.47–49 Conversely, others have described grossly normal-appearing nerves with clinical paresis, suggesting a pure stretch mechanism.50
The surgical repair of the hip joint, THA, has also been associated with significant sciatic injury. The frequency varies among studies, ranging from 0.65% to 3.7%, but most large series average 1.7%. These rates are elevated in revision surgeries (3% to 8%) and in patients with developmental dysplasia of the hip to about 5%. With simple THA, the incidence is about 1%. Because only a severe injury presents as a clinical problem, injury may be more frequent than is generally appreciated.51 The specific etiologies are variable. Direct injury from scalpel, electrocautery, retractors, wires, reamers, Gigli saw, bone fragments, or cement protrusion; constriction by suture, wire, or cable; heat from polymerization of cement; compression from dislocation; excessive lengthening (>4 cm); and subfascial hematoma have all been reported as mechanisms of nerve injury. Still, in more than 50% of THA-associated palsies, the exact mechanism remains unknown.52
Injection injuries remain a significant source of traumatic injuries to the sciatic nerve at the buttock level.46 Most can be attributable to misplaced gluteal injections. The sciatic nerve is injured more than any other peripheral nerve in this manner. The principle cause for these injuries, as with all nerve injection injuries, is “carelessness combined with an appalling ignorance of elementary anatomy.”3 Most of these injuries result from needle insertion in the inferior medial section of the buttock instead of the superior lateral quadrant. Unfortunately, animal experiments suggest that there is little to gain by immediate surgical maneuvers such as washing the nerve or internal neurolysis.53
Surgery
Exposure of the sciatic nerve is divided into two approaches: upper sciatic exposure for hip and buttock-level pathology (Fig. 243-12), and a lower exposure for thigh-level injuries (Fig. 243-12, inset, and Fig. 243-13). The sciatic nerve may be surgically separated both at the buttock level (Fig. 243-14) and at the thigh level, even in thick scar (Figs. 243-15 to 243-17). When even more exposure is required, the superior exposure may be connected to the inferior portion of the buttock exposure for a complete exposure of the sciatic nerve.
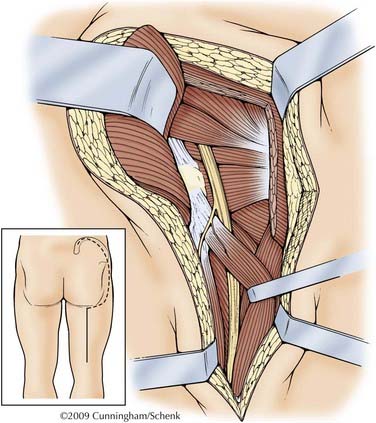
FIGURE 243-12 The proximal approach follows the general instruction of Henry.78 A “question mark” incision is used starting at the posterior superior iliac spine and running a handbreadth along the iliac spine and then turning toward the greater trochanter. This will expose the superior edge of the gluteus maximus. The lateral attachment of the gluteus maximus is then cut and elevated and further divided inferiorly. The inferior edge of the gluteus maximus is mobilized along the line of the gluteal cleft medially until the body of the gluteus maximus can be retracted medially. The sciatic nerve is then deep and medial to the gluteus maximus, often in fatty tissue coming out from under piriformis muscle.
(© M. Schenk and W. K. Cunningham, Biomedical Illustration Services, University of Mississippi Medical Center, Jackson, Mississippi.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree