Chapter 11 Normal Variants in the Electroencephalogram
Many of the normal variant patterns described here bear some resemblance to epileptiform activity. The importance of developing proficiency in recognizing these patterns is to avoid mistaking them for epileptiform abnormalities. The basic features of these normal variants should be committed to memory so as to avoid the pitfall of describing one of these variants as an epileptiform abnormality (Table 11-1).
Table 11-1 Summary Table of Selected Normal Variants
| Posterior Occipital Sharp Transients of Sleep | Positive-polarity, low-voltage occipital sharps occurring in sleep, a normal sleep element |
| Lambda Waves | Low-voltage occipital sharps during wakefulness associated with searching eye movements |
| Small Sharp Spikes/Benign Epileptiform Transients of Sleep | Low-voltage temporal spikes, synchronous or independent, unilateral or bilateral, with broad field seen in adults during drowsiness and light sleep |
| Mu Rhythms | Arch-shaped rhythm in central areas during wakefulness, suppresses with contralateral hand movement |
| 14- and 6-Hz Positive Bursts | Medium- to high-voltage, positive-polarity, arch-shaped bursts during drowsiness and light sleep in posterior temporal and occipital areas, mostly in children |
| Wicket Spikes/Wicket Rhythms | Arch-shaped rhythm of temporal areas during drowsiness and light sleep, mostly in adults |
| Breach Rhythms | Rhythm of increased fast activity, often with spiky appearance, seen over craniotomy sites |
| Rhythmic Temporal Theta Bursts of Drowsiness/Psychomotor Variant | Sharpened theta rhythm in temporal areas during drowsiness and light sleep |
| 6-Hz Spike and Wave/Phantom Spike and Wave | Brief 6-Hz rhythms with inconsistent spike component seen in wakefulness and drowsiness, mostly in adults, following WHAM and FOLD patterns |
| Posterior Slow Waves of Youth | Theta and delta waves intermixed with posterior rhythm until mid-teenage years |
FOLD, Female whose pattern has an Occipital emphasis, Low in amplitude, and seen in the Drowsy record; WHAM, Waking record, High in amplitude, Anterior in location and especially in Males.
NORMAL VARIANTS THAT MIMIC SINGLE EPILEPTIFORM WAVES
Posterior Occipital Sharp Transients of Sleep
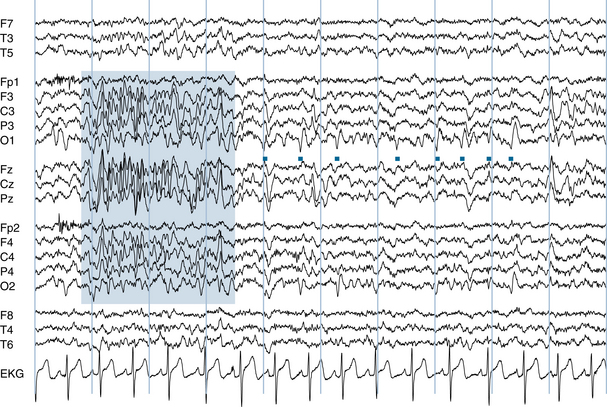
Posterior occipital sharp transients of sleep (POSTS) are one of the most common normal variants seen in the EEG and can be considered one of the normal elements of sleep. The acronym POSTS tells the story of these distinctive waveforms: POSTS are of Positive polarity, they are seen in the Occipital areas; they have a Sharp Transient waveform, and they occur in Sleep. POSTS are “triangular” or V-shaped wave that are particularly prominent in light sleep (see Figures 11-1 and 11-2). If not recognized as POSTS, these low-voltage discharges could potentially be mistaken for occipital sharp waves. Because POSTS are so common, the polarity of any low- to medium-voltage occipital sharp wave seen in sleep should be assessed before deciding that it is abnormal. Displaying POSTS in an appropriate referential montage should confirm their positive polarity and correctly identify them as POSTS rather than epileptiform discharges. POSTS usually appear in a bilaterally synchronous fashion, although normal POSTS may manifest asymmetrical amplitudes. POSTS may occur in brief, semirhythmic runs. Although POSTS usually consist of low-voltage, V-shaped waves, they may occasionally assume a more spiky appearance (see Figure 11-3).
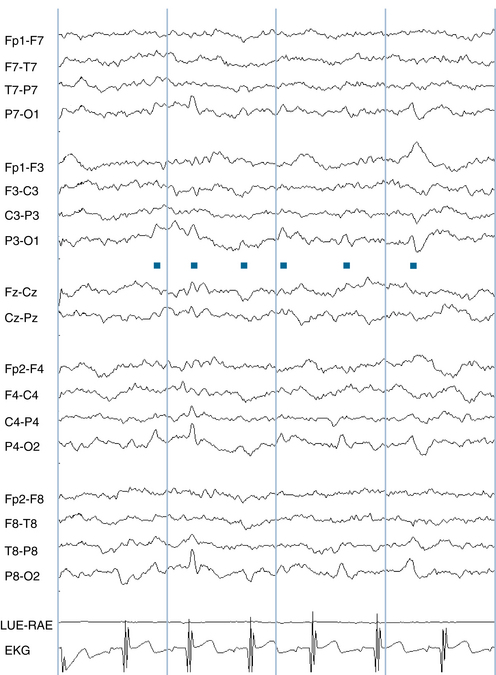
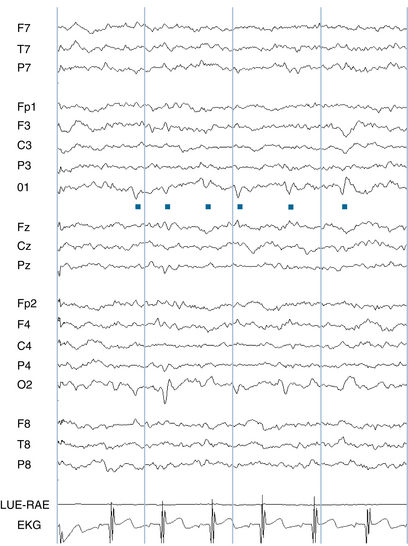
Figure 11-1 The distinctive triangular waves seen in the four occipital channels (P7-O1, P3-O1, P4-O2, and P8-O2) are examples of posterior occipital sharp transients of sleep (POSTS; indicated by dots). The upgoing deflection of these waves in the occipital channels of this bipolar montage suggests two possible polarity/localization combinations. The first is that the upgoing wave implies that the parietal electrodes, P3 and P4, are “more negative” than O1 and O2 and that these waves could be caused by a negativity in the parietal areas. No clear phase reversal is seen anterior to the upgoing waves, however, raising the suspicion that a parietal negativity does not explain the waveform. The second possibility is the correct explanation: O1 and O2 should be considered “more positive” than P3 and P4, and a positivity in the occipital area is causing the deflection. The absolute polarity of the event—in this case, an occipital positivity—is most easily confirmed by displaying it in a referential montage (see Figure 11-2).
Lambda Waves
Lambda waves are discussed with POSTS because their morphology and location are similar. The two are easily distinguished because lambda waves occur exclusively during wakefulness and POSTS are seen during sleep. Lambda waves also appear as low-voltage triangular waves in the occipital areas, reminiscent of the Greek letter λ, but they are distinctive in that they occur at the time of lateral searching eye movements. Confirmation that a low-voltage occipital sharp transient wave is a lambda wave is made easier by finding evidence of concurrent lateral eye movement artifact. Lambda waves may be either surface positive or surface negative in the occipital area (see Figure 11-4). They are not as common as POSTS and are seen more frequently in children than in adults. Because they are related to searching eye movements, lambda waves are generally seen when the patient’s eyes are open and the posterior rhythm is suppressed. Voltage asymmetry of lambda waves is not necessarily considered abnormal.
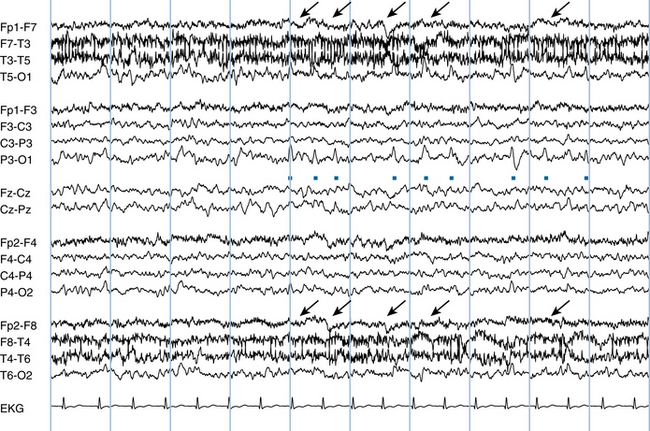
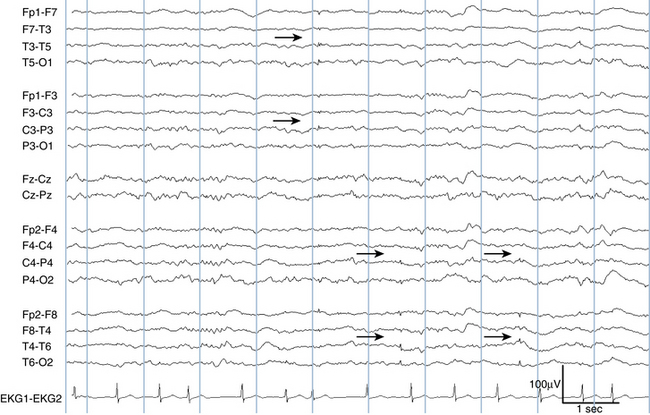
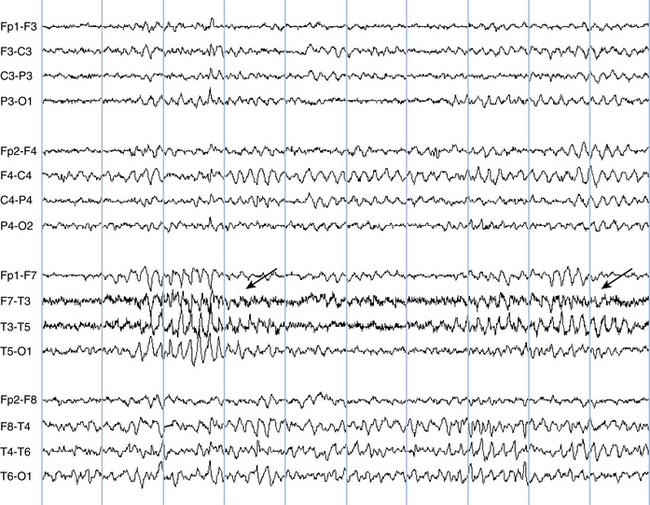
Figure 11-4 The triangular-shaped waves seen in the occipital channels are examples of lambda waves (dots). Lambda waves are associated with horizontal searching eye movements. Subtle lateral eye movement artifact (arrows) is seen in the frontal/anterior temporal channels with opposite polarity on each side (see Chapter 6, “Artifacts”) for further description of eye movement artifact).
Small Sharp Spikes and Benign Epileptiform Transients of Sleep
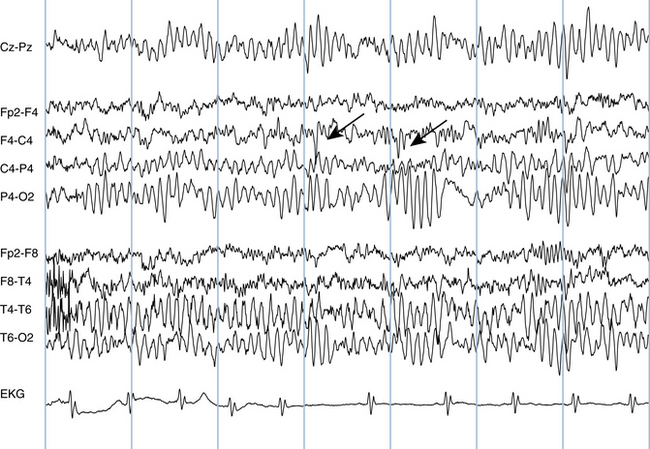
The terms small sharp spikes (SSS) and benign epileptiform transients of sleep (BETS) are synonymous. These quick, low-voltage spikes are usually seen in the temporal areas with a broad gradient across the temporal chain. The upward and downward phases of the transients are usually of similar amplitude. They occur either unilaterally or bilaterally and, when bilateral, they may occur either synchronously or independently (see Figure 11-5). SSS are seen in drowsiness and light sleep and tend to disappear with deepening sleep. SSS are considered by many to represent a normal variant but some authors still contend that the finding suggests an increased degree of epileptogenicity.
NORMAL VARIANTS THAT MIMIC REPETITIVE EPILEPTIFORM WAVES
Mu Rhythms
Mu rhythms are commonly encountered rhythms seen in the central areas during wakefulness, best recorded by the C3 and C4 electrodes. They are most often seen from later childhood into the adult years, although they are occasionally seen in very young subjects. The mu rhythm has a distinctive arciform (arch-like) or “comb-like” morphology (see Figure 11-6). Because the mu rhythm is suppressed by voluntary motor activity in the opposite hand, the technologist can establish that a sharp central rhythm is a mu rhythm by requesting that the patient move the contralateral hand and demonstrating that the rhythm disappears. Although classically suppressed by moving the contralateral hand, movement of the ipsilateral hand or planning to move the hand may also suppress the mu rhythm in some subjects.
Because this arciform rhythm is sharpened on one side and rounded on the other, there is some potential to mistake it for epileptiform activity. When mu rhythms occur in trains, it is not difficult to identify them correctly on the basis of their location, morphology, and suppression with movement, if necessary. Occasionally, fragments of a mu rhythm may resemble low-voltage spike activity (see Figure 11-7). Apparent low-voltage central spikes can be confirmed to be a mu phenomenon by showing that the morphology of the spike fragment is similar to the mu waves when they occur in trains.
The mu rhythm and the posterior rhythm are the two main idling rhythms of the EEG: the mu rhythm is only seen during contralateral motor inactivity and suppresses with movement. Similarly, the posterior rhythm is only present during visual inactivity and suppresses with eye opening or visual attention. A mu-shaped rhythm that does not necessarily suppress with movement is occasionally seen in the central midline (Cz) and is referred to as a midline theta rhythm.
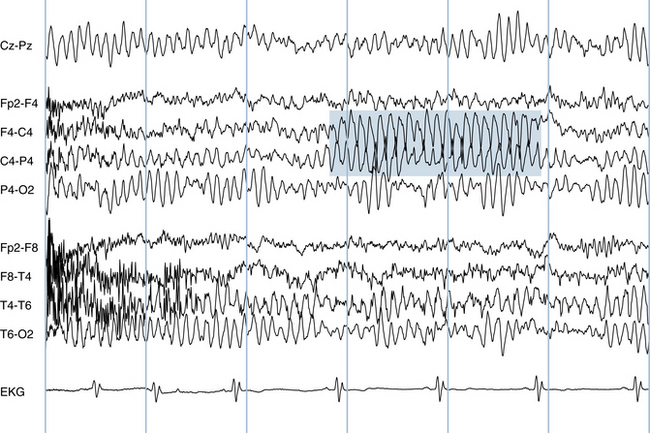
Wicket Spikes and Wicket Rhythms
Because their morphology is quite similar to that of mu rhythms, wicket rhythms are discussed with mu rhythms. Wicket rhythms differ from mu rhythms in that they are seen in drowsiness and light sleep rather than wakefulness and have a predilection for the temporal rather than the central areas (see Figure 11-8). Their arciform morphology is similar. Wicket rhythms range from 6 to 11 Hz with a voltage range of 60 to 200 μV (Reiher and Lebel, 1977). Similar to the situation seen with mu rhythms, it is possible to mistake a fragment of a wicket rhythm for epileptiform activity rather than a normal variant. Such fragments are called wicket spikes. Wicket spikes are distinct from temporal spike-wave discharges in that there is no aftercoming slow wave and they do not disrupt the underlying rhythm. The confirmation that a temporal spike is a wicket spike is best made by noting that the waveform is similar to that of the spikes when they occur in a train (as a continuous wicket rhythm) found elsewhere in the same tracing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree