New Applications of Postmortem Neuroradiology in the Forensic Investigation of Death
Barry Daly
Robert Morales
Modern neuroimaging, especially computed tomography (CT) and magnetic resonance imaging (MRI), has revolutionized practice and research in the clinical neurosciences in the last 30 years. Although radiographs have been used extensively in forensic diagnosis since shortly after their discovery by Wilhelm Roentgen at the end of the 19th century, the use of CT and MRI in the evaluation of medical examiners’ cases has been limited.1 Today, these diagnostic methodologies are poised to have a significant impact on forensic pathology and neuropathology as a complement to or, in selected cases, as a possible replacement for postmortem examinations. Early research on the use of CT and MRI in autopsy imaging has been performed in Europe, Japan, and the United States and has shown great promise.2, 3, 4, 5, 6, 7, 8, 9, 10 Recognizing that the application of postmortem imaging to neuropathology is in its infancy, we believe it is important for readers to be familiar with the available techniques, their current use, and their potential.
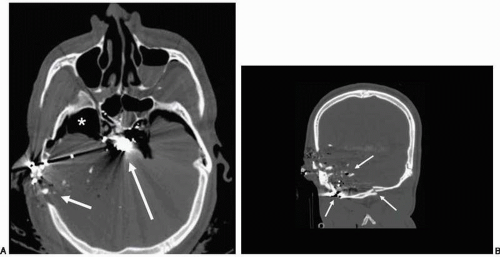
Postmortem neuroimaging has two major potential roles. First, neuroimaging can be used to aid in focusing autopsies. For example, in gunshot wounds of the head, CT can help to identify and accurately localize projectiles and their trajectories, fragments of projectiles, and bone fragments (Fig. 23.1).
Over many decades, conventional radiography and fluoroscopy have provided assistance to the forensic medical examiner for ballistic localization. The recent application of the three-dimensional (3D) capabilities of CT and MRI in this forensic setting has shown that these newer imaging tools are of greater value.3, 9 In major traumatic injuries in which multiple skull vault and/or base fractures are present, CT and MRI can be quite helpful in identifying fractures8 and providing a permanent record of the 3D appearances (Fig. 23.2).
It is widely recognized that autopsy dissection of the skull vault and base at autopsy may be difficult in the presence of multiple fractures: disintegration of the skull and its contents may easily occur after removal of the scalp. In such cases CT and MRI may provide information that is difficult to obtain with conventional autopsy. Both CTand MRI can accurately localize the presence and location of major spinal injuries, including fractures and dislocations, thus helping to guide the dissection at autopsy (Fig. 23.3).
Second, postmortem neuroimaging also has potential for screening intracranial lesions and providing sufficient information to determine whether conventional neuropathologic autopsy is necessary. If CTor MRI can exclude any substantive intracranial or spinal injury, especially in cases in which the clinical suspicion for such injury is low, dissection may be avoided, with resulting savings of time and expense. Conversely, if severe intracranial or spinal injuries are clearly depicted on CT or MRI, dissection to demonstrate what is evident on the imaging study might be considered redundant (Fig. 23.4).
The value of CT and MRI for in vivo diagnosis of cranial and spinal injury is well recognized.11, 12, 13, 14, 15, 16, 17, 18 The discussion of CTand MRI for “imaging autopsy” in this chapter addresses early experience in the application of many of the same techniques to the postmortem setting.
Few medical examiners’ offices or forensic pathology departments in academic institutions have CT or MRI scanners on site and so must rely on the availability of machines at clinical facilities. Such scanners are often unavailable for forensic work during daylight hours, and the logistic problems of transporting bodies of decedents into a hospital for imaging can be considerable. At the time of writing, no medical examiners’ office in the United States has introduced CT and MRI into forensic neuropathology, except on investigational and ad hoc bases. Centers in Europe, Australia, and Japan have introduced this technology, and initial accounts of their experiences have been positive.2, 3, 4, 5, 6, 7, 8
One important consideration that is likely to influence the adaptation of CT and MRI in forensic neuropathology is economic: major costs are associated with the purchase, use, and maintenance of the equipment, in addition to the cost of interpretation of the imaging studies by radiologists. To justify such expenses, imaging studies must provide added value or savings that may be offset against the cost of introducing this technology. If a role evolves in forensic medicine for CT and MRI studies and this technology becomes widely accepted in clinical practice, such developments may obviate the need for autopsy in some situations. Savings in time and expense for the medical examiner and staffmay be possible, and the shortage of forensic medical examiners in some jurisdictions may be eased. Radiologists are likely to become part of the medical examiner’s staff and may help to disseminate the use of this new science.
It is notable that CTscanner costs are lower than those for MRI units. The price for a CT scanner is in the $1 million range for a new 64-slice machine, (although refurbished 16-slice units may be considerably cheaper and still capable of performing the thin-section imaging necessary for diagnosis. Maintenance contracts and upkeep may run to $100, 000 annually. Space for a CT scanner suite and for 3D workstations also must be considered. Because CT scanners are more likely to be installed at medical examiners’ offices in major metropolitan centers, radiology services may be contracted with academic departments that are likely to have the necessary subspecialty expertise to interpret imaging studies. Transmission of digital imaging data via the Internet allows studies to be rapidly interpreted at sites far remote from the scanner, and
such teleradiology services are already widely used for off-hours readings and for consultations. Imaging the body with a modern multislice CT scanner takes less than 10 minutes, thereby allowing a relatively large number of studies to be completed in a short period of time (in practice, approximately 4 to 5 per hour).
such teleradiology services are already widely used for off-hours readings and for consultations. Imaging the body with a modern multislice CT scanner takes less than 10 minutes, thereby allowing a relatively large number of studies to be completed in a short period of time (in practice, approximately 4 to 5 per hour).
In contrast, MRI scanners are more expensive, typically in the $1 million to $1.5 million range. MRI is more time consuming: acquisition time for each body part may exceed 15 minutes, and an entire body requires at least 2 hours. MRI is used clinically to assess focal problems rather than to produce whole-body scans. MRI has greater sensitivity than CT for pathologic changes in most parts of the body, 12, 13, 16, 19 and it may have a role in cases in which abnormal findings are present but nonspecific on CT. MRI is more sensitive for subtle changes in the brain and spine, although CT may show major findings and cause of death in many cases, especially in the setting of major blunt trauma or spontaneous intracranial hemorrhage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree