CHAPTER 321 Osteoporotic Fractures
Evaluation and Treatment with Vertebroplasty and Kyphoplasty
The impact of osteoporosis is increasingly being recognized as the population ages.1 One of the primary adverse manifestations of osteoporosis is vertebral compression fractures. Indeed, an estimated 700,000 osteoporotic vertebral compressions fractures occur annually in the United States.2,3 Vertebral compression fractures are a significant problem associated with pain and functional impairment.4–7 The antiquated perception that these fractures are benign and self-limited is being replaced as our understanding evolves and our current treatment options have expanded.
History
The first vertebroplasty was performed in France in 1984 by Galibert and colleagues, with its subsequent appearance in the literature 3 years later.8 At that time, PMMA was used to successfully treat a painful hemangioma of the C2 vertebra. One year after the technique was first described, it was reported for the treatment of osteoporotic vertebral compression fractures.9 Almost a decade later, in 1993, the first vertebroplasty was performed in North America at the University of Virginia and was subsequently reported in 1997.10 Kyphoplasty, a modification of the established procedure vertebroplasty, was first reported in 1998, and shortly thereafter data began to accumulate supporting its use.11–13
Indications and Contraindications
Vertebroplasty and kyphoplasty are indicated in patients with osteoporotic vertebral body fractures associated with significant pain. These osteoporotic vertebral body fractures include compression fractures, as well as selected burst fractures,14 specifically those with no or limited canal compromise and an intact posterior cortex and posterior longitudinal ligament.
The timing of treatment with vertebroplasty and kyphoplasty is evolving. It has generally been suggested that vertebroplasty and kyphoplasty were indicated only after a failed 4- to 6-week trial of conventional medical therapy consisting of bed rest and analgesics, a protocol that has been used in numerous clinical studies.10,15 Although some have anecdotally reported improvement in pain after treatment years after the initial injury,16 late treatment (>6 months after injury) is less likely to be successful.17 Others have advocated earlier treatment for those unable to ambulate secondary to pain or for individuals requiring parenteral narcotics and hospital admission.18
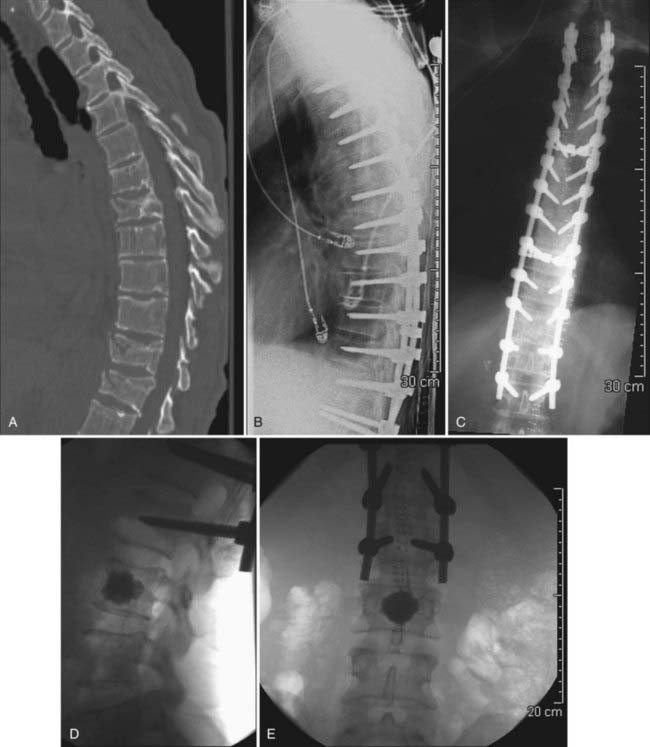
Although there may be a role for prophylactic vertebroplasty and kyphoplasty in patients who are at high risk for compression fractures, prophylactic treatment is not widely accepted or approved as an indication, even though there has been recent interest in investigating this issue.19–21 One exception may be patients who have undergone long-segment posterior spinal instrumentation procedures and are at high risk for failure at the cranial or caudal limits of the fusion (Figs. 321-1 and 321-2).
Patient Evaluation
To determine a patient’s suitability for vertebral body augmentation, one must obtain appropriate images before performing the procedure. The initial evaluation often consists of a plain radiograph followed by computed tomography (CT), magnetic resonance imaging (MRI), or a bone scan. For patients who have a documented new compression fracture seen on plain films, it may be unnecessary to acquire additional studies if they are clinically appropriate for vertebroplasty.22 Additionally, plain films document overall sagittal and coronal balance and provide some indication of bone quality and the degree of vertebral body collapse.
If it is not clear whether the fracture in question is acute or whether multiple compression fractures are present, MRI is often helpful to determine which level or levels may best be treated by vertebroplasty or kyphoplasty. It has been suggested that the finding of edema on MRI may predict a favorable outcome with vertebroplasty, although the absence of signal change on MRI does not necessarily obviate one from having such a response with treatment.22,23 For obvious reasons, MRI should be considered mandatory if the diagnosis of a vertebral body metastatic lesion is being entertained.
Bone scintigraphy has been proposed as an adjunctive technique for facilitating both the selection of patients and which levels to treat when multiple fractures are present in a given patient. Bone scintigraphy is particularly useful when multiple fractures of different age are present. Levels at which increased uptake of tracer are identified generally respond well to vertebroplasty or kyphoplasty in terms of pain relief.24–26
Technique
Vertebroplasty
Vertebroplasty is typically an outpatient procedure that can be performed in a location with appropriate imaging equipment, including the operating room and interventional radiology suite. We perform vertebroplasty in a neurointerventional suite with high-quality biplanar fluoroscopy. Alternatively, CT guidance has been used effectively for the performance of vertebroplasty.27–31 Vertebroplasty can usually be performed with a moderate amount of conscious sedation and local anesthesia. Even though conscious sedation may be adequate, certain individuals, such as patients unable to lie still because of pain, may require general anesthesia. Once sedated, the patient is placed in the prone position with the arms raised above the head to minimize interference with fluoroscopy. This position increases extension of the targeted vertebral bodies, and treatment in this position is thought to reduce the kyphotic deformity associated with the fracture.32
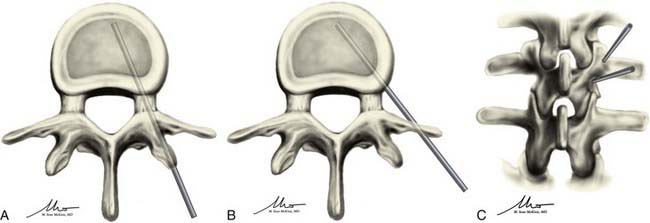
Once adequately positioned, the affected vertebrae and their respective landmarks are identified with biplanar fluoroscopy. After confirming that the target vertebrae are suitable for injection of cement, the needle trajectory is planned. Needle placement can be accomplished from either a transpedicular or parapedicular approach (Fig. 321-3). Factors that guide selection include pedicle size, vertebral body size, and whether a unipedicular or bipedicular approach is being contemplated. For the lumbar and thoracic spine, where pedicle size is larger, a transpedicular approach may be preferred. In the thoracic spine, where pedicle size is smaller, a parapedicular approach may be preferable. As mentioned, a unipedicular or bipedicular approach may be chosen. Early reports of vertebroplasty described a bipedicular approach in which cement was injected through each needle located in their respective hemivertebrae.10,22,33,34 The bipedicular approach was undertaken to maximize the volume of filling within the vertebral body. However, a unipedicular approach was proposed and implemented as a means of decreasing procedure time, radiation exposure, discomfort for the patient, and difficulties associated with monitoring the second injection, particularly on the lateral plane, when there was already preexisting cement from the first injection.35 This approach entailed the insertion of a single needle into the midline of the vertebral body near the anterior cortex of the vertebral body. With such needle placement, filling of the central vertebral body from pedicle to pedicle can be achieved. There does not appear to be any difference in clinical outcome between a unipedicular and a bipedicular approach for vertebroplasty.35 We have generally adopted a unipedicular approach.
When using a unipedicular approach, we prefer to insert the needle on the patient’s right side (the operators stand on the patient’s left side). This places the physician further away from the radiation source and is less cumbersome than an ipsilateral approach through the left pedicle. A straight anteroposterior (AP) image is obtained, and the AP tube is then moved obliquely approximately 20 degrees laterally until the Scotty dog profile is seen over the pedicle. For the thoracic spine, an oblique orientation of the tube may make visualization of the pedicle more difficult because the pedicles are less angulated in the AP plane. However, if the pedicle is carefully tracked from the straight AP to the oblique position, it can be visualized; alternatively, the AP tube can be oriented obliquely laterally until the pedicle projects over the medial fifth of the vertebral body.22 The needle for local anesthetic is then inserted until it rests on the periosteum at the proposed site where the vertebroplasty trocar will be inserted into the pedicle. Local anesthetic is then infused into the periosteum and infiltrated into the tissues as the needle is withdrawn to the skin surface. A wheal at the skin surface is raised just before the needle is withdrawn.
In the unilateral transpedicular approach, the needle is advanced until it docks on the intended pedicle. This should occur at the superior lateral quadrant of the pedicle to minimize the risk of damaging the exiting nerve root, a risk that increases with more inferior and medial positioning. This also creates a trajectory that is directed toward the center of the vertebral body. Once at the appropriate location on the pedicle, the needle is advanced in 1- to 2-mm increments through the pedicle into the vertebral body under biplanar fluoroscopic guidance. The needle tip should ideally end in the anterior half of the vertebral body and should be midline when seen on an AP view (see Fig. 321-3A and C). The target may be manipulated slightly according to the location of the fracture; however, the majority of treatments can be accomplished by placing the needle tip in this final location. If using the bipedicular approach, the contralateral side may be cannulated in similar fashion. If multiple levels are being treated, they are typically all cannulated before the injection. If the levels to be treated are contiguous and the distance between levels is relatively small, the side of needle placement can be alternated.
The parapedicular approach takes a more lateral trajectory to the vertebral body and begins by advancing the needle until it is docked on the transverse process. Once at the transverse process, the needle is walked caudal to the transverse process and passed anteromedially to the entry point. The ideal entry point into the vertebral body is at the junction between the pedicle and the vertebral body and is visualized on the lateral projection as being just anterior to the posterior end plate and on the lateral wall of the vertebral body on the AP projection. Once at this point, the needle is advanced into the middle of the vertebral body and should have a ending point similar to that for the transpedicular approach (see Fig. 321-3B and C).
Both the parapedicular and transpedicular approaches have their advantages and disadvantages. The transpedicular approach does offer more protection for the postganglionic nerve roots during passage of the needle and for the surrounding soft tissues from retrograde extravasation of cement along the needle’s path.36 However, because of its course within the pedicle, bilateral needle insertion may be required for injection of sufficient cement, with the accompanying risk associated with twice as many needle insertions as needed for the parapedicular approach. Additionally, its path within the pedicle requires the pedicle to be of sufficient width, a requirement that may make this technique less suitable above the midthoracic level.
The parapedicular approach exposes the patient to a higher risk for bleeding and pneumothorax37; however, the vertebroplasty is almost always performed through a unilateral approach. It also has no reliance on finding a suitable pedicle and can therefore be performed regardless of pedicle size or the angle at which the pedicle meets the vertebral body. This allows management of fractures that may be considered untreatable with the transpedicular approach. In our practice, with proper radiographic guidance, a transpedicular approach is usually sufficient and excellent filling can be achieved through a unilateral approach. When the size of the pedicle is small and particularly in the mid and upper thoracic spine, the needle insertion point can be at the junction of the rib head and pedicle interface, thereby allowing placement of the needle in the middle of the vertebral body while staying lateral to the medial aspect of the pedicle regardless of pedicle size.
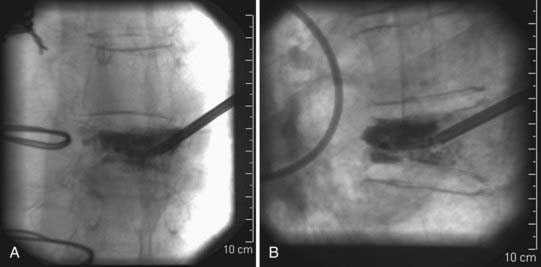
Some adjunctive techniques may allow salvage of an initially suboptimal needle trajectory. If the needle is nearing an end plate, especially when collapse of the vertebral body is severe, a beveled inner cannula can replace the initial pointed inner cannula and may help direct the needle away from the end plate that it is close to. Another helpful strategy that can be used to overcome suboptimal needle placement involves the use of a curved inner cannula for delivery of cement. This may allow administration of cement throughout the vertebral body even when the needle is not placed precisely where it was intended. The curved inner cannula may also facilitate delivery of cement directly to areas where the fractures are located (Fig. 321-4).
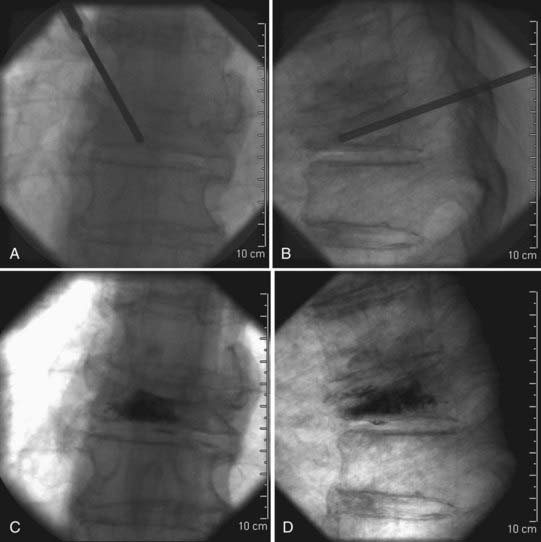
After proper placement, injection of the cement may be performed (Fig. 321-5). Some groups advocate injecting a small amount of contrast material into the vertebral body before injection of cement because it may eliminate the risk of injection into a large venous sinus.10,38 However, this risk has been shown to be negligible when vertebroplasty is performed by experienced operators, and therefore performing the procedure without an antecedent venogram may reduce contrast-related complications without a significant difference in clinical outcomes.39 The cement used for the procedure is PMMA. To fully monitor placement of the PMMA, barium sulfate is added to allow direct visualization of the cement as it is injected under fluoroscopic guidance. It is important to recognize that contrast material is often included in commercial PMMA preparations; however, it may be necessary to add additional sterile barium to the mixture. The PMMA is mixed until it reaches the consistency of toothpaste, at which time it is ready for injection. Injection should be performed under constant fluoroscopic visualization in the lateral projection and with intermittent visualization along the AP trajectory. Constant imaging on the lateral plane helps the surgeon prevent what is perhaps the most devastating potential complication of vertebral augmentation, posterior leakage with subsequent spinal cord compromise. Intermittent views in the AP plane allow monitoring to ensure that cement has not leaked out through lateral venous tributaries. We perform injections with an injector device. This places the surgeon further away from the x-ray source and facilitates AP views because the operator’s hands remain away from the x-ray field. As mentioned, injection is performed under constant lateral fluoroscopic guidance. The injector is then depressurized by turning the injector crank in the opposite direction so that the AP view can be examined. Once the cement has filled the anterior two thirds of the vertebral body, the procedure is complete. The patient is kept prone for 15 minutes to ensure that the cement has hardened sufficiently. Patients are most often discharged home on the day of the procedure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree